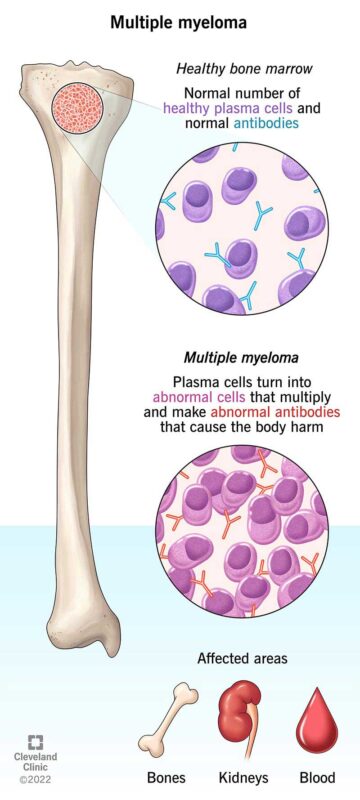
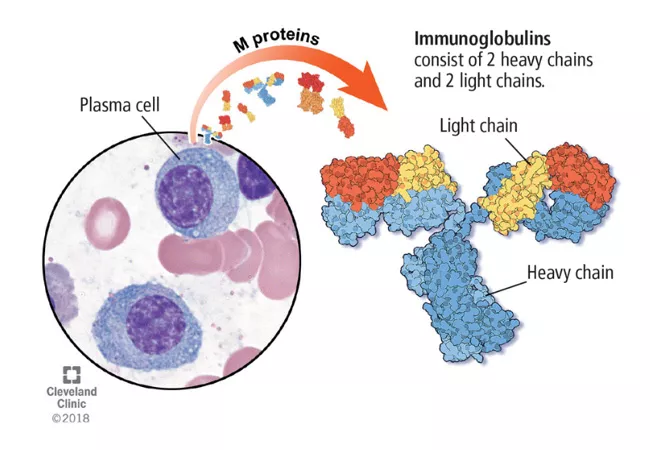
Multiple myeloma is a cancer of plasma cells, a type of white blood cell found in the bone marrow. These abnormal cells multiply uncontrollably, crowding out healthy blood cells and producing harmful proteins that can damage organs, weaken bones, and impair immune function.
Understanding its symptoms, stages, and treatment options is essential for early detection and better outcomes. This article will explore the causes, symptoms, diagnosis, staging, and treatment options, incorporating data from clinical studies and expert opinions to provide a comprehensive overview of this complex disease.
What Are the Symptoms of Multiple Myeloma?
Multiple myeloma manifests through various symptoms, with prevalence rates varying among patients. A comprehensive meta-analysis by Boland et al., published in the European Journal of Haematology, examined 36 studies encompassing 3,023 multiple myeloma patients to determine symptom prevalence. The study reported the following findings:
- Fatigue: The most prevalent symptom, affecting approximately 98.8% of patients (95% CI: 98.1–99.2%).
- Pain: Experienced by about 73% of patients (range: 39.9–91.7%), with bone pain, particularly in the spine and ribs, being a common manifestation.
- Constipation: Reported by 65.2% of patients (range: 22.9–92.2%).
- Tingling in Hands/Feet (Peripheral Neuropathy): Observed in 53.4% of patients (range: 0.4–99.7%).
These findings underscore the high prevalence of fatigue and pain among multiple myeloma patients, highlighting the importance of symptom management in this population.
What Are the Causes and Risk Factors for Multiple Myeloma?
