When people hear the term chemotherapy, one of the first questions that comes to mind is: What is the chemotherapy success rate?
The answer is not simple, because chemotherapy success depends on what cancer is being treated, the stage of disease, the treatment goal, and how “success” is defined.
Chemotherapy has been used in cancer care for decades and remains a cornerstone of treatment worldwide. While newer therapies such as immunotherapy and targeted drugs receive significant attention, chemotherapy continues to play a critical role—sometimes alone, often in combination, and sometimes with curative intent. Understanding what chemotherapy can realistically achieve helps patients make informed decisions and avoid misleading expectations.
This article explains how the chemotherapy success rate is measured, when chemotherapy works best, and how outcomes vary across cancers and clinical situations.
What Does “Chemotherapy Success Rate” Actually Mean?
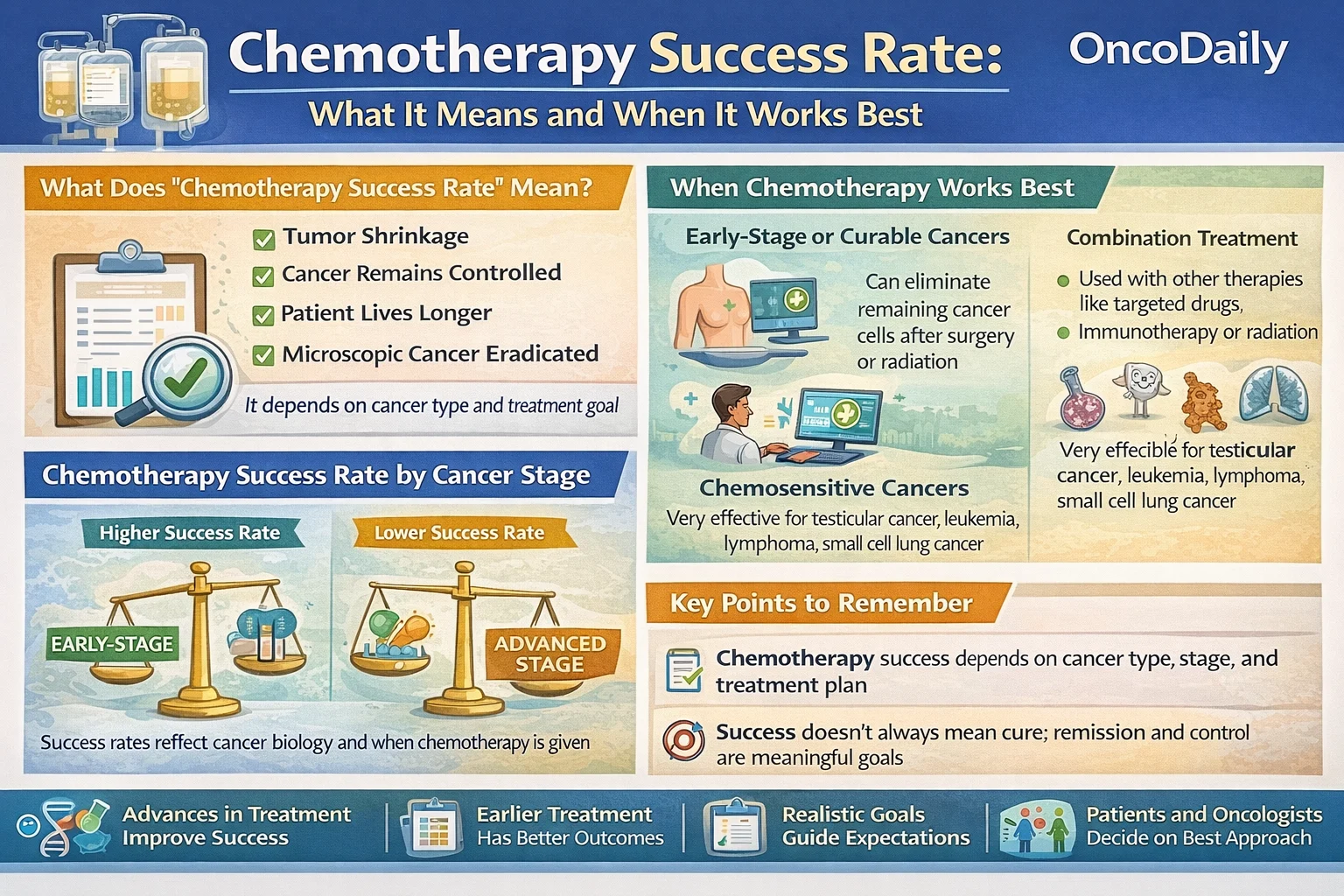
The chemotherapy success rate does not have a single universal definition. In oncology, success can mean different things depending on treatment goals.
In curative settings, success may mean eliminating all detectable cancer and preventing recurrence long term. In adjuvant therapy, chemotherapy is considered successful if it reduces the risk of cancer coming back after surgery or radiation. In advanced or metastatic cancer, success may mean shrinking tumors, slowing progression, relieving symptoms, or prolonging survival.
