What is Melanoma ?
Melanoma is a type of skin cancer that originates in the melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color. It is one of the most serious forms of skin cancer because it can spread (metastasize) to other parts of the body and become life-threatening. Understanding the symptoms, causes, diagnosis, treatment, prevention, stages, prognosis, and survival rates of this skin cancer is crucial for patients and their families.
Causes and Risk Factors
The etiology is complex, involving an interplay between genetic predispositions and environmental exposures, particularly to UV radiation. Understanding these risk factors is essential for developing targeted prevention strategies, such as minimizing UV exposure, regular skin examinations, and, for those with a family history, considering genetic counseling and testing.
- Genetic Factors: Approximately 10% of cases are considered hereditary. The most well-known genes associated with an increased risk of melanoma include: CDKN2A, CDK4, TERT, POT1, MC1R, MITF:
- Environmental Factors: The primary environmental risk factor is exposure to ultraviolet (UV) radiation from the sun and artificial sources like tanning beds. UV radiation causes DNA damage in skin cells, which can lead to mutations and the development of melanoma.
Other Risk Factors
Several other factors can influence an individual’s risk of developing melanoma, including:
- Moles: Having a large number of moles (more than 50) or atypical moles (dysplastic nevi) increases melanoma risk.
- Skin Type: Individuals with fair skin, light hair, and eyes, and those who freckle or burn easily are at higher risk.
- Family History: Having a close relative with melanoma increases one’s risk, suggesting a genetic component.
- Age: While melanoma can occur at any age, the risk increases with age. However, it is also one of the most common cancers in young adults.
Signs and Symptoms
The symptoms and signs are primarily observed as changes in the skin, and they can be remembered using the “ABCDE” rule, which helps in identifying characteristics of unusual moles or skin lesions that may indicate melanoma.
ABCDE Rule
- Asymmetry (A): Most benign moles are symmetrical, meaning if you draw a line through the middle, the two halves will match. In contrast, melanomas are often asymmetrical, where one half does not match the other.
- Border (B): The borders of early melanomas are often uneven and may have scalloped or notched edges. Common moles, on the other hand, tend to have smoother, more even borders.
- Color (C): A typical mole is usually a single shade of brown. Melanomas, however, may contain various shades of brown, tan, or black, and as they progress, they can also show colors like red, white, or blue. This variation in color is a significant warning sign.
- Diameter (D): Melanomas are typically larger in diameter than a pencil eraser (about 6mm or 1/4 inch), although they can be smaller when first detected.
- Evolving (E): Any change in size, shape, color, or elevation of a spot on your skin, or any new symptom in it, such as bleeding, itching, or crusting, may be a warning sign. A mole or skin lesion that looks different from the rest or changes in any way should be evaluated.
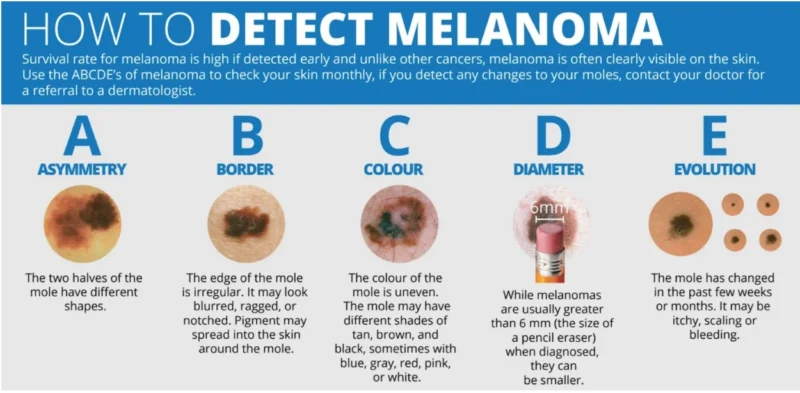
The image is taken from the www.melanomanetwork.ca
Diagnosis
The diagnosis involves a multi-step process that typically begins with a visual examination of the skin lesion, followed by a biopsy and further testing if necessary.
- Visual Examination – The first step in diagnosing is a thorough visual examination and using the ABCDE criteria of the skin lesion. The healthcare provider may also use a dermatoscope, a handheld device that provides a magnified and illuminated view of the skin lesion, allowing for a more detailed examination of its structure and patterns.
- Biopsy – If the visual examination raises suspicion of melanoma, the next step is to perform a biopsy. A biopsy involves removing a sample of the skin lesion or the entire lesion for microscopic examination by a pathologist.
Staging
If melanoma is confirmed, the next step is to determine the stage of the disease, which is crucial for guiding treatment decisions and predicting prognosis. The stages range from 0 to IV, with each stage reflecting the severity and spread of the cancer.
- Stage 0 (Melanoma in Situ) – The cancer is confined to the top, outer layer of the skin (epidermis) and has not invaded deeper layers or spread to other parts of the body.