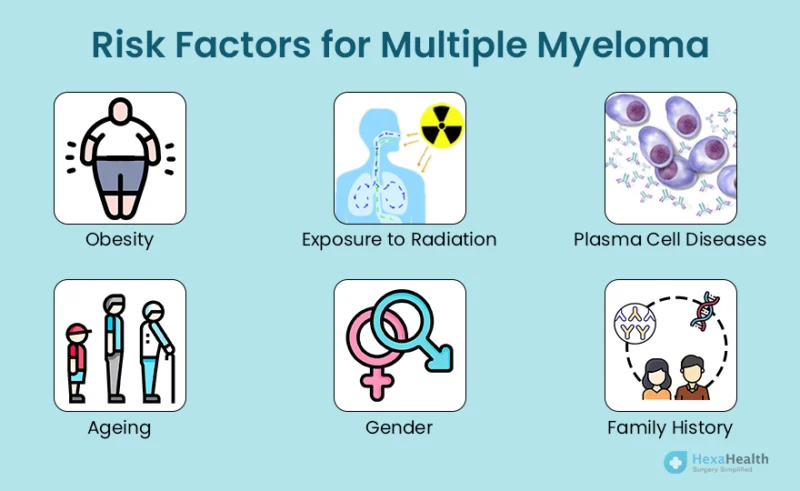
Multiple myeloma is a complex disease with several identified risk factors:
- Age: The likelihood of developing multiple myeloma increases with age. According to the American Cancer Society, most individuals diagnosed are over 65 years old. The first author of this information is Alexander DD.
- Race: African Americans have more than twice the incidence rate of multiple myeloma compared to white Americans. The reasons for this disparity remain unclear.
- Family History: A familial predisposition exists; having a sibling or parent with multiple myeloma increases one’s risk. However, most patients do not have affected relatives.
- Obesity: Excess body weight has been linked to a higher risk of developing multiple myeloma. Research indicates that with each increase in body mass index (BMI) by five units, the relative risk rises by 11%. This finding is discussed in the Annual Review of Medicine, authored by Calle EE.
- Environmental Exposures: Occupational exposure to certain chemicals, such as benzene and other aromatic hydrocarbons, has been associated with an increased risk of multiple myeloma.
Understanding these risk factors is crucial for early detection and prevention strategies in multiple myeloma.
What Are the Types of Multiple Myeloma?
- MGUS (Monoclonal Gammopathy of Undetermined Significance): A precancerous condition with abnormal plasma cells producing monoclonal protein, but no symptoms or organ damage.
- Smoldering Myeloma: An intermediate stage with higher levels of monoclonal protein and plasma cells but no active symptoms or tissue damage.
- Active Myeloma: The advanced stage where plasma cells proliferate uncontrollably, leading to bone lesions, kidney dysfunction, anemia, and other complications.
Early detection and monitoring are essential to determine the risk of progression and guide treatment decisions.
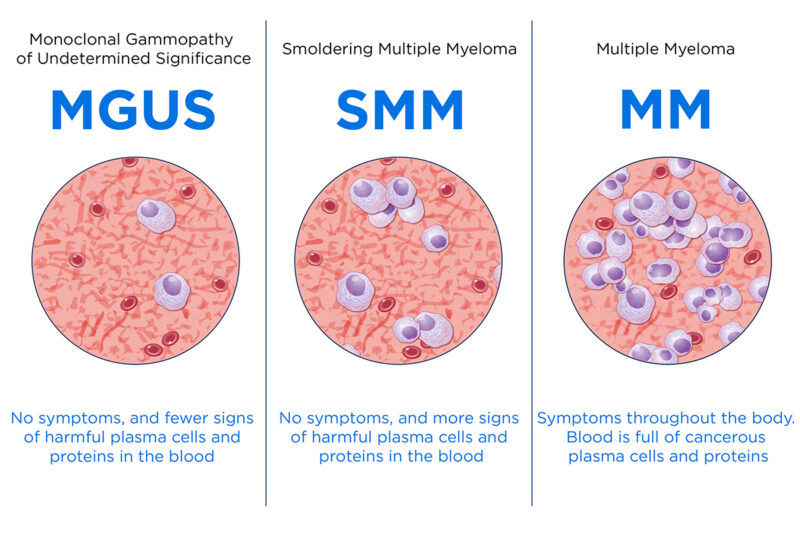
Smoldering Myeloma
Smoldering multiple myeloma (SMM) is an asymptomatic, precancerous condition characterized by elevated levels of monoclonal protein (M protein) and an increased percentage of plasma cells in the bone marrow. Unlike active multiple myeloma, SMM does not present with symptoms or organ damage.
- Detection: SMM is often detected incidentally during routine blood tests that reveal elevated M protein levels. Further diagnostic evaluations, including blood and urine tests, bone marrow biopsies, and imaging studies, are conducted to confirm the diagnosis. According to the American Cancer Society, individuals with SMM exhibit plasma cells in the bone marrow between 10% and 60% and higher than normal levels of M protein in the blood.
- Progression to Active Myeloma: The risk of SMM progressing to active multiple myeloma varies. Generally, the progression rate is approximately 10% per year for the first five years, then decreases to 3% per year for the next five years, and about 1% per year thereafter. Factors influencing progression include the level of M protein, the percentage of plasma cells in the bone marrow, and specific genetic markers. The American Cancer Society notes that people with high-risk SMM may consider treatment with medications, such as lenalidomide, with or without dexamethasone, to lower the risk of progression to active myeloma.
MGUS (Monoclonal Gammopathy of Undetermined Significance)
characterized by the presence of an abnormal monoclonal protein (M protein) produced by plasma cells in the blood. While MGUS itself is asymptomatic and does not cause harm, it is considered a precursor to more serious plasma cell disorders, such as multiple myeloma.
- Benign Nature and Need for Monitoring: Individuals with MGUS do not exhibit symptoms or organ damage. However, due to its potential to progress to malignant conditions, regular monitoring is essential. This typically involves periodic blood tests to measure M protein levels and assess for any signs of disease progression.
- Conversion Rates:The risk of MGUS progressing to multiple myeloma or related disorders is approximately 1% per year(American Cancer Society). This statistic underscores the importance of ongoing surveillance to detect any changes early
How Is Multiple Myeloma Diagnosed?
Diagnosing multiple myeloma requires a combination of laboratory tests, imaging studies, and bone marrow examinations to accurately assess the presence and extent of the disease.Since early symptoms can be vague or mistaken for other conditions, precise diagnostic procedures are crucial for detecting multiple myeloma before significant complications arise.
One of the first steps in diagnosis is blood testing, where physicians look for abnormal monoclonal proteins (M proteins) that signal plasma cell disorders.Serum protein electrophoresis (SPEP) is commonly used to identify and quantify M proteins in the blood, while a serum free light chain assay helps detect abnormal protein fragments not always visible in SPEP results.According to the American Cancer Society, these tests are essential for determining whether a patient has multiple myeloma, smoldering myeloma, or a precursor condition like MGUS. (American Cancer Society, Author: Rebecca L. Siegel)
To further confirm the diagnosis, a bone marrow biopsy is often performed, where a small sample of bone marrow is extracted—typically from the hip bone—and examined under a microscope.The percentage of plasma cells present in the sample is a key indicator, as multiple myeloma is characterized by an overproduction of these cells.Additionally, cytogenetic analysis can reveal chromosomal abnormalities that provide valuable prognostic information, helping physicians determine the likely course of the disease. (American Cancer Society, Author: Kimberly D. Miller)
Imaging tests also play a significant role in diagnosing multiple myeloma, especially in assessing bone damage and tumor spread. X-rays can detect bone lesions, which are common in myeloma patients due to excessive plasma cell activity weakening the skeletal structure. For a more detailed view, magnetic resonance imaging (MRI) and positron emission tomography (PET) scans are used to identify active disease sites in the bone marrow.These advanced imaging techniques have improved early detection and treatment planning by pinpointing areas of concern before severe damage occurs. (American Cancer Society, Author: Carol E. DeSantis)
What Are the Treatment Options for Multiple Myeloma?
Multiple myeloma treatment varies based on disease stage, patient health, and genetic factors. Standard and emerging therapies include:
- Chemotherapy – Uses cytotoxic drugs to target and kill rapidly dividing myeloma cells.
- Stem Cell Transplants – High-dose chemotherapy followed by transplantation of healthy stem cells to restore bone marrow function.
- Immunotherapy – Boosts the immune system to recognize and attack myeloma cells, including monoclonal antibodies and checkpoint inhibitors.