Clinically, chemotherapy success is often measured using endpoints such as:
- Objective response rate (ORR) – the percentage of patients whose tumors shrink by a defined amount
- Progression-free survival (PFS) – how long the cancer remains controlled
- Overall survival (OS) – how long patients live after treatment
- Pathologic complete response (pCR) – no residual cancer detected after treatment, especially in neoadjuvant settings
Because of these different endpoints, the chemotherapy success rate can appear high in some contexts and modest in others, without being misleading.
When Does Chemotherapy Work Best?
The chemotherapy success rate is highest when treatment is given early, appropriately, and for cancers that are biologically sensitive to cytotoxic drugs.
Early-Stage, Potentially Curable Cancers
Chemotherapy works best when cancer is diagnosed before widespread spread. In early-stage disease, chemotherapy may eradicate microscopic cancer cells that surgery or radiation cannot detect.
Examples include:
- Early-stage breast cancer after surgery
- Stage II–III colon cancer after tumor removal
- Testicular cancer
- Certain lymphomas and leukemias
In these settings, chemotherapy has contributed to dramatic improvements in long-term survival, with cure rates exceeding 70–90% in some cancers.
Highly Chemosensitive Cancers
Some cancers are inherently more responsive to chemotherapy due to their biology and growth patterns. These include:
- Acute leukemias
- Hodgkin lymphoma
- Testicular cancer
- Small cell lung cancer (initially)
In these diseases, the chemotherapy success rate is often high, particularly early in the disease course.
Combination and Multimodal Treatment
Chemotherapy often works best when combined with other treatments. For example:
- Chemotherapy plus surgery
- Chemotherapy plus radiation
- Chemotherapy combined with immunotherapy or targeted therapy
In many modern regimens, chemotherapy enhances the effectiveness of newer agents rather than acting alone.
Read About Immunotherapy vs Chemotherapy on OncoDaily
Chemotherapy Success Rate by Cancer Type (General Patterns)
While exact numbers vary by study and patient population, broad patterns are well established in oncology literature.
In breast cancer, chemotherapy significantly reduces recurrence risk and improves survival in high-risk early-stage disease. In hormone receptor-negative and triple-negative breast cancer, chemotherapy remains a critical component of treatment.
In colon cancer, adjuvant chemotherapy after surgery improves cure rates in stage III disease and selected high-risk stage II patients.
In lung cancer, chemotherapy improves survival in both early-stage (adjuvant) and advanced-stage disease, although success rates are higher when combined with immunotherapy.
In ovarian cancer, chemotherapy produces high initial response rates, though recurrence remains common.
In pancreatic cancer, chemotherapy improves survival but cure rates remain low, reflecting aggressive tumor biology rather than treatment failure.
These differences highlight that the chemotherapy success rate reflects cancer biology as much as drug effectiveness.
Chemotherapy in Advanced and Metastatic Cancer
In metastatic cancer, chemotherapy is usually not curative, but it can still be highly meaningful.
Here, success is measured by:
- Tumor shrinkage
- Symptom relief
- Delay of disease progression
- Extension of life
In many advanced cancers, chemotherapy adds months or years of survival, improves quality of life, and allows patients to access additional therapies over time. Importantly, a lower chemotherapy success rate in metastatic disease does not mean chemotherapy is ineffective—it means the disease is biologically more complex and resistant.
Factors That Strongly Influence Chemotherapy Success
The chemotherapy success rate is not the same for every patient. Key factors include:
Cancer Stage- Earlier stages consistently show higher success rates than advanced stages.
Tumor Biology- Aggressive or genetically complex tumors are often less responsive.
Treatment Timing- Chemotherapy given before visible progression or organ failure is more effective.
Patient Health- Good performance status allows patients to receive full-dose therapy safely.
Treatment Regimen- Modern protocols are more effective and better tolerated than older regimens.
Chemotherapy Success vs Newer Cancer Therapies
A common misconception is that chemotherapy is “outdated.” In reality, chemotherapy remains foundational.
Many immunotherapy regimens require chemotherapy to prime the immune response. Targeted therapies are often added to chemotherapy rather than replacing it. Even CAR T-cell therapy is preceded by chemotherapy to prepare the immune environment.
Rather than competing approaches, modern oncology uses chemotherapy strategically, often in combination with newer modalities to maximize success.
Real-World Success vs Clinical Trial Results
Clinical trials often report higher chemotherapy success rates than real-world practice. This difference reflects:
- Healthier trial populations
- Strict eligibility criteria
- Close monitoring and supportive care
Real-world data show slightly lower response rates but similar survival trends when treatment is applied appropriately. Understanding this gap helps patients interpret statistics realistically.
What Patients Should Take Away
The chemotherapy success rate is context-dependent, not a single number. Chemotherapy works best:
- In early-stage or curative-intent settings
- In chemosensitive cancers
- As part of combination treatment strategies
- When patients are carefully selected and supported
For many patients, chemotherapy has been and continues to be the reason long-term survival or cure is possible.
Final Perspective
Chemotherapy is not a one-size-fits-all solution, nor is it an outdated one. Its success depends on timing, biology, and treatment goals. When used appropriately, chemotherapy remains one of the most powerful tools in cancer care.
Understanding what chemotherapy success truly means allows patients to move beyond fear or oversimplified statistics and engage in informed, realistic discussions with their care teams, focused not just on numbers, but on outcomes that matter.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD