Common dietary supplements and cancer survivorship supplements took center stage at the Society for Integrative Oncology (SIO) 2025 Annual Meeting, where Dr. Channing Paller delivered a data-rich and pragmatic session on their role in optimizing patient outcomes. Drawing on both scientific evidence and clinical experience, she offered oncologists practical steps to safely guide their patients through supplement use and integrative care.
Background
As more cancer patients turn to supplements to manage treatment side effects and improve well-being, oncologists are increasingly asked for advice that bridges conventional care and integrative approaches. However, the safety and efficacy of many supplements remain unclear, with risks of overuse and potential drug interactions often overlooked.
At the Society for Integrative Oncology (SIO) 2025 Annual Meeting, Dr. Channing Paller from Johns Hopkins University addressed this growing need for clarity. Her talk, inspired by frequent patient questions, reviewed the most clinically relevant data on vitamins, minerals, and lifestyle interventions, aiming to help clinicians provide safe, evidence-based recommendations to their patients.
Common Dietary Supplements: Vitamin D
Dr. Paller began by emphasizing that vitamin D has the most substantial body of evidence among nutritional supplements. Chronic deficiency—found in over 50% of newly diagnosed cancer patients—can cause low calcium, muscle weakness, and an increased risk of fractures and falls, particularly in older adults.
According to the NCCN guidelines, all at-risk patients—especially those receiving androgen or estrogen deprivation therapy or living with bone metastases—should be screened and supplemented with vitamin D and calcium. Maintaining serum 25-hydroxyvitamin D levels between 30–50 ng/mL is recommended. Dr. Paller noted that vitamin D₃ is more effective than D₂ and should be taken with food containing fat for optimal absorption.
Vitamin B12 and Folate: Common, Correctable Deficiencies
Vitamin B12 deficiency affects up to 48% of patients with cancer, particularly those with gastrointestinal disease, older adults, or individuals taking proton pump inhibitors. Symptoms such as anemia, neuropathy, or fatigue may develop insidiously. Replacement options include oral, sublingual, or intramuscular forms, depending on the degree of malabsorption.
Folate deficiency—though less frequent—can result from poor diet, alcohol use, chemotherapy, or oral contraceptives. Dr. Paller highlighted that megaloblastic anemia and mucosal ulcerations are early warning signs and recommended 1 mg of folic acid daily for correction and maintenance.
Vitamin C: Dual Mechanisms and Emerging Clinical Data
Vitamin C functions as an antioxidant at low doses but may act as a pro-oxidant at high intravenous concentrations. Dr. Paller referenced recent studies examining its potential role in cancer therapy:
A 2024 Phase II trial in metastatic pancreatic cancer combined high-dose intravenous vitamin C (HDIVC) with gemcitabine and nab-paclitaxel. The study demonstrated improved progression-free survival (6.2 vs. 3.9 months) and overall survival (16 vs. 8.3 months) compared to standard care, without added toxicity.
Conversely, a randomized trial in metastatic castration-resistant prostate cancer (mCRPC) found no significant improvement when HDIVC was added to docetaxel, underscoring the need for biomarker-based patient selection in future trials.
Trace Elements: Balancing Zinc and Selenium Intake
Zinc deficiency presents with impaired taste, dermatitis, and reduced immunity. Mild deficiency can be corrected at 2–3 times the RDA (11 mg for men, 8 mg for women), but chronic intake exceeding 75 mg/day over long periods may increase the risk of aggressive prostate cancer, according to the Health Professionals Follow-Up Study.
Similarly, selenium—essential at small doses (55 µg/day)—may raise the risk of both prostate cancer and diabetes when consumed in excess, especially among men with specific genetic variants. Dr. Paller reiterated that “moderation is essential” and that supplementation should only target true deficiencies.
Curcumin and Green Tea: Promising but Not Risk-Free
Curcumin, the bioactive compound in turmeric, possesses anti-inflammatory and potential anticancer properties. It is generally recognized by the FDA as safe, even at doses of 4,000–8,000 mg/day. However, Dr. Paller cautioned that curcumin can interact with chemotherapies metabolized by cytochrome P450 enzymes (such as cyclophosphamide and doxorubicin) and has been associated with liver toxicity in some black-pepper–enhanced formulations.
Green tea extract (EGCG) also shows chemopreventive potential. Data from two Japanese studies revealed that women who consumed 3–5 cups of green tea daily had a 44% lower breast cancer recurrence rate. Yet, excessive intake (≥800 mg/day) has been linked to elevated liver enzymes and reduced efficacy of drugs like bortezomib.
Omega-3 Fatty Acids: Supporting Nutrition During Treatment
Fish-derived omega-3 fatty acids—EPA and DHA—play critical roles in inflammation control and metabolic health. While evidence is insufficient to recommend them for all patients, the ESPEN Clinical Nutrition Guidelines advise considering omega-3 supplementation in weight-losing or malnourished patients undergoing chemotherapy to maintain lean body mass and appetite.
Dr. Paller also noted that high-dose fish oil has antiplatelet properties, warranting caution in patients using anticoagulants or at risk for bleeding.
Exercise: A Proven Survival Advantage
Shifting from supplements to lifestyle, Dr. Paller underscored that physical activity remains one of the most powerful tools in survivorship. A randomized controlled trial in patients with stage I–II colon cancer showed that structured exercise significantly improved disease-free survival compared to health education alone.
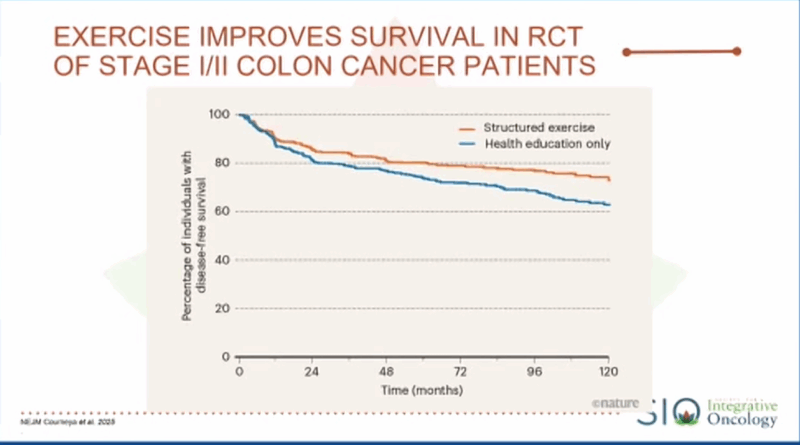
She highlighted the ASCO and SIO recommendations of at least 150 minutes of moderate or 75 minutes of vigorous exercise per week, plus 2–3 strength sessions targeting major muscle groups.
Conclusion: Safety, Moderation, and Collaboration
Dr. Paller concluded by encouraging clinicians to focus on balance and evidence. True deficiencies—such as vitamin D, B12, and folate—should be routinely screened and corrected. Over-supplementation, however, can be harmful, with risks of liver toxicity, drug interactions, and reduced treatment efficacy.
For more information clik here.