- Targeted Therapy – Focuses on specific molecular pathways in myeloma cells to prevent their growth and survival.
- CAR-T Cell Therapy – A cutting-edge approach where a patient’s T cells are genetically engineered to target myeloma cells.
- Radiation Therapy – Used to shrink tumors and relieve bone pain in localized cases.
Each treatment option plays a role in managing multiple myeloma, and combination approaches are often used for the best outcomes.
Chemotherapy
Chemotherapy remains a fundamental treatment for multiple myeloma, helping to slow disease progression and manage symptoms.It works by targeting rapidly dividing myeloma cells, disrupting their ability to grow and multiply.While newer therapies, such as immunomodulators and proteasome inhibitors, have become more common, chemotherapy is still widely used, particularly in combination regimens and for patients who may not be candidates for more aggressive treatments.
Several chemotherapy drugs have been established in treating multiple myeloma. Melphalan, one of the most commonly used agents, has been a standard treatment for decades, especially in patients undergoing autologous stem cell transplantation.Cyclophosphamide is another alkylating agent that is frequently combined with corticosteroids or newer targeted therapies to enhance effectiveness. Doxorubicin, an anthracycline antibiotic, disrupts DNA synthesis and is often part of combination chemotherapy regimens.Additionally, vincristine has been used in some cases to inhibit cancer cell division. More recent additions, such as bortezomib (a proteasome inhibitor) and lenalidomide (an immunomodulatory drug), have revolutionized multiple myeloma treatment, often used alongside traditional chemotherapy for better outcomes. (American Cancer Society, Author: Rebecca L. Siegel)
However, chemotherapy is not without challenges.Due to its broad effects on rapidly dividing cells, it also impacts healthy cells, leading to side effects. Many patients experience fatigue, nausea, and vomiting as their bodies respond to the treatment. Hair loss is another common effect, along with an increased risk of infections due to lowered white blood cell counts.Peripheral neuropathy, which causes tingling or numbness in the hands and feet, can also develop in some patients, particularly with prolonged use of certain drugs. (American Cancer Society, Author: Carol E. DeSantis)
Despite these side effects, chemotherapy continues to improve survival rates for multiple myeloma patients.According to the American Cancer Society, the five-year relative survival rate for multiple myeloma is approximately 60%, with improvements seen in patients receiving combination therapies.Studies show that the integration of chemotherapy with newer targeted treatments has led to better disease control and prolonged remission periods. (American Cancer Society, Author: Kimberly D. Miller)
Immunotherapy
Immunotherapy has emerged as a transformative approach in the treatment of multiple myeloma, particularly through the use of monoclonal antibodies (mAbs). These laboratory-engineered molecules are designed to specifically target antigens present on myeloma cells, thereby enhancing the body’s immune response against the malignancy.
Monoclonal antibodies function by recognizing and binding to specific proteins on the surface of myeloma cells. This binding can directly inhibit tumor growth or mark the cancer cells for destruction by the immune system. For instance, elotuzumab targets the SLAMF7 protein on myeloma cells, activating natural killer (NK) cells and promoting antibody-dependent cellular cytotoxicity (ADCC). This dual action not only flags the malignant cells for immune attack but also stimulates the immune effector cells to enhance their cytotoxic activity.
Clinical trials have demonstrated the efficacy of monoclonal antibodies in improving patient outcomes. In the ELOQUENT-2 trial, elotuzumab combined with lenalidomide and dexamethasone was evaluated in patients with relapsed or refractory multiple myeloma. The study reported a significant reduction in the risk of disease progression or death by 30% compared to lenalidomide and dexamethasone alone. Specifically, the median progression-free survival (PFS) was 19.4 months in the elotuzumab group versus 14.9 months in the control group. Additionally, the overall response rate (ORR) was higher in the elotuzumab group, indicating a more favorable treatment outcome.
