A chemotherapy port, or totally implantable venous access device (TIVAD), is a subcutaneously placed system that provides long-term central venous access for cancer patients. Typically implanted in the chest, it consists of a reservoir connected to a catheter that terminates in a central vein. These devices are widely used in oncology to safely administer chemotherapy, blood products, fluids, and parenteral nutrition while reducing peripheral vein irritation. As cancer survival improves and treatment regimens become longer and more complex, the demand for durable and reliable vascular access has increased.
This article aims to provide an updated overview of chemotherapy ports, focusing on their clinical indications, management, complications, and recent innovations, with the goal of improving care quality and patient outcomes.
Types of Long-Term Venous Access Devices in Oncology
In oncology, long-term venous access is essential for the safe and effective delivery of systemic therapies. Several types of central venous access devices are used, each with distinct characteristics and clinical applications.
- Implantable Ports (TIVADs) are completely implanted under the skin, usually in the chest, and accessed through the skin with a non-coring Huber needle. They are ideal for patients undergoing intermittent chemotherapy over extended periods, particularly those with solid tumors. Their fully internal design reduces the risk of infection and allows patients to maintain normal daily activities with minimal interference.
- Tunneled Catheters (e.g., Hickman or Broviac lines) are external catheters that exit the skin and are tunneled under the tissue to a central vein. These are more commonly used in patients with hematologic malignancies who require frequent or continuous access, such as for bone marrow transplantation or prolonged infusions. Although effective, their external components increase the risk of infection and require meticulous care.
- Peripherally Inserted Central Catheters (PICCs) are inserted through a peripheral vein, typically in the arm, and advanced into a central vein. They are less invasive to place but are associated with higher rates of thrombosis and infection, especially when used for extended durations. PICCs are often selected for shorter-term use or when other access routes are contraindicated.
Among these options, implantable ports offer the most favorable profile for long-term safety, reduced infection rates, and patient comfort, making them the preferred choice for many solid tumor patients requiring intermittent but ongoing treatment.
Clinical Indications for Chemotherapy Port Placement
Chemotherapy ports are primarily indicated in patients who require reliable, long-term central venous access for cancer treatment. One of the most common reasons for port placement is the need for prolonged chemotherapy, typically extending beyond 3 to 6 months. This is especially relevant in patients with solid tumors receiving multi-cycle regimens or maintenance therapy.
Ports are also essential for the safe administration of vesicant or irritant agents, such as anthracyclines or certain alkylating drugs, which can cause severe tissue damage if extravasated through peripheral veins. In such cases, central access ensures both efficacy and safety of drug delivery.
Another indication is poor peripheral venous access, which may result from previous chemotherapy, obesity, or underlying vascular conditions. In these patients, repeated cannulation attempts can be painful and unreliable, making a port a more sustainable option.
Chemotherapy ports are also beneficial for patients requiring frequent blood sampling or transfusions, minimizing the trauma of repeated venipuncture. Additionally, they are sometimes used in patients needing long-term parenteral nutrition or supportive care in advanced-stage malignancies.
Clinical guidelines from leading organizations such as the National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO) recommend considering port placement in patients with solid tumors who meet these criteria. These guidelines emphasize that early planning for central venous access can improve treatment adherence, reduce complications, and enhance overall patient experience.
Port Placement Procedure
The implantation of a chemotherapy port is a minor surgical procedure typically performed under local anesthesia with conscious sedation, ensuring patient comfort while maintaining safety. It is most commonly carried out in an interventional radiology suite or an operating room under sterile conditions.
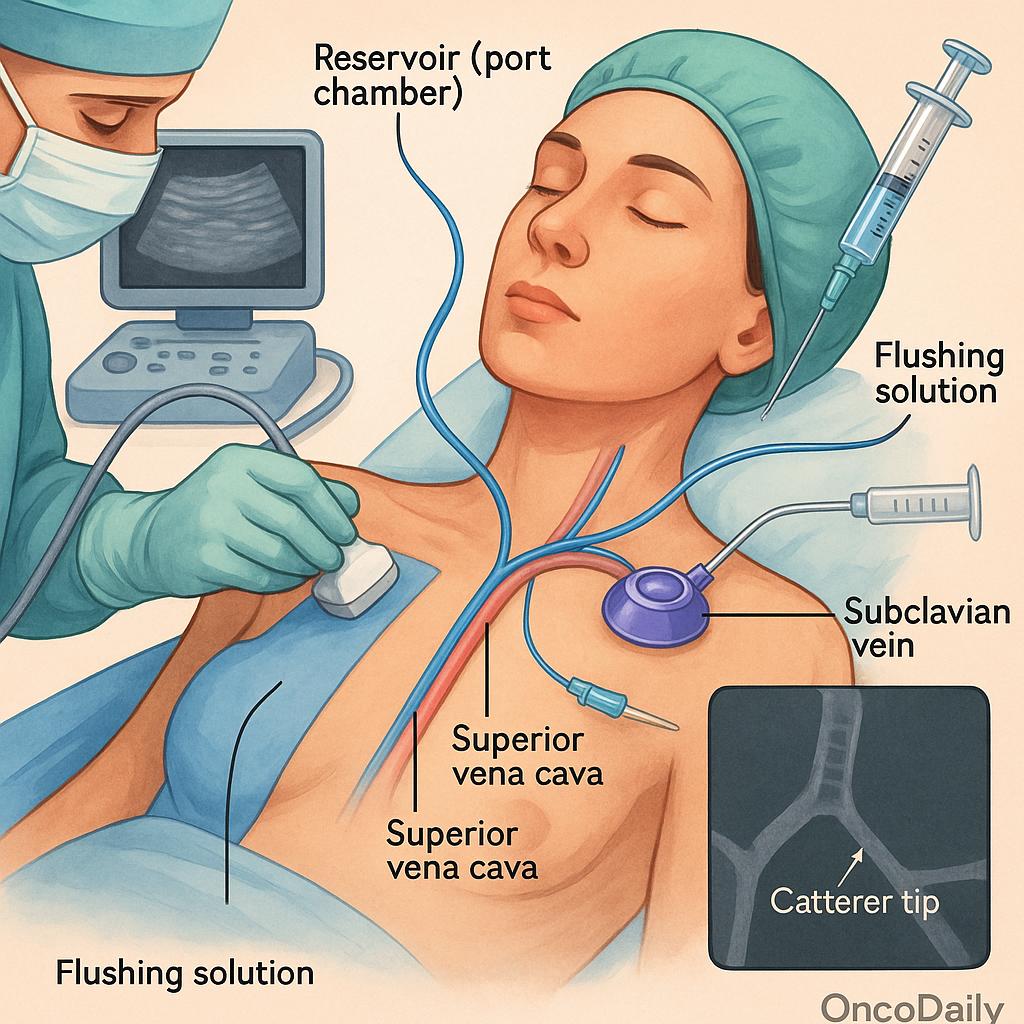
The procedure begins with the identification of a suitable central vein, most often the subclavian, internal jugular, or less commonly, the cephalic vein. Using ultrasound guidance, the vein is cannulated, and a catheter is advanced into the superior vena cava, with its tip ideally positioned near the cavoatrial junction. The other end of the catheter is tunneled subcutaneously to a reservoir (port chamber), which is placed in a surgically created subcutaneous pocket on the anterior chest wall, typically below the clavicle.
Once the catheter is connected to the port chamber, the entire system is flushed with saline or heparinized solution to ensure patency. Fluoroscopy or post-placement chest X-ray is used to confirm the correct position of the catheter tip and to exclude potential complications such as pneumothorax or catheter malposition.
After the procedure, the patient is monitored briefly and provided with specific instructions regarding wound care, port use, and signs of complications such as infection, swelling, or difficulty in flushing the device. The port site is usually allowed to heal for several days before the first use. Proper initial education and follow-up contribute significantly to the long-term functionality and safety of the device.
Materials and Design of Chemotherapy Ports
A chemotherapy port is composed of two main components: the port chamber and the catheter. The port chamber, also referred to as the reservoir, is typically made of titanium or high-grade medical plastic, designed to withstand repeated needle punctures. It is sealed with a self-sealing silicone septum, which allows for repeated access with a non-coring Huber needle while maintaining a closed, sterile system.
The catheter, which extends from the port chamber into a central vein, is made from biocompatible materials such as silicone or polyurethane. Silicone offers flexibility and softness, reducing vessel trauma, while polyurethane provides greater tensile strength and is more durable in power-injection systems.
Modern ports are designed with low-profile configurations, allowing for improved cosmetic outcomes and greater patient comfort, especially in thin individuals. Most contemporary ports are also MRI-compatible, which is essential for oncologic imaging and follow-up. Additionally, power-injectable ports have become increasingly common, enabling the safe delivery of high-pressure contrast media during CT or MRI scans, thereby eliminating the need for separate intravenous access during imaging.
Innovations such as antimicrobial-impregnated catheters and antithrombogenic coatings have been introduced to reduce the risk of infection and thrombotic complications. These advanced features may be particularly useful in immunocompromised patients or those at high risk for device-related complications.
There is variability among port manufacturers in terms of size, shape, chamber material, and compatibility with imaging and infusion protocols. These differences can influence port selection based on patient anatomy, treatment plan, and institutional preference. Understanding these nuances helps clinicians choose the most appropriate device to optimize long-term function and minimize adverse events.
Clinical Benefits of Chemotherapy Ports
Chemotherapy ports offer several critical advantages that make them the preferred choice for long-term venous access in oncology. One of the foremost benefits is the reduction in venous irritation and tissue injury, particularly when administering vesicant or irritant agents such as anthracyclines or platinum compounds. By delivering these agents directly into the central circulation, ports minimize the risk of extravasation and associated complications like skin necrosis or phlebitis, which are more common with peripheral lines.
Ports also greatly enhance patient comfort, especially in individuals with difficult peripheral access or those undergoing prolonged treatment regimens. Repeated venipunctures can lead to bruising, pain, and vein sclerosis, all of which are mitigated by the use of a subcutaneous port that allows for painless access with a non-coring needle.
Another major advantage is the reliability of central venous access for routine blood sampling, laboratory monitoring, and emergency administration of fluids, medications, or blood products. This continuity supports the timely and uninterrupted delivery of care, reducing delays in chemotherapy due to access issues.
Importantly, ports have been shown to carry lower infection rates compared to externalized catheters such as tunneled central lines or PICCs. Because the port is fully implanted beneath the skin, the risk of contamination is significantly reduced. A meta-analysis published in Supportive Care in Cancer (2021) confirmed that totally implantable ports are associated with a lower incidence of catheter-related bloodstream infections (CRBSI) and thrombosis compared to peripherally inserted central catheters (PICCs), particularly in patients receiving intermittent therapy.
Complications and Risk Management of Chemotherapy Ports
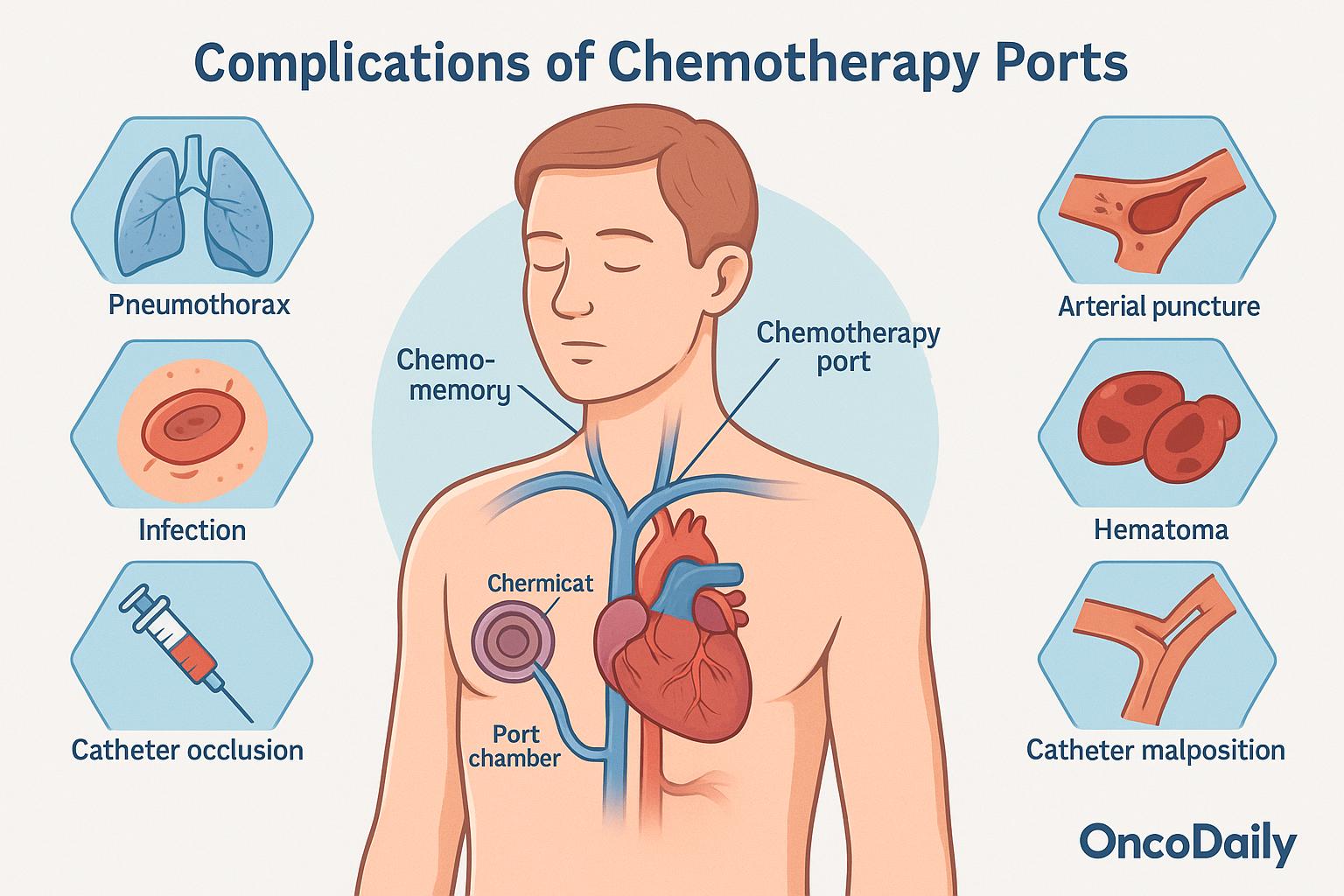
Chemotherapy ports, while generally safe and well-tolerated, can be associated with both early and late complications. Early issues typically arise during or immediately after placement and include pneumothorax, arterial puncture, hematoma, and catheter malposition. The risk of pneumothorax is relatively low, especially with the use of ultrasound guidance, but it remains a notable procedural concern. Arterial injury and hematoma formation can also occur, particularly in patients on anticoagulation, while improper catheter tip positioning may require fluoroscopic adjustment.
Late complications tend to emerge during ongoing use. Infection is one of the most significant risks, though rates of catheter-related bloodstream infections (CRBSI) are lower with ports than with external catheters, estimated at 0.1 to 0.3 per 1,000 catheter-days in large cohort studies. Thrombosis is another frequent concern, affecting approximately 3–5% of patients, and can lead to impaired flow or necessitate device removal. Catheter occlusion, often due to fibrin sheath formation or drug precipitation, may compromise function, while mechanical problems such as port rotation or extrusion are more likely in underweight or elderly patients.
