Colorectal cancer is responsible for the loss of hundreds of thousands of lives, ranking as the second leading cause of cancer-related death. According to the World Health Organization, it accounted for approximately 1.9 million new cases and over 930,000 deaths globally in 2020. These figures are expected to increase, reaching an estimated 3.2 million cases and 1.6 million deaths annually by 2040.
While the statistics are concerning, colorectal cancer is notably one of the most amenable to early detection due to its slow progression and well-defined precancerous stages. Colonoscopy plays a central role in this process, not only allowing for early detection but also enabling immediate removal of precancerous polyps. As a comprehensive screening method, colonoscopy reduces the incidence and mortality of colorectal cancer. S Zheng, Cancer (Basel), 2023.

This article provides an overview of colonoscopy – what the procedure entails, who it is recommended for, and discusses the supporting evidence for colonoscopy as a primary screening method, focusing on its effectiveness, technological advancements, and its role in long-term cancer prevention.
Understanding Colorectal Cancer
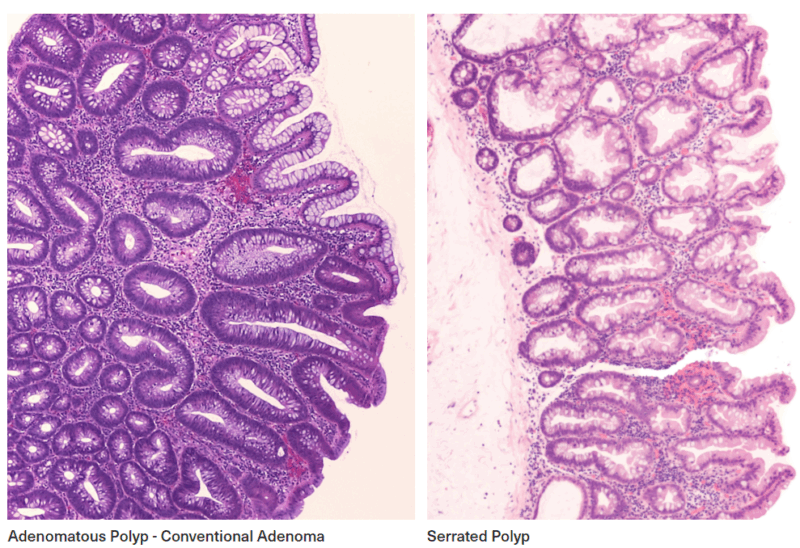
Colorectal cancer typically develops over time from benign growths (polyps) in the colon or rectum, which may gradually progress to malignancy. This is the well-established, stepwise process called adenoma-to-carcinoma sequence by which about 80% of colorectal cancers (carcinomas) develop from benign polyps (adenomas). While most cases are not inherited, some are linked to family history.
Early detection of colorectal cancer is vital, as early-stage cancers have significantly better survival rates. Many patients are asymptomatic in the early stages, making screening essential. Screening methods include stool-based tests like the faecal immunochemical test (FIT) and stool DNA, which check for hidden blood or abnormal DNA. Blood-based tests are in development. Colonoscopy, the gold standard, directly examines the colon and removes precancerous polyps when found. A Kasi, Curr Colorectal Cancer Rep, 2021. S C Liu, World J Gastroenterol, 2024.
What is a Colonoscopy and How Does It Work?
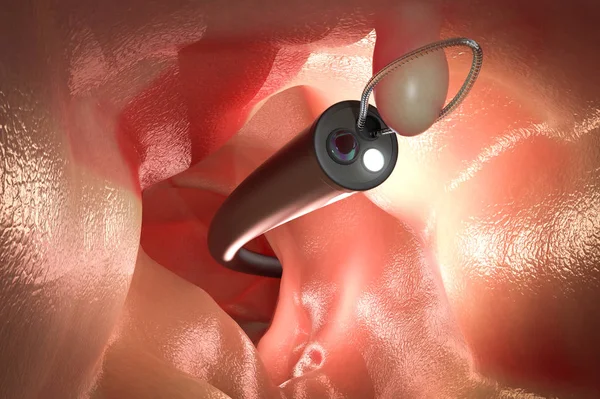
Colonoscopy uses a long, flexible tube with a light and camera (a colonoscope) inserted through the anus to examine the entire colon and rectum. This provides a full view of the large intestine, allowing for detection and removal of abnormalities such as polyps or tumors, as well as the diagnosis of non-neoplastic colon diseases. The procedure is generally safe and well-tolerated under sedation, still it does require bowel preparation and carries a small risk of complications.