Daratumumab, a monoclonal antibody targeting the CD38 protein on myeloma cells, has demonstrated significant efficacy in combination therapies for relapsed or refractory multiple myeloma. In the phase 3 CASTOR trial, led by Dr. Antonio Palumbo and published in the New England Journal of Medicine, the addition of daratumumab to bortezomib and dexamethasone resulted in a 61% reduction in the risk of disease progression or death compared to bortezomib and dexamethasone alone. Specifically, the median progression-free survival was 16.7 months in the daratumumab group versus 7.1 months in the control group.
Dr. Thierry Facon’s research, presented in the Journal of Clinical Oncology, focused on the IMROZ clinical trial assessing isatuximab in combination with bortezomib, lenalidomide, and dexamethasone (Isa-VRd) for newly diagnosed multiple myeloma patients. The study reported that 63% of patients receiving Isa-VRd remained in remission at four years, compared to 45% with the standard VRd regimen, indicating a substantial improvement in long-term disease control.
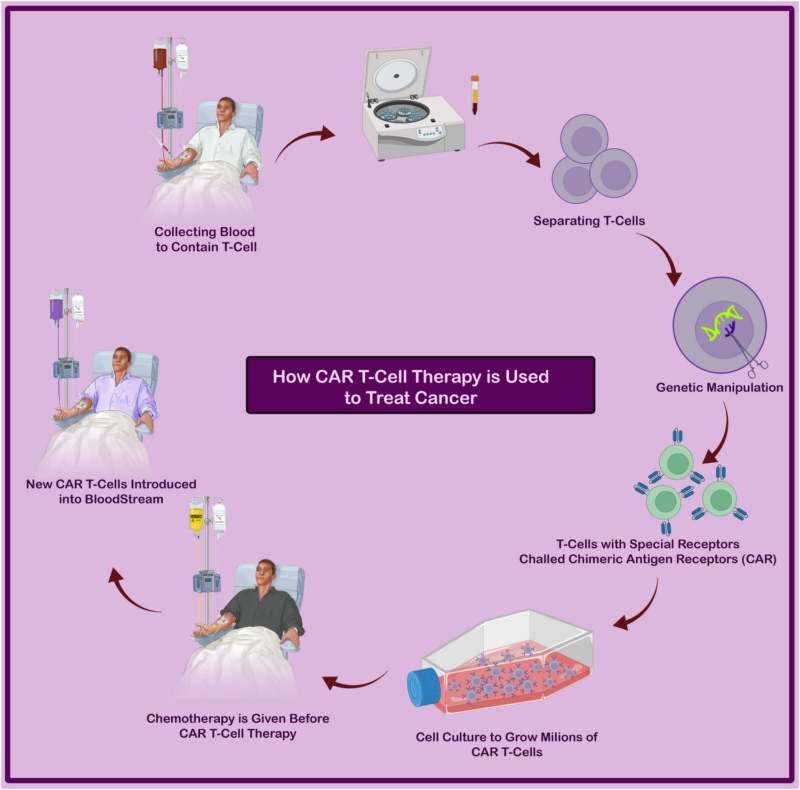
CAR-T Cell Therapy
Chimeric Antigen Receptor (CAR) T-cell therapy represents a groundbreaking advancement in the treatment of multiple myeloma, particularly for patients with relapsed or refractory disease. This innovative approach involves the genetic modification of a patient’s own T cells to express receptors specific to antigens on myeloma cells, thereby enhancing the immune system’s ability to recognize and eradicate these malignant cells.
The process begins with the collection of T cells from the patient, which are then genetically engineered to express chimeric antigen receptors targeting specific proteins on myeloma cells, such as B-cell maturation antigen (BCMA). These modified T cells are expanded in the laboratory and subsequently infused back into the patient. Upon reintroduction, the CAR T cells seek out and bind to BCMA-expressing myeloma cells, initiating a robust immune response that leads to the destruction of these cancerous cells.
Clinical trials have demonstrated the remarkable efficacy of CAR T-cell therapy in treating advanced multiple myeloma. In the pivotal phase 2 KarMMa trial, idecabtagene vicleucel (ide-cel), a BCMA-directed CAR T-cell therapy, was administered to patients with relapsed or refractory multiple myeloma. The study reported an overall response rate (ORR) of 73%, with a median progression-free survival (PFS) of 8.6 months. Notably, 33% of patients achieved a complete response (CR), indicating the absence of detectable disease. These findings underscore the potential of ide-cel to induce significant clinical responses in heavily pretreated patient populations.
