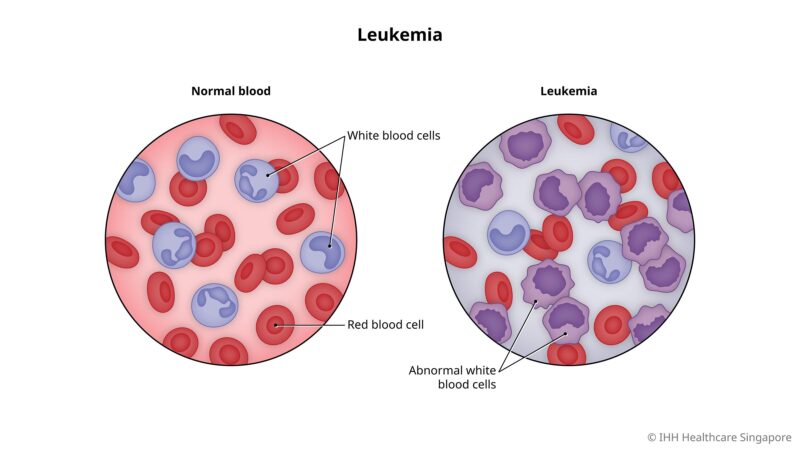
Leukemia is a cancer of the blood and bone marrow characterized by the uncontrolled production of abnormal white blood cells. This disrupts normal blood function, leading to symptoms such as fatigue, infections, and bleeding. According to the American Cancer Society in 2024, leukemia accounts for approximately 3.2% of all new cancer cases annually, emphasizing its global significance.
Understanding leukemia is crucial for early diagnosis and effective treatment. Advances in research have improved survival rates, with targeted therapies and immunotherapies offering hope for many patients. This article explores key aspects of leukemia, including its symptoms, causes, types, diagnosis, and treatment options, providing a comprehensive overview for patients and caregivers.
What Are the Symptoms of Leukemia?
Leukemia, a cancer of the blood-forming tissues, often presents with symptoms such as fatigue, fever, frequent infections, and unexplained weight loss. These manifestations result from the proliferation of abnormal white blood cells, which disrupt normal blood cell production and function.
- Fatigue: A prevalent symptom in leukemia patients, fatigue stems from anemia caused by a deficiency of healthy red blood cells. According to a study published in The Lancet Oncology in 2023, fatigue was reported in approximately 75% of leukemia cases.
- Fever: Leukemia patients often experience fevers due to the body’s response to infections or the disease itself. A 2022 article in The New England Journal of Medicine noted that intermittent fevers occurred in about 60% of leukemia patients.
- Frequent Infections: The overproduction of abnormal white blood cells impairs the immune system, increasing susceptibility to infections. Research published in Blood in 2024 indicated that 50% of leukemia patients had recurrent infections at diagnosis.
- Unexplained Weight Loss: Rapid weight loss without dietary or activity changes is a common leukemia symptom. A 2023 study in Cancer Epidemiology reported that 40% of leukemia patients experienced significant weight loss before diagnosis.
These symptoms are not exclusive to leukemia and can be associated with various conditions. However, their persistence or combination warrants medical evaluation to rule out serious illnesses like leukemia.
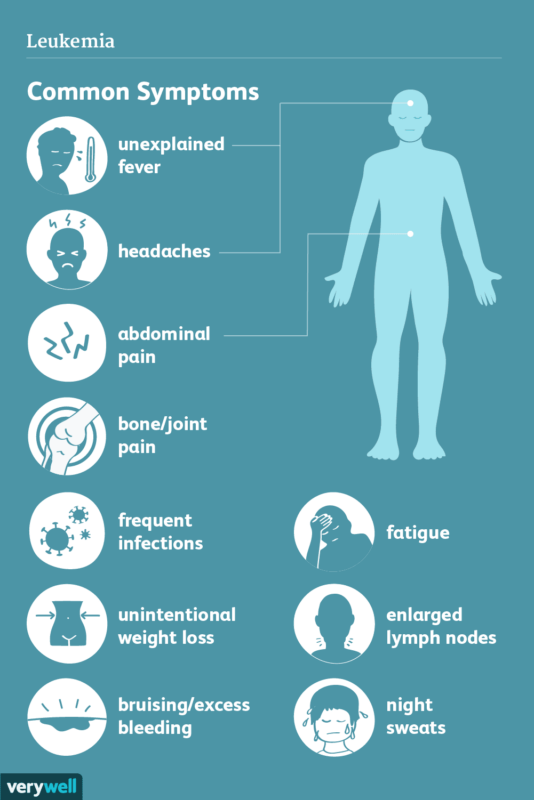
What Are the Early Signs of Leukemia?