To reduce these risks, strict aseptic technique during every access is essential. Regular flushing with saline or heparin maintains patency and prevents occlusion, particularly when the port is not in continuous use. The application of antimicrobial dressings and skin antisepsis further lowers infection risk in vulnerable patients. Although prophylactic anticoagulation has been investigated, recent studies have not shown a clear benefit in routine use, and it is typically reserved for those at high thrombotic risk. With appropriate care, the incidence of serious complications remains low, making ports a safe and effective option for long-term vascular access in oncology.
Standards of Chemotherapy Port Care
The proper care and maintenance of chemotherapy ports are essential to ensure their long-term function, reduce complications, and support uninterrupted cancer treatment. Port care protocols are standardized across most institutions and are informed by evidence-based guidelines, including those from the Oncology Nursing Society (ONS) and the Centers for Disease Control and Prevention (CDC).
Accessing the port is performed using a non-coring Huber needle, which is specifically designed to preserve the integrity of the silicone septum and minimize leakage or damage. Each access must be conducted using strict sterile technique, including thorough hand hygiene, the use of sterile gloves, and skin preparation with an appropriate antiseptic agent—typically chlorhexidine gluconate. This reduces the risk of catheter-related infections, which can compromise the device and the patient’s overall health.
Routine flushing protocols are crucial to prevent catheter occlusion. According to ONS recommendations, ports should be flushed with normal saline or heparinized saline after each use, and at least every 4 to 6 weeks when not in active use. This maintains catheter patency and prevents fibrin buildup or clot formation. Some institutions prefer saline-only flushing based on updated infection control policies and manufacturer instructions for specific port models.
Dressing changes are required when the port is accessed and typically occur every 7 days using sterile, transparent semipermeable dressings unless soiled or loose. During each dressing change, the site should be carefully inspected for signs of infection, including redness, swelling, tenderness, or discharge, as well as for any signs of mechanical complications such as skin breakdown, port rotation, or dehiscence.
Equally important is the education of nursing staff and patients. Nurses must be trained in evidence-based port care techniques, access procedures, and early detection of complications. Patients should receive clear instructions on how to monitor their port site, recognize symptoms of infection or malfunction, and when to seek medical attention. Education empowers patients and caregivers to participate actively in the care process and helps prevent delays in diagnosis or treatment.
Indications and Procedure for Chemotherapy Port Removal
The removal of a chemotherapy port is typically indicated when the device is no longer clinically necessary or when complications arise that cannot be resolved through conservative measures. One of the most common reasons for removal is the completion of chemotherapy, particularly in patients who are in remission or no longer require ongoing intravenous treatment. In such cases, removing the port avoids the risks associated with maintaining an unused central venous device.