Preparation for a colonoscopy typically begins 1-3 days before the procedure, with some dietary changes – patients are advised to follow a low-fiber diet and switch to clear liquids the day before. A bowel-cleansing regimen using prescribed laxatives is essential to ensure the colon is empty and clearly visible during the exam. Medication adjustments may be necessary, especially for those taking blood thinners or supplements containing iron. On the day of the procedure, patients are required to fast. After the patient receives conscious sedation or general anesthesia, the colonoscope is inserted to examine the colon. Carbon dioxide gas is used to inflate the colon, improving visibility and allowing for careful inspection of the lining.
Colonoscopy provides a real-time, direct view of the entire colon and rectum. As the scope is advanced, it transmits high-quality images to a monitor, enabling the specialist to examine the lining for polyps, inflammation, or signs of cancer. Colonoscopy detects even small lesions and allows for immediate biopsy or polyp removal.The procedure usually lasts 30-60 minutes. Afterwards, patients recover briefly before being discharged, and results are typically discussed the same day or within a few days if biopsies were taken. National Cancer Institute, NIH website, 2024. Mayo Clinic, Mayo Clinic Website, 2024.
Why Colonoscopy is a Critical Screening Tool
Colonoscopy is universally recognized as the gold standard for detecting precancerous lesions and early-stage colorectal cancers due to its ability to both detect and prevent in a single procedure. This dual diagnostic and therapeutic function offers clear clinical advantages, distinguishing colonoscopy from other screening methods. If polyps are found during the exam, they can often be removed immediately through a procedure called polypectomy, reducing the risk of progression to cancer without the need for a separate intervention. This ability to treat during screening makes colonoscopy uniquely effective in reducing cancer risk.
Compared to other screening methods, colonoscopy demonstrates higher sensitivity for advanced neoplasia – precancerous or cancerous lesions more likely to progress to colorectal cancer if left untreated, especially in asymptomatic individuals. When used as a regular screening program, colonoscopy has been associated with up to 69% reduction in colorectal cancer incidence and up to 88% reduction in mortality. And while non-invasive tests continue to evolve and play an important role, particularly in expanding access and adherence, colonoscopy remains a cornerstone of colorectal cancer prevention and early detection. I A Issa, World J Gastroenterol, 2017. D K Rex, Dig Dis Sci, 2025.
Colonoscopy provides the most complete assessment of the colon, examining the entire length from rectum to cecum and allowing for the immediate removal of polyps or biopsy of suspicious areas. In contrast, flexible sigmoidoscopy only evaluates the lower third of the colon and often misses lesions in the upper sections. CT colonography visualizes the full colon but cannot remove polyps, requiring follow-up colonoscopy if abnormalities are found. Stool-based tests, while non-invasive, detect potential signs of cancer indirectly and must be repeated frequently. Overall, colonoscopy offers the highest sensitivity and remains the most effective method for both detecting and preventing colorectal cancer. I A Issa, World J Gastroenterol, 2017. American Cancer Society, ACS website, 2025.
Beyond its clinical effectiveness, colonoscopy as a screening tool brings benefits across multiple levels – from individual care to public health. Detecting cancer at an early stage not only allows for less invasive treatment options but is also associated with higher survival rates, with a five-year survival rate approaching 89%. Increasing screening uptake could lower colorectal cancer incidence and mortality significantly, with an estimated 22% reduction in new diagnoses by 2030, while also lowering long-term healthcare costs. Centers for Disease Control and Prevention, CDC website, 2025.
Indications for Colonoscopy: When Is It Necessary?
Colonoscopy is an important tool used not only to detect cancer but also to diagnose and treat a range of other colon conditions. It is performed for various reasons, including evaluating symptoms, investigating abnormalities, and providing treatment when needed. Understanding the key indications helps guide appropriate and timely use of this procedure.
How Is Routine Screening Done?
Routine screening, as defined by established screening guidelines, applies specifically to asymptomatic individuals.
According to the American Cancer Society and the U.S. Preventive Services Task Force guidelines, individuals at average risk are advised to begin screening at age 45 now instead of 50, reflecting updated evidence on the rising incidence of colorectal cancer in younger adults. Colonoscopy is typically repeated every 10 years, and is generally advised up to age 75. For individuals aged 76 to 85, the decision to continue screening should be made in consultation with their healthcare provider, taking into account their health status and prior screening history. Screening is not recommended for those over 85.
In Europe, colonoscopy screening for colorectal cancer is part of organized, population-based screening programs primarily targeting adults aged 50 and above. Although many European countries use FIT testing as a primary screening method, several programs offer organised colonoscopy screening as a follow-up step in a two-stage process after a positive FIT test result. European Commission, European Guidelines for Quality Assurance in Colorectal Cancer Screening and Diagnosis, 2012.
Is Colonoscopy Just for Cancer Screening — or Much More?
