Pancreatic Cancer
Pancreatic cancer is a cancer originating from the pancreas. The pancreas is an organ located in the abdomen, near the stomach and small bowel (small intestine). The pancreas releases natural chemicals called enzymes into the small bowel that help digest food. It also releases hormones, including insulin, into the bloodstream, to help convert food into energy. Cancer occurs when cells in the pancreas grow in an uncontrolled way. Most pancreatic cancers start in the cells of ducts of the pancreas (called exocrine pancreatic cancer). Cancer can also start in the hormone-producing cells of the pancreas (called pancreatic neuroendocrine tumors).
Prevalence and Epidemiology
Pancreatic cancer is the 10th most common cancer in the United States, accounting for approximately 3% of all new cancer cases. In 2024, it is estimated that there will be around 62,000 new cases of pancreatic cancer diagnosed in the United States and approximately 49,000 deaths from the disease. The incidence of pancreatic cancer is slightly higher in men compared to women, with a male-to-female ratio of approximately 1.3:1.
Pancreatic cancer incidence increases significantly with age, with nearly 90% of cases diagnosed after age 55. The incidence of pancreatic cancer has been steadily increasing over the past few decades, and it is projected to become the second leading cause of cancer-related deaths in the United States by 2030. This trend is likely due to the increasing prevalence of risk factors such as obesity, type 2 diabetes, and an aging population.
Causes and Risk Factors
Risk Factors and Causes
Pancreatic cancer is a complex disease with both non-modifiable and modifiable risk factors.
The non-modifiable risk factors include:
- Age – Pancreatic cancer is primarily a disease of older adults, with approximately 90% of newly diagnosed patients being over the age of 55. The incidence increases significantly after age 60, and the median age at diagnosis is 72 years.
- Family History and Genetics – About 10% of pancreatic cancers are thought to have a hereditary component. Individuals with a first-degree relative (parent, sibling, or child) with pancreatic cancer have an approximately 2- to 3-fold increased risk of developing the disease. Certain inherited genetic syndromes, such as Lynch syndrome, familial atypical multiple mole melanoma (FAMMM) syndrome, and hereditary breast and ovarian cancer (BRCA1/2) syndromes, are also associated with an increased risk of pancreatic cancer.
- Sex – Pancreatic cancer is slightly more common in men than in women, with a male-to-female ratio of approximately 1.3:1.
- Race/Ethnicity – Pancreatic cancer incidence is higher in African Americans compared to other racial/ethnic groups in the United States.
- Blood Type – Individuals with blood type A, AB, or B have a slightly higher risk of developing pancreatic cancer compared to those with blood type O.
The modifiable risk factors for pancreatic cancer include:
- Smoking – Smoking is a well-established risk factor for pancreatic cancer, with smokers having a 2- to 3-fold increased risk compared to non-smokers. The risk decreases after smoking cessation, but it may take several years for the risk to return to that of a non-smoker.
- Obesity and Diabetes – Obesity, particularly abdominal obesity, and type 2 diabetes are associated with an increased risk of pancreatic cancer. The risk is even higher in individuals with both obesity and diabetes.
- Chronic Pancreatitis – Chronic inflammation of the pancreas, known as chronic pancreatitis, is a risk factor for pancreatic cancer. The risk is particularly high in individuals with hereditary or autoimmune forms of chronic pancreatitis.
- Dietary Factors – A diet high in red and processed meats, as well as a diet low in fruits and vegetables, may be associated with an increased risk of cancer.
- Alcohol Consumption – Heavy, long-term alcohol consumption has been linked to an increased risk of pancreatic cancer, particularly in individuals with chronic pancreatitis.
Symptoms
Early-stage pancreatic cancer often does not cause any specific symptoms, making it difficult to detect early.
The most common symptoms of pancreatic cancer include:
- Jaundice (yellowing of the skin and eyes)
- Abdominal or back pain
- Unexplained weight loss
- Loss of appetite
- Nausea and vomiting
- Diarrhea
- Fatigue
- Newly diagnosed diabetes or worsening of existing diabetes
A tumor’s location in the pancreas can impact the specific symptoms experienced. Tumors in the head of the pancreas are more likely to cause jaundice and pale stools (due to tumor mass effect, and compression of bile ducts), while tumors in the body or tail may cause more abdominal or back pain.
Symptoms of metastatic or advanced pancreatic cancer can include additional issues related to the spread of the cancer, such as liver dysfunction, lung problems, and bone pain.
The symptoms of pancreatic cancer can be vague and similar to those of other gastrointestinal conditions, which can delay diagnosis.
Patients are advised to report any new or worsening symptoms to their healthcare provider, as early detection is crucial for improving outcomes.
 Pancreatic Cancer: Symptoms. This image is taken from gicancer.org.
Pancreatic Cancer: Symptoms. This image is taken from gicancer.org.
Diagnosis and Types
Diagnosis
Diagnosing pancreatic cancer can be challenging, as the disease often does not cause specific symptoms until it has progressed.
The diagnostic process typically involves a combination of the following:
- Physical examination and medical history review
- Imaging tests such as CT scans, MRI, endoscopic ultrasound, and PET scans to visualize the pancreas and look for tumors
- Blood tests to measure tumor markers like CA 19-9
- Biopsy, either through fine-needle aspiration or endoscopic procedures, to obtain a tissue sample for analysis
- The biopsy is considered the most definitive way to diagnose pancreatic cancer, but it can be challenging due to the location of the pancreas and the diffuse nature of some tumors.
- Genetic and molecular testing of the tumor sample may also be performed to guide treatment decisions, such as identifying mutations in genes like BRCA or KRAS.
- Staging cancer, based on the size of the tumor, the extent of local and regional spread, and presence of distant metastases, is a crucial part of the diagnostic process to determine prognosis and guide treatment planning
Timely and accurate diagnosis is essential, as pancreatic cancer is often diagnosed at an advanced stage when the prognosis is poor. Referral to a specialized medical center with experience in pancreatic cancer is recommended.
Types
There are two main types of pancreatic cancer:
Exocrine Pancreatic Cancers
This group accounts for about 95% of pancreatic cancers. The most common type is pancreatic adenocarcinoma, making up around 85% of cases. It arises from the exocrine cells that produce digestive enzymes. Other less common exocrine cancers include adenosquamous carcinomas, squamous cell carcinomas, acinar cell carcinomas, and others.
Pancreatic Neuroendocrine Tumors (PNETs)
These account for about 5-7% of pancreatic cancers and arise from the hormone-producing endocrine cells. PNETs can be functioning (producing hormones like insulin, glucagon, etc.) or non-functioning. Specific types are named based on the hormone produced, such as insulinomas, glucagonomas, gastrinomas, etc.
Some key differences:
- Exocrine cancers are far more common but more aggressive.
- PNETs are less common but tend to be less aggressive.
- They differ in symptoms, diagnostic tests, treatment, and prognosis due to their distinct origins.
Screening and Early Detection
Due to the lack of early symptoms and the difficulty in detecting pancreatic cancer at an early stage, screening for the disease is an area of active research and debate. Currently, there are no widely accepted screening programs for the general population, as the benefits of screening have not been demonstrated. However, screening may be recommended for individuals at high risk of developing pancreatic cancer, such as those with a strong family history or certain genetic syndromes. Potential screening approaches being investigated include:
- Imaging tests, such as MRI or endoscopic ultrasound, performed annually or every few years
- Blood-based biomarker tests that could detect early signs of pancreatic cancer
- Genetic testing to identify individuals with inherited genetic variants that increase the risk of pancreatic cancer
While these screening methods show promise, more research is needed to determine their effectiveness in detecting pancreatic cancer at an early, potentially curable stage. Healthcare providers and patients should discuss the potential benefits and risks of screening, especially for those at high risk of the disease.
Treatment
Surgery
Surgery remains the only potentially curative treatment for pancreatic cancer, but only about 15-20% of patients have resectable disease at diagnosis. The most common surgical procedures are:
- Whipple procedure (pancreaticoduodenectomy) for tumors in the head of the pancreas
- Distal pancreatectomy for tumors in the body or tail of the pancreas
- Total pancreatectomy for large or multifocal tumors
5-year survival rates after surgery range from 10-25%, with a median survival of 12-20 months. Postoperative complications occur in up to 40% of patients.
Neoadjuvant Therapy
Neoadjuvant chemotherapy or chemoradiation is increasingly used to try to shrink borderline resectable tumors and increase the chance of complete surgical resection. This approach is associated with a higher rate of margin-negative resections and improved survival compared to upfront surgery.