Another BCMA-targeted CAR T-cell therapy, ciltacabtagene autoleucel (cilta-cel), has also shown impressive results. In a study involving patients with relapsed or refractory multiple myeloma, cilta-cel achieved an ORR of 98%, with approximately 60% of patients remaining free of disease progression at two years.
What Are the Stages of Multiple Myeloma?
Multiple myeloma is classified into three stages—Stage I, Stage II, and Stage III—based on factors such as blood test results and chromosomal abnormalities. This staging helps determine the disease’s progression, prognosis, and guides treatment strategies.
- Stage I: In this initial stage, the disease progresses slowly and may not present noticeable symptoms. Patients often have lower levels of M protein and fewer myeloma cells in the bone marrow. The prognosis is generally favorable, with treatment approaches focusing on monitoring and, in some cases, initiating therapy to prevent progression. According to Cancer Research UK, almost 80% of people diagnosed at Stage I survive for five years or more.
- Stage II: This intermediate stage is characterized by a higher number of myeloma cells and may present with symptoms such as bone pain. Treatment typically involves a combination of medications, and in some cases, stem cell transplantation to achieve remission. The prognosis varies, with approximately 60% of patients surviving five years or more post-diagnosis.(Cancer Research UK)
- Stage III: The most advanced stage, Stage III, indicates a high number of myeloma cells and significant symptoms, including anemia, kidney dysfunction, and extensive bone damage. Treatment is more aggressive, often combining multiple drug regimens and considering stem cell transplantation. The prognosis is less favorable, with about 40% of patients surviving five years or more.(Cancer Research UK)
After Treatment: What to Expect
The post-treatment phase of multiple myeloma requires ongoing care, as patients often experience lingering side effects and must remain vigilant for recurrence.Fatigue is one of the most common complaints, sometimes persisting for months due to the impact of chemotherapy and other treatments on the body.Many patients find that gentle exercise, proper hydration, and a balanced diet help manage energy levels.
Regular follow-up visits are essential, including blood tests and imaging to detect early signs of relapse.Patients often describe the anxiety of waiting for test results, but experts emphasize that early detection of recurrence allows for better treatment options.According to the American Cancer Society, ongoing monitoring every three to six months is recommended.
Lifestyle adjustments, such as avoiding infections, maintaining bone health, and managing emotional well-being, are crucial for long-term recovery.Support groups and counseling can help patients cope with the psychological impact of living with a chronic condition.Ultimately, the goal is to maintain the best possible quality of life while staying proactive about health.
How Long Does It Take to Notice and Treat Multiple Myeloma?
The journey from initial symptom onset to the diagnosis and commencement of treatment for multiple myeloma varies among patients. Studies indicate that the median time from first symptoms to diagnosis ranges between 4 to 6 months. For instance, a study by Dr. Hartmut Goldschmidt et al. reported a median diagnostic interval of 4 months.
In a study published in Leukemia Research, first author Dr. Jayakrishnan TT and colleagues analyzed data from 38,178 multiple myeloma patients, revealing a median time to systemic therapy initiation of 17 days. Notably, patients who began treatment within 7 days of diagnosis had a median overall survival of 27 months, whereas those who started therapy after 30 days had a median overall survival of 46 months. This suggests that a shorter time to treatment may be associated with more aggressive disease, necessitating prompt intervention. Conversely, a study led by Dr. Hamlet Gasoyan, published in Blood Cancer Journal, examined 720 newly diagnosed multiple myeloma patients and found a median time of 28 days from diagnosis to the initial prescription fill of oral antimyeloma medication. This study highlighted disparities in treatment initiation times, particularly among older patients, Black patients, and those diagnosed during inpatient admissions.