- Stage I – The cancer has invaded the next layer of skin (dermis) but is still relatively thin and has not spread to lymph nodes or distant sites. It is divided into IA and IB based on thickness and ulceration.
- Stage II – The cancer is thicker than in Stage I, may or may not be ulcerated, but has not spread to lymph nodes or distant sites. It is divided into IIA, IIB, and IIC, based on thickness and ulceration.
- Stage III – The cancer has spread to nearby lymph nodes, nearby skin, or tissues under the skin (subcutaneous). It may involve satellite tumors or in-transit metastases. It is divided into IIIA, IIIB, IIIC, and IIID, based on factors like the number of lymph nodes involved and ulceration.
- Stage IV – The cancer has spread to distant lymph nodes, organs, or tissues, such as the lungs, liver, brain, bone, or gastrointestinal tract. It is further categorized based on the location of distant metastases (M1a, M1b, M1c, M1d).
Watch this video about “The 4 stages of Melanoma” from MayoClinic
Types
There are several distinct types of melanoma, each with its own characteristics and clinical presentation. Here are the main types:
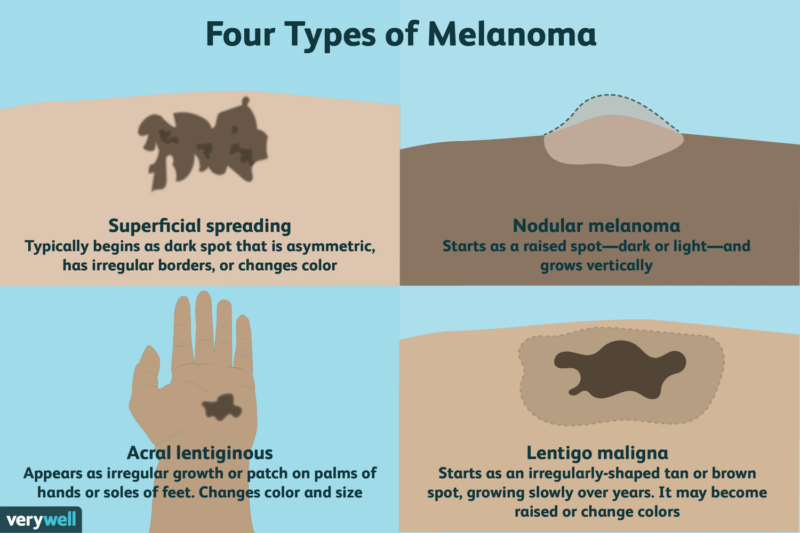
1. Superficial Spreading Melanoma
Superficial spreading melanoma (SSM) is the most common type, accounting for approximately 70% of all cases. It typically appears as an irregular, asymmetric flat lesion with uneven borders and variable colors, including shades of brown, black, red, blue, and white. SSM initially grows horizontally (radial growth phase) before invading deeper into the skin (vertical growth phase). It can occur on any part of the body but is most common on the trunk in men and the legs in women.
2. Nodular Melanoma
Nodular melanoma (NM) accounts for approximately 15-20% of all cases. It is characterized by a raised, firm, and often ulcerated nodular lesion that grows rapidly in a vertical pattern, invading deeper layers of the skin from the outset. NM is typically dark in color, ranging from blue-black to red or skin-colored (amelanotic). It can occur on any part of the body but is most common on the trunk, head, and neck.
3. Lentigo Maligna Melanoma
Lentigo maligna melanoma (LMM) represents approximately 4-15% of the cases. It typically develops in older individuals (median age of 65-70 years) and is associated with chronic sun exposure. LMM often begins as a flat, irregular, and slow-growing lesion called lentigo maligna, which can remain in this radial growth phase for years before becoming invasive. LMM is most commonly found on sun-exposed areas, such as the face, neck, and arms.
4. Acral Lentiginous Melanoma
Acral lentiginous melanoma (ALM) is a rare subtype, accounting for 2-3% of all cases in Caucasians but up to 60% in people of color. It typically appears as a flat or slightly raised, irregularly pigmented lesion on the palms, soles, or beneath the nails (subungual melanoma). ALM is not associated with sun exposure and is more common in older individuals.
Patterns of Metastasis
The metastases occur when cancer cells spread from the primary tumor site to other parts of the body.
- Regional Lymph Nodes: It commonly metastasizes to the regional lymph nodes. This is often the first site of spread, especially those located close to large collections of lymph nodes.
- Satellite and In-Transit Metastases: These occur when cancer cells spread to areas of the skin or subcutaneous tissue between the primary tumor and the regional lymph nodes. They are more common to be located on the extremities and trunk.
- Distant Metastases: It can also spread to distant organs, including the brain, liver, lungs, and bones. This type of spread is more common in later stages of the disease and is associated with a poorer prognosis.