A colonoscopy may be recommended to investigate a range of concerning symptoms that may suggest underlying colorectal pathology. These include rectal bleeding, persistent unexplained alterations in bowel habits, chronic abdominal pain, and potential signs of gastrointestinal blood loss, such as iron-deficiency anemia, fatigue, and unintentional weight loss.
Colonoscopy plays a critical role in diagnosing and managing various non-neoplastic gastrointestinal conditions. It is essential in the evaluation of inflammatory bowel disease, allowing direct visualization of mucosal inflammation, ulceration, as well as determination of the extent and severity of inflammation, and assistance in ruling out other causes of bowel symptoms. Biopsies collected during the procedure enable histological confirmation.
Being the definitive follow-up for any abnormal findings from non-invasive testing, colonoscopy is required to evaluate positive stool-based tests to identify and assess the source of bleeding or abnormal cell changes. It also confirms concerning findings from imaging studies, such as CT colonography, and further investigates abnormalities detected during sigmoidoscopy.
Beyond its diagnostic role, colonoscopy also serves as an important therapeutic tool, most notably through polypectomy, which plays a direct role in colorectal cancer prevention by interrupting the adenoma-to-carcinoma sequence. In addition, colonoscopy is used to manage gastrointestinal bleeding through epinephrine injection, thermal coagulation or metallic clip placement, as well as relieve bowel obstruction and remove foreign bodies. It also allows for symptom management in advanced disease through palliative measures. National Center for Biotechnology Information, Colonoscopy, 2022.
Colonoscopy for High-Risk Individuals
Screening guidelines distinguish a certain group of individuals as being at higher risk for colorectal cancer based on particular medical and familial factors. For those in this group, screening protocols are typically adjusted to ensure earlier detection and close monitoring of potential risks.
Having a first-degree relative diagnosed with colorectal cancer or advanced adenomas increases risk. Screening is recommended to start at age 40 or 10 years earlier than the youngest affected relative, whichever comes first. Individuals with a history of colorectal cancer, high-risk polyps, inflammatory bowel disease, such as ulcerative colitis or Crohn’s disease, as well as hereditary colorectal cancer syndromes, such as Lynch syndrome (hereditary non-polyposis colorectal cancer, HNPCC) or familial adenomatous polyposis (FAP) also require to begin screening at a younger age. Additionally, prior radiation therapy to the abdomen or pelvis for other cancers raises colorectal cancer risk, necessitating earlier and more frequent screening for these patients, too.
Colonoscopy is the most effective screening method for high-risk individuals, often beginning at age 40 or earlier, and typically performed every 5 years or more frequently with personalized intervals based on individual risk and findings. While other methods like FIT may be used, colonoscopy remains the gold standard for comprehensive prevention and monitoring for this group. C Tanadi, Rom J Intern Med, 2023.
Colonoscopy Myths vs Reality: What are the True Barriers You Need to Know?
Many people put off colonoscopy for a mix of emotional, practical and medical reasons. Common concerns include fear or anxiety about the procedure, discomfort with the bowel preparation, or embarrassment. Some believe there is no need to get screened if they have no symptoms or family history. Concerns about cost, time, and lack of awareness about its importance also contribute to low screening rates.
While these reasons are understandable, it is important to separate myth from reality and understand that most barriers can be overcome with accurate information, reassurance, and support.
Like any other medical procedure, colonoscopy does carry some risks, though serious complications are rare, occurring in only about 2 to 3 out of every 1000 procedures. Most side effects, such as bloating, cramping, or minor bleeding, are mild and temporary. More serious risks like perforation, infection, or sedation-related issues occur infrequently when proper protocols and safety standards are followed. While older adults may have a slightly higher risk due to underlying conditions, the overall benefits of colonoscopy in preventing and detecting colorectal cancer far outweigh these potential risks for the majority of patients. W Waddingham, BMJ Open Gastroenterol, 2023. C A Doubeni, Gut, 2018. M Shnell, IGIE, 2022.
However, it is important to recognize that not all colonoscopies offer the same level of effectiveness, highlighting a key factor: the quality of the procedure. A high-quality colonoscopy relies on a skilled provider, adequate time spent examining the colon, modern equipment with clear visualization, and most importantly, a well-prepped colon to ensure accurate and thorough screening. J Díaz-Tasende, Rev Esp Enferm Dig, 2022. A Hammami, Tunis Med, 2021.
Who Shouldn’t Get a Colonoscopy?
Despite its effectiveness, colonoscopy is not universally appropriate and may be contraindicated in certain clinical scenarios. It should be avoided in cases of known or suspected gastrointestinal perforation, fulminant colitis or toxic megacolon – due to the high risk of perforation from inflamed and fragile tissue, as well as after a recent myocardial infarction or hemodynamic instability, or when a patient is unable to cooperate. It may also need to be delayed after recent abdominal surgery, during active diverticulitis or acute inflammatory bowel disease flares, or in patients with severe cardiac or respiratory issues.