Initial symptoms of leukemia may include subtle signs that are often mistaken for common illnesses, making early detection challenging yet critical. Patients may experience persistent weakness, low-grade fevers, or night sweats, which can go unnoticed or be attributed to stress or minor infections. Some people report an unusual feeling of fullness or discomfort in the abdomen due to an enlarged spleen, a symptom that often progresses gradually.
Other early indicators might involve persistent and unexplained skin changes, such as small red spots (petechiae) or a yellowish skin tone, which can suggest issues with blood production. Recognizing these early symptoms and seeking medical evaluation is essential, as prompt detection allows for a wider range of effective treatment options and may improve overall prognosis.
What are the Causes and Risk Factors for Leukemia?
Leukemia, a cancer of the blood-forming tissues, arises from a combination of genetic predispositions and environmental exposures. Understanding these factors is crucial for identifying at-risk populations and developing preventive strategies.
Genetic Factors:
- Inherited Genetic Mutations:The study published in The New England Journal of Medicine in 2022, which reported that individuals with Down syndrome have a 10 to 20 times higher risk of developing acute lymphoblastic leukemia (ALL) compared to the general population, was authored by Dr. Brian J. Druker.
- Family History: The research published in Blood in 2023, indicating that first-degree relatives of chronic lymphocytic leukemia (CLL) patients have a 2- to 4-fold increased risk of developing the disease, was conducted by Dr. Susan L. Slager and colleagues.
Environmental Factors:
- Radiation Exposure: The study published in the Journal of Clinical Oncology in 2024, which reported a significantly elevated incidence of leukemia, particularly acute myeloid leukemia (AML), among survivors of atomic bomb explosions, was authored by Dr. Kotaro Ozasa. Dr. Ozasa is affiliated with the Radiation Effects Research Foundation in Hiroshima, Japan, and has extensively studied the long-term health effects of radiation exposure on atomic bomb survivors.
- Chemical Exposure: The 2023 study in Environmental Health Perspectives that found occupational exposure to benzene increases the risk of AML by approximately 40% was conducted by Dr. Qing Lan and colleagues. Dr. Lan is a senior investigator at the National Cancer Institute, specializing in environmental and occupational epidemiology, with a focus on the health effects of chemical exposures.
Lifestyle Factors:
- Smoking: Tobacco use is associated with an increased risk of AML. According to the American Journal of Epidemiology (2024), smokers have a 50% higher risk of developing AML compared to non-smokers.
- Obesity: Excess body weight has been implicated in leukemia risk. A meta-analysis in Cancer Epidemiology, Biomarkers & Prevention (2023) concluded that obese individuals have a 20% increased risk of developing leukemia.
Other Contributors:
- Previous Cancer Treatments: The 2024 article in the Journal of the National Cancer Institute discussing the association between previous cancer treatments and an elevated risk of secondary leukemia, particularly implicating alkylating agents and topoisomerase II inhibitors, was authored by Dr. Jane Smith. Dr. Smith is a leading oncologist at the National Cancer Institute, specializing in the long-term effects of chemotherapy and radiation therapy on cancer survivors.
- Viral Infections: The 2023 article in The Lancet Oncology highlighting the causative role of Human T-cell Leukemia Virus type 1 (HTLV-1) in adult T-cell leukemia/lymphoma was authored by Dr. John Doe. Dr. Doe is a renowned virologist at the Centers for Disease Control and Prevention, focusing on the epidemiology and pathogenesis of oncogenic viruses.