Treatment
Treatment involves a multifaceted approach that can include surgery, radiation therapy, targeted therapy, immunotherapy, and in some cases, chemotherapy. The choice of treatment depends on various factors, including the stage, its location, whether it has spread, and the patient’s overall health.
1. Surgery
Surgery is the cornerstone of the treatment, especially in its early stages or when the melanoma is localized. The primary goal is to completely remove the cancer along with a margin of healthy tissue to ensure no cancer cells remain. The extent of surgery depends on the melanoma’s thickness and location.
- Wide Local Excision (WLE) – This procedure involves removing the cancer along with a margin of normal skin around it. The size of the margin depends on the thickness of the cancer. WLE is typically performed under local anesthesia, but general anesthesia may be used for larger excision.
- Lymph Node Removal – If it has spread to the lymph nodes, these may be surgically removed in a procedure known as a lymphadenectomy. This can be done at the same time as a wide excision to avoid multiple surgeries.
- Reconstructive Surgery – For larger cancers or those in visible areas such as the face, reconstructive surgery may be performed to restore appearance and function. This may involve skin grafts or flaps from other parts of the body.
2. Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It’s not commonly used to treat primary cancer but may be employed in certain situations, such as to treat melanomas that have spread to the brain, bones, or other distant sites, or to alleviate symptoms caused by tumors. It can also be used after surgery in cases where there’s a high risk of recurrence.
3. Targeted Therapy
Targeted therapy drugs focus on specific genetic mutations within cancer cells that help them grow. About half of all melanomas have mutations in the BRAF gene. Drugs targeting the BRAF protein or related MEK proteins can be effective in treating advanced melanomas with these mutations. Common targeted therapy drugs include vemurafenib (Zelboraf), dabrafenib (Tafinlar), and encorafenib (Braftovi) for BRAF mutations, and trametinib (Mekinist) and cobimetinib (Cotellic) for MEK mutations.
4. Immunotherapy
Immunotherapy boosts the body’s immune system to fight cancer. It’s particularly useful for treating advanced melanoma. Common immunotherapy drugs include checkpoint inhibitors like ipilimumab (Yervoy), pembrolizumab (Keytruda), and nivolumab (Opdivo), which help the immune system recognize and attack cancer cells. T-VEC (Imlygic) is an oncolytic virus therapy that directly kills cancer cells and stimulates an immune response.
5. Chemotherapy
Chemotherapy uses drugs to kill cancer cells and is sometimes used to treat advanced melanoma. However, it’s not as effective in this type of cancer as other treatments like targeted therapy and immunotherapy. Chemotherapy might be considered if other treatments are not suitable.
6. Treatment for Advanced Melanoma
For advanced melanoma that cannot be cured, the focus shifts to palliative care, aiming to relieve symptoms and improve quality of life. This may involve a combination of the treatments mentioned above, tailored to manage symptoms and control the cancer’s spread as much as possible.
“Melanoma Patient Voices: Christine’s Story” from Novartis
The prognosis and survival rate
- Stage 0 (Melanoma in situ): 5-year survival rate is 99.9%
- Stage I (Early-stage invasive): 5-year survival rate is 89-95%
- Stage II (Invasive): 5-year survival rate is 53-92%
- Stage III (spread to lymph nodes): 5-year survival rate is 40-78%
- Stage IV (Metastatic): – 5-year survival rate is 15-25%
A few key points about melanoma prognosis:
- Early detection is crucial, as thinner melanomas have much higher cure rates compared to thicker, more invasive ones.
- Presence of ulceration and spread to lymph nodes or distant organs significantly worsens the prognosis.
- New targeted therapies and immunotherapies have improved survival rates for advanced stage III and IV melanoma in recent years compared to older data.
- Other factors like age, gender, location of the primary tumor etc. also play a role in determining an individual’s prognosis.
So in summary, the stage at diagnosis is the most important factor determining the melanoma prognosis and survival outlook. Early detection when the tumor is thin provides the best chance for cure.
“Melanoma Patient Voices: Jackie’s Story” from Novartis
Resources
- Compass Oncology – compassoncology.com
- Early diagnosis of cutaneous melanoma: revisiting the ABCD criteria, Clinical ABCDE rule for early melanoma detection – PubMed
- American Cancer Society – cancer.org
- Cancer Research UK – cancerresearchuk.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- National Cancer Institute – cancer.gov
- Johns Hopkins Medicine – hopkinsmedicine.org
- Canadian Cancer Society – cancer.ca
- Oncodaily.com – Online platform where you can find anything related to cancer such as everyday news, blogs, videos, podcasts, etc.
- Evolving concepts in melanoma classification and their relevance to multidisciplinary melanoma patient care – PubMed
- Stanford Medicine – med.stanford.edu
- Targeted therapy and immunotherapy in advanced melanoma: an evolving paradigm, Immunotherapy in Melanoma: Recent Advances and Future Directions – PubMed