Additionally, colonoscopy is sometimes overused in low-risk situations: performing colonoscopy too frequently, such as for low-risk hyperplastic polyps or without a clear indication after adenoma removal or cancer resection, offers little clinical benefit and exposes patients to unnecessary risk and cost. Similarly, using colonoscopy when other screening methods would be more appropriate—or in patients for whom the risks outweigh the potential benefits—can lead to harm rather than help. J J Telford, Gastroenterol Hepatol (N Y), 2012. National Center for Biotechnology Information, Colonoscopy, 2022.
You Can Also Read Cervical Cancer Screening: Who Needs a Pap Smear or HPV Test and When? by Oncodaily
The New Era of Colonoscopy: What’s Changed for the Better?
Recent technological advancements have improved both the diagnostic accuracy of colonoscopy and patient safety. High-definition and wide-angle scopes now offer enhanced visualization, increasing the detection of flat and small polyps, while adjunct devices such as cap-assisted colonoscopy, Endocuff, and the Third Eye Retroscope help flatten mucosal folds to reveal hidden lesions. Artificial intelligence-assisted detection systems offer real-time support during procedures, helping endoscopists identify subtle or hard-to-see lesions and reducing oversight. For patients unable or unwilling to undergo traditional colonoscopy, non-invasive alternatives have expanded screening options. CT colonography (virtual colonoscopy) provides detailed imaging without the need for sedation, while capsule endoscopy allows for visualization of the colon via a swallowable camera.
These innovations, alongside the integration of quality indicators and structured screening programs, are helping to expand access, standardize care, and improve early detection outcomes across diverse populations. U Ladabaum, gastroenterology, 2020. E Seward, F1000Res, 2019. J Joseph, World J Gastroenterol, 2021.
So, Is Colonoscopy the Right Choice?
Colorectal cancer is one of the most common and deadly types of cancer, but it is also one of the most preventable. Its high fatality rates underline the importance of early detection and prevention through screening. While colonoscopy, like any other procedure, carries some risks, it remains one of the most powerful tools available to fight colorectal cancer. If there is uncertainty or concern about the procedure, healthcare providers can offer guidance to discuss the potential benefits and risks involved. In the end, timely and informed screening is one of the few critical steps within individual control – an opportunity to take charge of your health and reduce the risk of advanced disease.
Written by Seda Adibekyan
FAQ
What is a colonoscopy and why is it done?
A colonoscopy is a procedure that allows a doctor to examine the lining of your colon for abnormalities such as polyps, inflammation, or cancer. It is performed using a flexible tube with a camera and can also be used to remove polyps or take biopsies.
At what age should I start getting colonoscopy screenings?
Most guidelines recommend starting routine colonoscopy screening at age 45 for average-risk adults. Those with higher risk factors may need to start earlier
Is a colonoscopy painful or uncomfortable?
The procedure is typically performed under sedation, so most patients experience little to no discomfort and often have no memory of the procedure itself14.
How often do I need a colonoscopy?
For average-risk individuals with normal results, colonoscopy is usually recommended every 10 years. The interval may be shorter for those with risk factors or previous findings.
What should I expect during bowel preparation for a colonoscopy?
Bowel prep involves following a special diet and drinking a solution to clean out the colon. Modern preparations are more palatable and can be mixed with flavored drinks to improve taste56.
How common is colorectal cancer and who is at risk?
Colorectal cancer is the third most commonly diagnosed cancer and the third leading cause of cancer death in both men and women. Risk increases with age, but cases are rising among younger adults as well.
Can colorectal cancer be prevented or detected early?
Yes, regular screening (such as colonoscopy or stool-based tests) can detect precancerous polyps and early-stage cancers, significantly improving outcomes and survival rates
Is a colonoscopy painful or uncomfortable?
Most patients are sedated during the procedure and experience little to no pain. Many people have no memory of the procedure at all and report only mild discomfort, if any, after waking up.
Do I need a colonoscopy if I have no symptoms?
Colon polyps and early colorectal cancer often cause no symptoms. Screening is crucial for early detection and prevention, even in people without symptoms or family history
Is the bowel preparation as bad as people say?
Modern bowel preparations are more manageable than in the past. They can be split into two doses and mixed with flavored drinks to improve taste, making the process easier for most people. Tags: Colonoscopy, Colorectal Cancer Screening, Advances in Colonoscopy, Colonoscopy Risks, Preventive Medicine, Early Detection, Cancer Prevention.