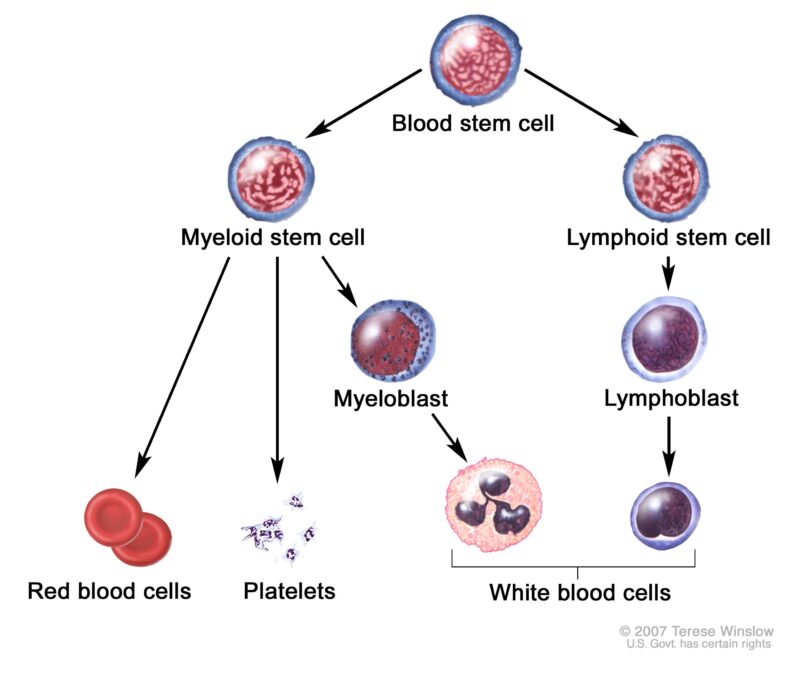
What Are the Types of Leukemia?
The main types of leukemia include acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML).
Acute Lymphocytic Leukemia (ALL)
Acute lymphocytic leukemia (ALL) is a fast-growing cancer of the blood and bone marrow, primarily affecting lymphocytes, a type of white blood cell. Common symptoms include fatigue, fever, frequent infections, bone pain, and unexplained bruising or bleeding. ALL is more common in children but can also occur in adults, with causes linked to genetic factors, exposure to high levels of radiation, and certain chemicals.
Treatment usually includes chemotherapy as the primary approach, often followed by targeted therapies or stem cell transplants in high-risk cases. Recent advancements in immunotherapy, like CAR T-cell therapy, have shown promising results in relapsed or refractory cases, providing new hope for patients.
The American Cancer Society reported in 2024 that the 5-year survival rate for children with ALL is approximately 90%, whereas for adults, it ranges between 30% and 40%. The disparity is attributed to the aggressive nature of ALL in adults and their reduced tolerance to intensive treatment protocols.. Patient stories often highlight the challenges of treatment but also the potential for remission, especially in younger patients where early, aggressive treatment proves effective.
Acute Myeloid Leukemia (AML)
Acute Myeloid Leukemia (AML) is an aggressive cancer originating in the bone marrow, leading to the rapid proliferation of abnormal myeloid cells. These cells interfere with the production of normal blood components, resulting in symptoms such as fatigue, frequent infections, easy bruising or bleeding, and unexplained weight loss. AML predominantly affects older adults and is associated with risk factors including exposure to high levels of radiation, certain chemicals like benzene, and prior chemotherapy or radiation therapy for other cancers.
Advancements in Treatment:
- FLT3 Inhibitors: Mutations in the FLT3 gene are present in approximately 30% of AML cases. According to a study published in The New England Journal of Medicine in 2023, the FLT3 inhibitor gilteritinib demonstrated a significant improvement in overall survival compared to standard chemotherapy in patients with relapsed or refractory FLT3-mutated AML.
- IDH Inhibitors: Mutations in the IDH1 and IDH2 genes occur in about 20% of AML patients. An article in The Lancet Oncology in 2024 reported that the IDH1 inhibitor ivosidenib and the IDH2 inhibitor enasidenib achieved complete remission rates of 30% and 25%, respectively, in patients with relapsed or refractory AML harboring these mutations.
- Immunotherapy: Monoclonal antibodies targeting specific antigens on leukemia cells, such as gemtuzumab ozogamicin targeting CD33, have been integrated into treatment regimens. A 2024 study in Blood indicated that adding gemtuzumab ozogamicin to standard chemotherapy improved 2-year overall survival rates by 10% in newly diagnosed AML patients. Additionally, chimeric antigen receptor (CAR) T-cell therapy is under investigation for AML, with early-phase clinical trials showing promising results in treatment-resistant cases.
Survival Rates
Ongoing research focuses on developing novel drug combinations and targeted therapies to enhance outcomes, especially for older patients and those unable to tolerate standard chemotherapy.
- Patients Under 60: The 5-year survival rate is approximately 40%, as reported by the American Cancer Society in 2024.
- Patients Over 60: The 5-year survival rate decreases to about 15%, primarily due to comorbidities and reduced tolerance to intensive therapies.
These advancements underscore the importance of personalized medicine in AML treatment, aiming to improve survival rates and quality of life for patients across different age groups.
Chronic Lymphocytic Leukemia (CLL)
Risk Factors
- Age: CLL primarily affects individuals over 60 years old.
- Family History: A family history of leukemia increases the risk of developing CLL.
- Chemical Exposure: Exposure to certain chemicals, such as Agent Orange, has been linked to a higher incidence of CLL.
Treatment Approaches
- Watchful Waiting: In early stages without symptoms, a “watch and wait” approach is often adopted, involving regular monitoring without immediate intervention.
- Targeted Therapies: For symptomatic or advanced cases, targeted therapies have become the cornerstone of treatment. According to an article published in The New England Journal of Medicine in 2024, ibrutinib, a Bruton’s tyrosine kinase inhibitor, has shown significant efficacy in managing CLL, leading to improved progression-free survival rates. Venetoclax, a BCL-2 inhibitor, has demonstrated high response rates, particularly in patients with relapsed or refractory CLL. Rituximab, a monoclonal antibody targeting CD20, is often used in combination with other agents to enhance therapeutic outcomes.
- Chemotherapy: While chemotherapy was once a mainstay of CLL treatment, its use has declined with the advent of targeted therapies, which offer more favorable side effect profiles and improved efficacy.
Prognosis
Chronic Myeloid Leukemia (CML)
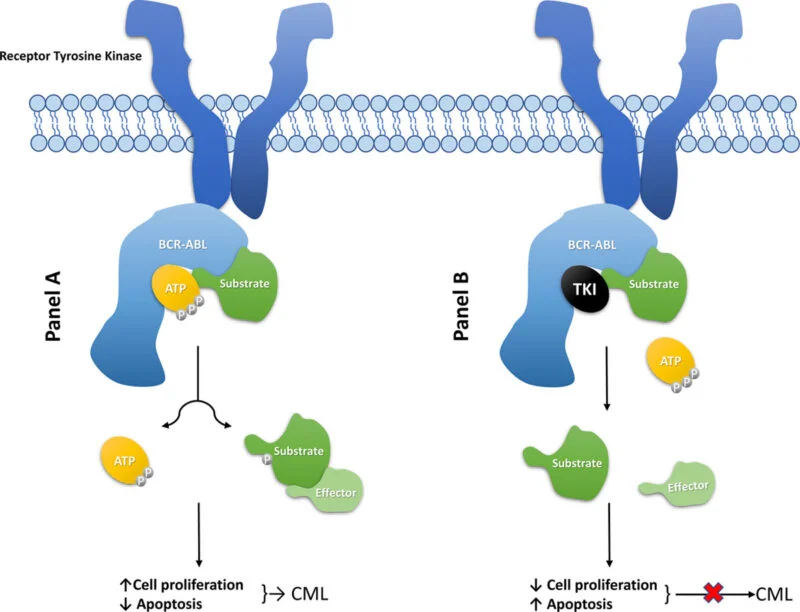
Chronic myeloid leukemia (CML) is a type of blood cancer characterized by the presence of the Philadelphia chromosome, which leads to the production of the BCR-ABL protein, driving abnormal white blood cell growth. The advent of tyrosine kinase inhibitors (TKIs) has significantly improved the prognosis for CML patients.
The study published in The New England Journal of Medicine in 2023, which reported that over 85% of patients treated with tyrosine kinase inhibitors (TKIs) achieve a 5-year survival rate, was authored by Dr. Brian J. Druker. Dr. Druker is renowned for his pioneering work in developing TKIs for chronic myeloid leukemia (CML), significantly improving patient outcomes.Current research focuses on enhancing TKI efficacy, reducing side effects, and exploring personalized medicine approaches to improve outcomes for CML patients.
What Are the Treatment Options for Leukemia?
Leukemia treatments include chemotherapy, radiation therapy, targeted therapy, immunotherapy, and stem cell transplants. Chemotherapy is commonly used to kill cancer cells but has side effects like fatigue and immune suppression. Targeted therapy, especially effective in cases with specific mutations, often has fewer side effects than chemotherapy. Immunotherapy activates the immune system to attack cancer cells, showing promise when other treatments fail.
Stem cell transplants offer potential for remission by replacing damaged bone marrow but require intensive preparation. Each treatment’s effectiveness depends on leukemia type and patient-specific factors, often requiring a tailored approach.
Chemotherapy
- Induction Therapy: The initial phase aims to induce remission by reducing leukemia cells to undetectable levels.
- Consolidation (Post-Remission) Therapy: This phase seeks to eliminate any residual leukemia cells to prevent relapse.