Another indication is infection, especially when it involves the port chamber or catheter and is unresponsive to systemic antibiotics. Persistent or recurrent catheter-related bloodstream infections often necessitate prompt port removal to prevent sepsis and other systemic complications.
Ports may also require removal due to mechanical failure, such as catheter fracture, occlusion that cannot be cleared with thrombolytics, or port chamber rotation or extrusion. In these situations, the port is no longer functional or safe for use. Additionally, in patients who are transitioning to palliative or hospice care, the port may be removed if it is no longer required for treatment or symptom management, particularly if it becomes a source of discomfort or infection risk.
Port removal is generally a minor surgical procedure performed under local anesthesia with or without light sedation. It involves reopening the original incision, dissecting around the port chamber, and gently withdrawing the catheter from the central vein. Most removals are uncomplicated, but risks include bleeding, infection, and in rare cases, retained catheter fragments, especially if the catheter is damaged or adherent to the vessel wall. If a fragment remains intravascularly, it may require interventional radiologic retrieval or monitoring depending on its location and associated risk.
Recent Developments and Innovations in Chemotherapy Ports
In recent years, significant advancements have been made in the design, functionality, and safety of chemotherapy ports, reflecting ongoing efforts to improve patient outcomes and reduce complications associated with long-term central venous access. These innovations span both materials science and procedural technologies, offering a more personalized and precise approach to vascular access in oncology.
One important area of development has been the introduction of antimicrobial and heparin-coated catheters. These surface modifications aim to reduce the risk of catheter-related infections and thrombotic events by preventing biofilm formation and inhibiting platelet adhesion. Clinical studies, including data from multicenter registries, have shown that such coatings may lower the incidence of catheter-related bloodstream infections, particularly in high-risk or immunocompromised cancer populations. These coated devices are increasingly being integrated into routine care in settings where infection prevention is paramount.
Another major innovation is the widespread availability of power-injectable ports, which are designed to withstand the high pressures used during contrast-enhanced imaging studies such as CT or MRI scans. These ports eliminate the need for peripheral IV placement during imaging, thereby enhancing patient comfort and reducing the risk of extravasation. Both the NCCN and ESMO guidelines acknowledge the utility of power-injectable ports, especially in patients undergoing frequent imaging for cancer staging or treatment response assessment.
Advancements in placement techniques have also emerged, most notably with the adoption of 3D navigation and ultrasound-guided vascular access systems. These technologies enable more precise catheter tip positioning and reduce the risk of malposition, arterial puncture, and other procedural complications. Such approaches are particularly beneficial in patients with distorted anatomy, prior central line placements, or radiation-induced changes in vascular structures.
Looking to the future, ongoing research is exploring the use of biodegradable materials for temporary venous access, which could potentially reduce the need for surgical removal in select cases. In parallel, nanotechnology-based surface coatings are being investigated for their ability to confer antimicrobial and antithrombotic properties without compromising biocompatibility or flexibility. Perhaps most novel is the development of wireless, sensor-embedded port systems capable of real-time monitoring for early signs of occlusion, infection, or mechanical malfunction. These smart ports, still in experimental phases, may offer a transformative shift in the way vascular access is managed, allowing for predictive maintenance and personalized care.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is a chemotherapy port?
A chemotherapy port is a small device implanted under the skin to provide long-term central venous access for administering chemotherapy and other treatments.
Who needs a chemotherapy port?
Patients undergoing long-term chemotherapy, receiving vesicant drugs, or those with poor peripheral veins often benefit from port placement.
How is a chemotherapy port implanted?
The port is surgically inserted under the skin and connected to a central vein, usually in the chest, under local anesthesia with sedation.
What are the types of central venous access devices?
Common devices include implantable ports (TIVADs), tunneled catheters (e.g., Hickman), and PICC lines—each suited for different clinical needs.
How do I care for my chemotherapy port?
Routine flushing, sterile access, and regular monitoring by trained nurses are essential to prevent infection or blockage.
What are common complications of chemotherapy ports?
Infections, thrombosis, catheter occlusion, and mechanical failure are possible but infrequent with proper care.
When is a port removed?
Ports are removed after treatment completion or if complications arise that cannot be resolved conservatively.
Are chemotherapy ports safe for imaging scans?
Many modern ports are power-injectable and MRI-compatible, making them safe for use during CT or MRI with contrast.
What are the latest innovations in port design?
Innovations include antimicrobial coatings, power-injectable designs, smart ports with sensors, and more precise placement techniques.
Is a port better than a PICC line or tunneled catheter?
For long-term, intermittent chemotherapy, ports are preferred due to lower infection risk and improved patient comfort.