Delays in diagnosis and treatment initiation can lead to increased disease-related complications. Therefore, prompt recognition of symptoms and timely medical intervention are crucial to improving patient outcomes.
How to Live with Multiple Myeloma?
Living with multiple myeloma requires a balanced approach to physical and emotional well-being. Bone health is crucial, so patients should include calcium and vitamin D in their diet and engage in low-impact exercises like walking or yoga to prevent fractures. To reduce infection risk, hand hygiene, vaccinations, and avoiding sick individuals are essential, as myeloma and its treatments weaken the immune system.
Coping strategies include managing fatigue by prioritizing rest and pacing activities. Support groups and counseling can help with emotional stress, and staying connected with family and friends provides crucial encouragement. Expert recommendations also emphasize proper nutrition, staying hydrated, and regular check-ups to monitor disease progression and treatment side effects. A positive mindset, proactive self-care, and strong support networks can improve quality of life while managing multiple myeloma.
Can Multiple Myeloma Be Prevented?
Preventing multiple myeloma involves regular screenings for high-risk individuals, lifestyle modifications, and vigilant monitoring for those diagnosed with monoclonal gammopathy of undetermined significance (MGUS).
- Regular Screenings for High-Risk Individuals: While routine screening for multiple myeloma in the general population isn’t standard practice, individuals with a family history or other risk factors should consult healthcare providers about potential screenings. Early detection can lead to more effective management strategies.
- Lifestyle Changes: Adopting a healthy lifestyle may reduce the risk of progression to multiple myeloma. Maintaining a balanced diet, engaging in regular physical activity, and avoiding exposure to known environmental risk factors are advisable.
- Monitoring for MGUS Patients: MGUS is a condition where an abnormal protein is present in the blood, which can progress to multiple myeloma at an average rate of 1% per year. Regular monitoring is essential to detect any changes early. The International Myeloma Working Group recommends that all patients with MGUS be reassessed six months after diagnosis with tests including complete blood count, serum protein electrophoresis, free light chain assay, calcium, and creatinine to determine clinical stability. If stable, follow-up evaluations can occur annually. This approach helps in early identification of progression to more serious conditions.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is multiple myeloma?
Multiple myeloma is a type of blood cancer that affects plasma cells, which are white blood cells responsible for producing antibodies. It leads to abnormal cell growth in the bone marrow, reducing normal blood cell production.
What are the early symptoms of multiple myeloma?
Early symptoms may include bone pain, fatigue, frequent infections, and high calcium levels in the blood. Some patients may not have noticeable symptoms in the early stages.
What causes multiple myeloma?
The exact cause is unknown, but risk factors include genetic mutations, exposure to radiation or certain chemicals, and a history of monoclonal gammopathy of undetermined significance (MGUS).
How is multiple myeloma diagnosed?
Diagnosis involves blood tests (such as protein electrophoresis), urine tests, bone marrow biopsy, and imaging studies (MRI, CT, or PET scans) to detect abnormal plasma cells and bone damage.
What are the stages of multiple myeloma?
Multiple myeloma is classified into three stages based on the Revised International Staging System (R-ISS), which considers beta-2 microglobulin levels, albumin levels, and genetic abnormalities.
What are the treatment options for multiple myeloma?
Treatment may include chemotherapy, targeted therapy, immunotherapy, stem cell transplantation, and supportive care to manage symptoms like bone pain and kidney dysfunction.
Is multiple myeloma curable?
There is no cure for multiple myeloma, but treatments can help control the disease and prolong survival. Some patients achieve long-term remission with effective therapy.
How does multiple myeloma affect the bones?
Myeloma cells release substances that weaken bones, leading to fractures, pain, and osteoporosis. Bone-strengthening drugs like bisphosphonates can help manage these complications.
Can multiple myeloma be inherited?
Multiple myeloma is not directly inherited, but a family history of the disease may slightly increase the risk. Genetic factors may play a role in susceptibility.
What lifestyle changes can help manage multiple myeloma?
A balanced diet, regular exercise, hydration, and avoiding infections can help improve quality of life. Patients should also follow their doctor’s recommendations and attend regular check-ups.