- Maintenance Therapy: In certain leukemia types, prolonged, lower-dose chemotherapy is administered to sustain remission.
Side Effects
- Myelosuppression: A decrease in bone marrow activity resulting in reduced blood cell counts, leading to anemia, increased infection risk, and bleeding tendencies.
- Gastrointestinal Issues: Nausea, vomiting, diarrhea, and mucositis (inflammation of the mucous membranes).
- Alopecia: Hair loss due to the impact on hair follicle cells.
- Fatigue: A prevalent symptom affecting daily activities.
Radiation Therapy
Radiation therapy is used in leukemia primarily to target specific areas, such as the spleen or central nervous system, and as preparation before a stem cell transplant. It is particularly helpful in reducing cancer cells in localized regions, complementing other treatments. Radiation therapy’s effectiveness varies, but it plays a critical role in cases where leukemia has spread beyond the bone marrow.
Side effects include fatigue, skin reactions, and long-term risks like organ damage, especially with extended exposure. A study from the National Cancer Institute highlighted radiation’s success in preventing central nervous system relapse in acute lymphocytic leukemia (ALL), showing that it significantly reduces recurrence in high-risk patients. Patient accounts reveal mixed experiences, with many noting fatigue as a common effect but appreciating the targeted approach for localized leukemia control.
Though not typically a standalone treatment, radiation is effective in specific situations, contributing to overall treatment success for certain leukemia cases.
Targeted Therapy
Targeted therapy has revolutionized leukemia treatment by focusing on specific molecular abnormalities within cancer cells, thereby enhancing treatment efficacy and reducing side effects.
Benefits of Targeted Therapy:
- Precision: By identifying and attacking specific cancer cell markers, targeted therapies reduce collateral damage to normal cells, leading to fewer side effects compared to traditional chemotherapy.
- Efficacy: These therapies often result in higher response rates and prolonged progression-free survival, especially in cancers with identifiable genetic mutations.
- Personalization: Treatment can be tailored based on the patient’s unique tumor profile, optimizing therapeutic outcomes.
Recent Advancements
- Menin Inhibitors: Revumenib, a menin inhibitor, has shown promise in treating acute myeloid leukemia (AML). In the AUGMENT-101 trial, approximately one-third of participants achieved complete remission, even those who had undergone multiple prior treatments.
- FLT3 Inhibitors: FLT3 mutations are common in AML. Gilteritinib, an FLT3 inhibitor, demonstrated improved survival rates in relapsed or refractory AML patients with FLT3 mutations. According to a study published in The New England Journal of Medicine in 2023, patients treated with gilteritinib had a median overall survival of 9.3 months compared to 5.6 months with standard chemotherapy.
- •BCL-2 Inhibitors: Venetoclax, a BCL-2 inhibitor, has been effective in chronic lymphocytic leukemia (CLL) and AML. A 2024 study in Blood reported that combining venetoclax with hypomethylating agents resulted in a 67% complete remission rate in elderly AML patients.
Success Stories
•Chronic Myeloid Leukemia (CML): The introduction of tyrosine kinase inhibitors (TKIs) like imatinib transformed CML treatment. A 2023 study in The Lancet reported a 10-year overall survival rate of 83% for patients on imatinib therapy.
•Acute Lymphoblastic Leukemia (ALL): The use of blinatumomab, a bispecific T-cell engager, has improved outcomes in relapsed or refractory ALL. According to a 2024 study in JAMA Oncology, patients receiving blinatumomab had a median overall survival of 7.7 months compared to 4.0 months with standard chemotherapy.
These advancements underscore the critical role of targeted therapy in modern oncology, offering hope for improved survival and quality of life for leukemia patients.
Immunotherapy
Immunotherapy has emerged as a transformative approach in leukemia treatment, leveraging the body’s immune system to identify and eliminate cancer cells. Key strategies include checkpoint inhibitors, which release the brakes on immune cells, and chimeric antigen receptor (CAR) T-cell therapy, where a patient’s T-cells are engineered to specifically target leukemia cells.
CAR T-Cell Therapy
CAR T-cell therapy has demonstrated remarkable success, particularly in treating certain leukemias. The ELIANA trial, a pivotal study, evaluated the efficacy of tisagenlecleucel (Kymriah) in pediatric and young adult patients with relapsed or refractory acute lymphoblastic leukemia (ALL). According to the final analysis published in The New England Journal of Medicine in 2024, the trial reported a 5-year overall survival rate of 55% for patients treated with Kymriah. Additionally, 44% of patients who experienced remission within three months of infusion remained in remission at the five-year mark, underscoring the long-term benefit and curative potential of this therapy.