Adjuvant Therapy
Adjuvant chemotherapy, typically with gemcitabine or 5-FU-based regimens, is recommended after surgery to eradicate micrometastatic disease and improve survival. Adjuvant chemoradiation may also be considered for patients with positive margins or lymph nodes.
Locally Advanced Disease
For patients with locally advanced, unresectable disease, the goals of treatment are to control local symptoms and prolong survival. Options include:
- Chemotherapy with regimens like FOLFIRINOX or gemcitabine/nab-paclitaxel, which can achieve a median survival of 11-15 months
- Chemoradiation, which may provide better local control but has not been shown to improve overall survival compared to chemotherapy alone
Metastatic Disease
Patients with metastatic pancreatic cancer have a very poor prognosis, with a median survival of only 6-11 months with chemotherapy. Treatment options include:
- Chemotherapy with FOLFIRINOX or gemcitabine/nab-paclitaxel, which can improve survival and quality of life compared to gemcitabine alone
- Palliative radiation for symptomatic metastases
- Targeted therapies like PARP inhibitors for tumors with BRCA mutations
- Immunotherapy for tumors with high microsatellite instability or mismatch repair deficiency
Emerging Therapies
Novel approaches under investigation include:
- Tumor-treating fields, which use alternating electric fields to disrupt cell division
- Oncolytic viruses that selectively infect and lyse tumor cells
- Combination therapies with immunotherapy, targeted agents, and/or chemotherapy
In summary, while pancreatic cancer remains a challenging disease to treat, ongoing research is exploring new surgical techniques, neoadjuvant and adjuvant therapies, targeted agents, and immunotherapies to improve outcomes. Multidisciplinary care at high-volume centers is crucial for optimizing treatment and survival.
Prognosis and Survival
Pancreatic cancer has an extremely poor prognosis and low survival rates compared to other cancers. The overall 5-year relative survival rate is only around 12% in the United States. However, survival varies significantly based on the stage at diagnosis. If diagnosed at an early stage when surgical removal is possible, the 5-year survival rate is 44%. Unfortunately, only about 12% of cases are diagnosed at this early stage. For locally advanced cases where the cancer has spread to surrounding tissues (stage 3), the 5-year survival rate drops to 15%. In the majority (52%) of cases where the cancer has metastasized to distant organs at diagnosis, the 5-year survival is a dismal 3%.
Several factors have been identified as independent predictors of poor prognosis, including:
Tumor Factors
- Higher tumor grade and stage correlate with worse prognosis.
- Tumor size >3cm is associated with lower survival rates.
- Certain molecular subtypes like squamous have a worse prognosis.
Patient Factors
- Older age at diagnosis portends a poorer outcome.
- Better performance status and lack of significant weight loss correlate with improved survival.
- The presence of diabetes mellitus may worsen the prognosis.
Biomarkers
- High pretreatment CA19-9 levels are linked to worse survival.
- Other adverse prognostic biomarkers include high neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, and low albumin levels.
Treatment Factors
- Patients who undergo surgical resection have significantly better outcomes than unresectable cases.
- Adjuvant (post-surgery) chemotherapy improves survival compared to surgery alone.