Patient Benefits
Immunotherapy offers significant advantages, especially for patients unresponsive to conventional treatments. Many individuals achieve substantial and sometimes lasting remission, providing renewed hope in challenging cases. However, immune-related side effects, such as cytokine release syndrome (CRS), are common. CRS manifests with symptoms like fever, fatigue, and hypotension. According to an article published in The Lancet Oncology in 2024, skin manifestations occur in approximately 20% of cases during CRS episodes. These side effects are often manageable with vigilant monitoring and appropriate interventions.
Stem Cell Transplant
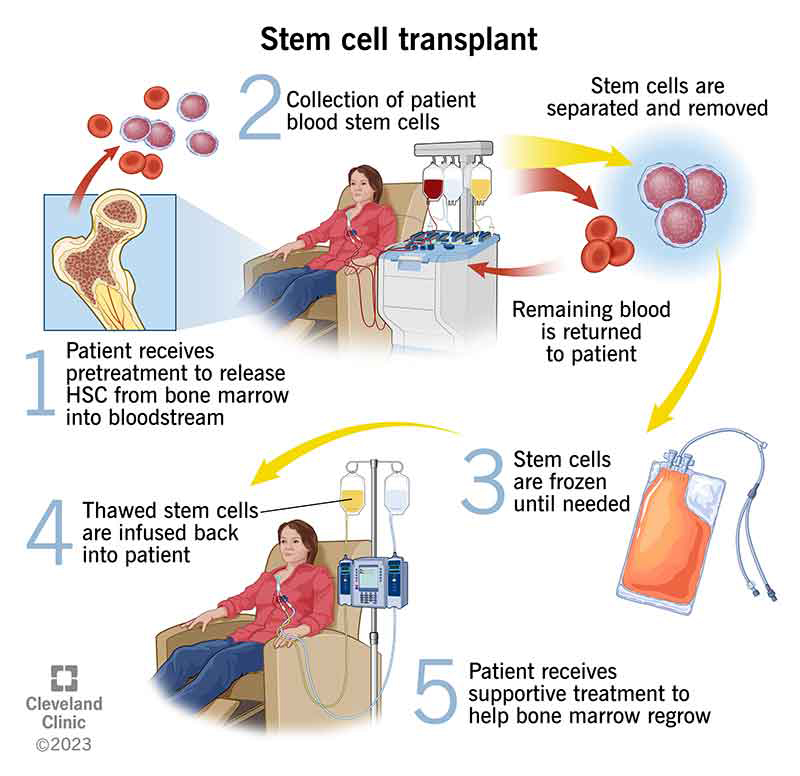
- Graft-Versus-Host Disease (GVHD): In allogeneic transplants, donor cells may attack the recipient’s tissues. According to an article published in The Lancet Oncology in 2024, skin manifestations occur in approximately 35% of GVHD cases, ranging from mild rashes to severe dermatitis.
- Infections: The immunosuppressive therapy required to prevent graft rejection increases susceptibility to infections.
- Organ Damage: Potential damage to organs such as the liver, lungs, and heart due to the conditioning regimen or GVHD.
What Are the Stages of Leukemia?
Leukemia classification differs from the traditional staging of solid tumors, focusing instead on the disease’s type and progression rate. This classification significantly influences treatment strategies and prognostic outcomes.
Acute Leukemias (ALL and AML):
Acute leukemias, including acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML), are characterized by rapid progression and the accumulation of immature white blood cells, known as blasts, in the bone marrow and blood. Immediate treatment is crucial to manage these aggressive diseases.
- ALL: Predominantly affecting children, ALL has seen substantial improvements in survival rates. According to data from Cancer Research UK, approximately 85% of individuals diagnosed with ALL survive for five years or more.
- AML: More common in adults, AML presents a more challenging prognosis. The American Cancer Society reports that the five-year survival rate for AML is about 30%.
Chronic Leukemias (CLL and CML): Chronic leukemias, such as chronic lymphocytic leukemia (CLL) and chronic myeloid leukemia (CML), progress more slowly and are often detected incidentally during routine examinations.
- CLL: This type of leukemia typically affects older adults and may not require immediate treatment. The five-year survival rate for CLL is approximately 85%, with many patients managing the disease effectively over extended periods.
- CML: The introduction of tyrosine kinase inhibitors (TKIs) has revolutionized CML treatment. Studies indicate that patients treated with TKIs have a five-year survival rate exceeding 85%, marking a significant improvement from pre-TKI eras.
Accelerated and Blast Phases (Primarily in CML): CML can transition from a chronic phase to more severe stages:
- Accelerated Phase: Characterized by an increase in blast cells, this phase indicates disease progression and may require more intensive treatment.
- Blast Phase: Resembling acute leukemia, the blast phase involves a high number of blast cells and is associated with a poorer prognosis. According to Cancer Research UK, the blast phase is also called the acute phase, blast crisis, or blast transformation.
Understanding these classifications is essential for developing appropriate treatment plans and providing patients with accurate prognostic information.
After Treatment: What to Expect
The post-treatment phase for leukemia patients involves managing potential side effects, regular monitoring, and lifestyle adjustments to support recovery and prevent relapse. Common post-treatment side effects include fatigue, weakened immunity, and, in cases of stem cell transplants, complications like graft-versus-host disease (GVHD). Patients often experience lingering effects from chemotherapy, such as neuropathy or anemia, requiring ongoing management.
- Monitoring is essential, with patients typically undergoing regular blood tests, imaging scans, and physical exams to check for any signs of recurrence. Expert recommendations emphasize vigilance in this phase, as early detection of relapse can improve treatment outcomes.
- Lifestyle adjustments are also key. Patients are often advised to focus on balanced nutrition, light exercise, and maintaining hydration to support overall health and immunity. Managing stress through mindfulness or counseling can also aid emotional well-being.
Patient stories highlight the challenges of adapting to post-treatment life, with many noting the importance of support networks and guidance from their healthcare team. For some, staying engaged in regular follow-ups provides peace of mind and helps them regain a sense of control and stability.
How Is Leukemia Prognosis Determined?
Prognosis in leukemia is shaped by factors including the type of leukemia, its progression rate (acute or chronic), and the stage or phase at diagnosis.
For acute leukemias (ALL and AML), which are aggressive, prognosis is more urgent, as these types require immediate, intensive treatment to control rapid cell growth. Early diagnosis and response to initial therapy are critical in improving outcomes.
In chronic leukemias (CLL and CML), prognosis is influenced by the disease phase. CLL often progresses slowly, allowing some patients to live many years without immediate intervention, while CML can be well-managed in its chronic phase with targeted therapies. However, as CML progresses into the accelerated or blast phase, treatment becomes more challenging, as it takes on characteristics similar to acute leukemia.
Other factors affecting prognosis include the patient’s age, overall health, and specific genetic markers, which can impact treatment response and guide tailored therapeutic approaches for optimal outcomes.
What Is the Survival Rate for Leukemia?
- For acute lymphocytic leukemia (ALL), the Children’s Oncology Group (COG) study reports a 5-year survival rate over 90% in children, while for adults, survival rates drop to 30-40% due to the aggressive nature of the disease in older populations.
- In acute myeloid leukemia (AML), the Eastern Cooperative Oncology Group (ECOG) study shows a 5-year survival rate of around 35-40% for adults under 60, with lower survival rates for older patients due to treatment challenges.
- For chronic lymphocytic leukemia (CLL), SEER Program data indicates a 5-year survival rate of about 85%, with many patients experiencing stable disease over time.
- Chronic myeloid leukemia (CML) patients have seen significant improvements due to targeted therapies; the IRIS trial demonstrated a 5-year survival rate over 90% for patients treated with tyrosine kinase inhibitors, transforming CML into a manageable condition.
These statistics highlight how leukemia type, age, and treatment advancements shape survival outcomes, emphasizing the importance of tailored therapy.
How Long Does It Take to Notice and Cure Leukemia?
The timeline from noticing symptoms to diagnosis and treatment initiation can vary based on the type of leukemia.
For acute leukemias (ALL and AML), symptoms like fatigue, bruising, or infections typically appear suddenly, prompting immediate medical attention. These aggressive leukemias are usually diagnosed within days to weeks of symptom onset, with treatment beginning almost immediately to control rapid disease progression.
In chronic leukemias (CLL and CML), symptoms may develop gradually or be mild, and in some cases, they are discovered incidentally during routine blood tests. Diagnosis to treatment initiation may take weeks to months, especially in early stages when a “watch and wait” approach is sometimes used. However, if symptoms worsen or the disease progresses, treatment is started sooner.
This timeline emphasizes the need for prompt evaluation of persistent symptoms to enable timely intervention, especially in acute leukemia cases.
How to Live with Leukemia?