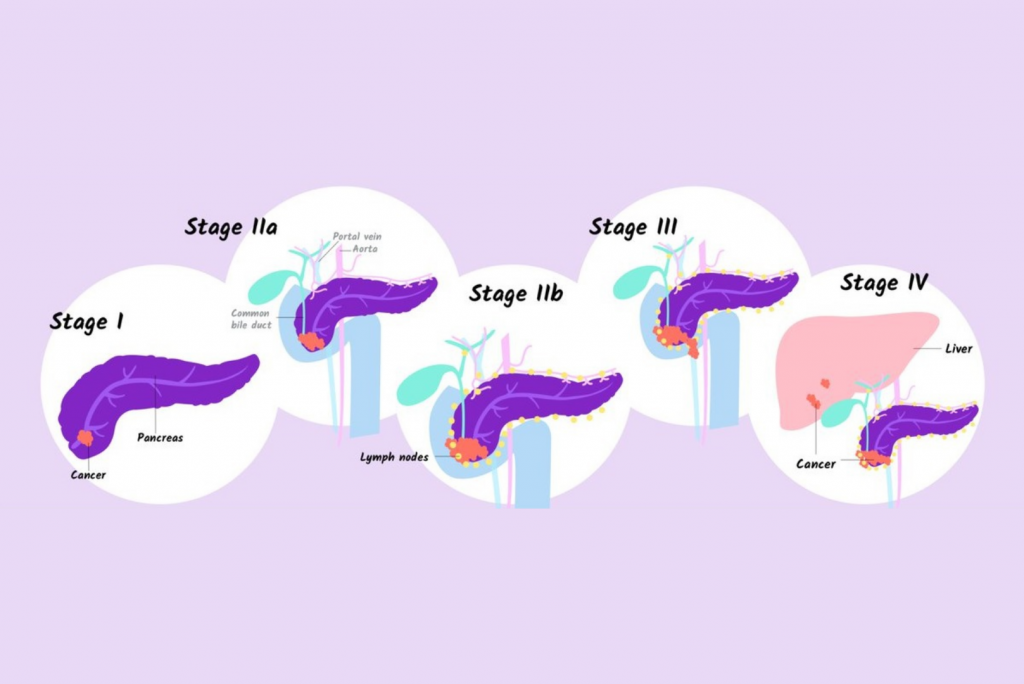
Stages of pancreatic cancer. This image is taken from regencymedicalcentre.com.
Patient’s Survivorship
While pancreatic cancer survivorship remains extremely low overall, understanding the factors associated with long-term survival and providing comprehensive survivorship care is important for optimally supporting the unique needs of this patient population. Pancreatic cancer survivors face significant physical, emotional, and practical challenges given the aggressive nature of the disease and the high risk of recurrence.
Key issues they may encounter include fear of cancer recurrence, long-term effects from treatments like surgery, chemotherapy and radiation, sexual health concerns, financial toxicity from the high costs of care, and lack of structured survivorship care planning. Survivorship care plans can help coordinate follow-up care, surveillance for recurrence, management of late treatment effects, and psychosocial support services tailored to pancreatic cancer survivors. A multidisciplinary approach involving oncologists, primary care providers, nurses, psychologists, social workers and others is crucial for delivering comprehensive survivorship care.
Problems During Treatment
Pain Management
- Pancreatic cancer patients often experience severe pain, which can impact their quality of life and ability to undergo treatment.
- Effective pain management strategies include opioid analgesics, nerve blocks, celiac plexus neurolysis, and integrative therapies like acupuncture.
- Early involvement of a palliative care team is recommended for comprehensive pain management.
Malnutrition and Exocrine Pancreatic Insufficiency (PEI)
- PEI, or inability to properly digest food due to lack of pancreatic enzymes, is common in pancreatic cancer patients.
- This can lead to malnutrition, weight loss, and impaired treatment tolerance.
- Pancreatic enzyme replacement therapy and nutritional support are crucial for managing PEI and preventing malnutrition.
- However, studies show PEI is often underdiagnosed and undertreated by clinicians.
Elderly Patient Population and Treatment Ineligibility
- Cancer predominantly affects the elderly, many of whom are ineligible for aggressive treatments like surgery due to comorbidities.
- Tailored treatment approaches and supportive care are needed for this patient population.
Lack of Early Detection and Screening
- The absence of effective screening methods leads to late-stage diagnosis when the cancer is often unresectable or metastatic.
- This limits curative treatment options and contributes to the poor prognosis.
- Ongoing research aims to develop better early detection and screening strategies.
Treatment Resistance and Limited Therapeutic Options
- This cancer is inherently resistant to many treatments, with few long-term survivors among metastatic cases.
- New targeted therapies, immunotherapies, and combination regimens are being explored to improve outcomes.
After treatment
Emotional Challenges
- Dealing with difficult emotions like sadness, anxiety, fear, or anger after treatment completion.
- Manage by seeking counseling, joining support groups, or speaking with a social worker to develop coping strategies.
- Connect with other pancreatic cancer survivors for peer support.
Fear of Cancer Recurrence
- Worry and anxiety about the cancer returning are common after treatment.
- Discuss this fear openly with the healthcare team.
- Maintain regular follow-up visits and surveillance as recommended.
Long-Term Side Effects
- Pancreatic cancer treatments like surgery, chemotherapy, and radiation can cause lasting side effects.