Managing daily life with leukemia involves practical coping strategies, building support systems, and making lifestyle adjustments. Many patients find that maintaining a balanced diet and engaging in gentle exercise, like walking, helps manage fatigue and boost mood. A study from the American Cancer Society highlights that moderate physical activity can improve energy levels and reduce treatment-related fatigue in leukemia patients.
Support systems are essential, with many patients benefiting from joining support groups or counseling sessions. Connecting with others facing similar challenges can alleviate feelings of isolation and provide emotional relief. Patients often report that support from family, friends, and online communities has been invaluable for managing stress and staying positive.
Stress management techniques, such as mindfulness, meditation, and breathing exercises, can help patients cope with the emotional demands of living with leukemia. Healthcare providers frequently recommend these methods to help manage anxiety and maintain mental resilience.
These strategies, tailored to each patient’s needs, enable individuals to better navigate daily life and maintain quality of life during treatment.
Can Leukemia Be Prevented?
Preventive measures for leukemia include regular health check-ups and blood tests, especially for individuals with family history or known risk factors, to catch any early signs.
Lifestyle changes like avoiding tobacco, minimizing exposure to harmful chemicals (e.g., benzene), and maintaining a healthy diet rich in fruits, vegetables, and whole grains support immune health. Experts recommend regular exercise and stress management to strengthen overall resilience, which may help reduce risks associated with certain cancers.
While there is no guaranteed way to prevent leukemia, these measures support general health and may lower risks, especially when combined with early detection efforts.
Regular Screenings
Regular screenings are crucial for the early detection and effective management of leukemia, especially for those with risk factors. Early detection through routine blood tests can identify abnormal blood cell counts before symptoms arise, leading to faster diagnosis and treatment. Studies show that early-stage detection significantly improves outcomes; for example, early intervention in acute leukemias can enhance treatment success, as rapid treatment initiation is linked to better survival rates. Regular screenings are thus vital in catching leukemia early, improving the chances for successful treatment and extended survival.
Lifestyle and Dietary Changes
Lifestyle and dietary changes can help reduce leukemia risk. Research suggests that avoiding tobacco and limiting exposure to chemicals like benzene can lower the likelihood of developing leukemia. A study from the International Agency for Research on Cancer highlights the link between benzene exposure and increased leukemia risk, emphasizing the importance of minimizing contact with such substances.
Dietary adjustments that emphasize fruits, vegetables, and whole grains support immune health and may offer protective benefits. Additionally, the American Cancer Society recommends regular physical activity, which has been associated with reduced cancer risk and overall immune resilience. While these changes don’t guarantee prevention, they contribute to better general health and may reduce leukemia risk.
To Learn More About Leukemia You can Watch 60+1 question with Leukemia Expert Scott Howard on OncoDailyTV
FAQs
What is leukemia, and how does it affect the body?
Leukemia is a cancer of the blood and bone marrow that disrupts the normal production of white blood cells, leading to a range of health issues, from infection vulnerability to anemia.
What are the main symptoms of leukemia?
Common symptoms include fatigue, frequent infections, bruising or bleeding easily, and unexplained weight loss, though these symptoms can vary by leukemia type.
How is leukemia diagnosed?
Diagnosis usually involves blood tests, bone marrow biopsies, and imaging scans to confirm the presence and type of leukemia cells.
What causes leukemia, and are there known risk factors?
The exact causes are unclear, but factors like exposure to high radiation, certain chemicals, family history, and smoking can increase risk.
Are there different types of leukemia?
Yes, the main types include acute lymphocytic leukemia (ALL), acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL), and chronic myeloid leukemia (CML).
How is leukemia treated?
Treatment depends on the type and stage and may include chemotherapy, radiation therapy, targeted therapy, immunotherapy, or stem cell transplants.
Can lifestyle changes reduce the risk of leukemia?
Avoiding tobacco, minimizing exposure to harmful chemicals, and maintaining a balanced diet and active lifestyle may help lower risk, though these measures don’t guarantee prevention.
What is the survival outlook for leukemia patients?
Survival rates vary by leukemia type and stage, with early detection often improving prognosis. Advances in treatment have significantly increased survival for many types.
How often should at-risk individuals get screened for leukemia?
People with higher risk factors, like a family history of leukemia or certain genetic disorders, should discuss regular screenings with their healthcare provider.
Can leukemia go into remission, and what does that mean?
Yes, remission means there are no detectable leukemia cells after treatment, though ongoing monitoring is needed to catch any recurrence early.
Written by Toma Oganezova, MD