- Manage side effects like pain, fatigue, and digestive issues through medications, lifestyle changes, or palliative care as needed.
Financial Toxicity
- The high costs of cancer treatment can lead to financial strain and distress.
- Explore financial assistance options from government programs, non-profits, and pharmaceutical companies.
- Speak to a financial counselor/navigator about managing expenses.
Nutritional Challenges
- Pancreatic enzyme insufficiency and malnutrition are common due to the nature of the disease.
- Pancreatic enzyme replacement therapy and nutritional support can help manage these issues.
Survivorship Care Plan
- Lack of a structured follow-up plan after active treatment completion.
- Work with the oncology team to develop a comprehensive survivorship care plan covering surveillance, management of late effects, healthy lifestyle recommendations, and psychosocial support.
Utilizing a multidisciplinary team involving oncologists, nurses, dietitians, social workers, psychologists, and financial counselors can help pancreatic cancer survivors comprehensively address the various challenges they may face after treatment completion.
Recommendations for Patients
Post-Surgical Care
- Follow instructions on proper medication usage, diet, and oral hygiene practices provided by the dental/medical team.
- Be aware of potential complications like bleeding, swelling, etc. and know when to seek urgent medical attention.
- Attend scheduled follow-up appointments for monitoring of healing and removal of any sutures.
Managing Bleeding/Swelling
- Apply firm, continuous pressure with gauze on the surgical area if bleeding occurs. Change gauze hourly.
- Use ice packs (15 minutes on, 15 minutes off) on the face near the surgical site for the first 24 hours to reduce swelling.
- Keep head elevated, even while sleeping, to help minimize swelling.
Diet
- Start with soft, liquid or pureed foods once anesthesia wears off. Avoid hard, crunchy foods that could get lodged in the surgical site.
- Gradually transition to a normal, healthy diet as healing progresses.
- Focus on nutrient-dense foods like fruits, vegetables, whole grains, and lean proteins to aid recovery.
Lifestyle
- Avoid alcohol and smoking, as they can impair healing.
- Engage in light physical activity as tolerated, but check with the medical team before resuming exercise.
- Maintain a healthy weight through a balanced diet and regular activity.
Emotional Well-being
- Expect to experience a range of emotions. Seek support from counselors or support groups as needed.
- Discuss any fears, like cancer recurrence, openly with the healthcare team.
Long-Term Care
- Follow the survivorship care plan provided for managing late effects, surveillance, and healthy lifestyle recommendations.
- Attend all recommended follow-up appointments for monitoring.
The key is to closely follow post-operative instructions, maintain a nutritious diet, engage in healthy lifestyle practices, address emotional needs, and adhere to long-term follow-up care for optimal recovery and management of late effects.
Watch Eric’s story who was diagnosed with stage 3 pancreatic cancer.
Conclusion
While pancreatic cancer carries a notoriously poor prognosis, there exists a subset of exceptional patients who defy the odds and achieve long-term survival. Factors like younger age, early detection, well-differentiated tumors, and aggressive multimodal treatment have enabled some to survive long-term against this devastating disease. Intriguingly, certain racial/ethnic groups also experience higher rates of long-term survival, suggesting potential biological differences. Each remarkable long-term survivor serves as a beacon of hope and inspiration for others battling cancer. With continued research into the factors driving exceptional responses, the future outlook for this malignancy may gradually improve over time.
References
- Pancreatic Cancer Review – PubMed
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research UK – cancerresearchuk.org
- MD Anderson Cancer Center – mdanderson.org
- Patients with Pancreatic Ductal Adenocarcinoma – PubMed
- Screening of pancreatic cancer – PubMed
- Pancreatic Cancer: Challenges and Opportunities in Locoregional Therapies – PubMed
- Association of Cancer Care Centers – accc-cancer.org
- World Journal of Surgical Oncology – wjso.biomedcentral.com
- Congressionally Directed Medical Research Programs – cdmrp.health.mil
- UC San Diego Health Clinical Trials – clinicaltrials.ucsd.edu
- University of California San Francisco – clinicaltrials.ucsf.edu
- John Hopkins Medicine – hopkinsmedicine.org
- Diagnosis and management of pancreatic cancer – PubMed
- National Cancer Institute – cancer.gov
- American Cancer Society – cancer.org