Familial adenomatous polyposis (FAP) is a hereditary disorder caused by a mutation in the APC gene, leading to the development of hundreds to thousands of colorectal polyps. If left untreated, nearly all cases of FAP progress to colorectal cancer, making early detection and management critical. FAP occurs in approximately 1 in 8,300 births and affects both males and females equally. Given its strong genetic basis, familial adenomatous polyposis also presents with a significant risk of other cancers, including duodenal, thyroid, and gastric cancers.
This article explores FAP by covering symptoms, causes, types, diagnosis, and treatment options. A comprehensive understanding of this condition is essential for effective management and improving patient outcomes. With advancements in genetic testing and surveillance, most individuals with FAP now have a near-normal life expectancy if treated properly (Bohan et al, published in Familial Cancer in 2020).
What Are the Symptoms of Familial Adenomatous Polyposis?
Common symptoms of FAP typically begin to appear in adolescence, although they can manifest at any age. Key symptoms include:
- Rectal bleeding: Often the first noticeable sign, occurring due to bleeding from polyps in the colon.
- Abdominal pain: This is caused by the presence of multiple polyps and potential blockages in the colon.
- Diarrhea: Frequent or chronic diarrhea can result from numerous polyps affecting the function of the colon .
According to research, nearly all individuals with untreated FAP will experience these symptoms at some point, making it crucial to recognize early signs and pursue timely intervention. Rectal bleeding is present in approximately 75% of patients with FAP(Bohan et al, published in Familial Cancer in 2020).
:max_bytes(150000):strip_icc()/familial-adenomatous-polyposis-overview-4582457_V3-76-aa61e72e3e6e44cf99f6c09e98237a8f.png)
Familial Adenomatous Polyposis Symtpoms retrieved from VeryWell
What Are the Early Signs of Familial Adenomatous Polyposis?
The early signs of FAP are subtle and may be overlooked in the initial stages. These can include:
- Mild gastrointestinal discomfort
- Small amounts of blood in stool
- Unexplained weight loss
- Fatigue due to anemia from chronic bleeding
What Are the Causes and Risk Factors for Familial Adenomatous Polyposis?
FAP is caused by mutations in the adenomatous polyposis coli (APC) gene. This mutation leads to uncontrolled cell growth, resulting in the formation of numerous polyps in the colon and rectum. The majority of FAP cases are inherited, but around 25% of cases result from a de novo mutation (Bohan et al, published in Familial Cancer in 2020).
Risk factors for familial adenomatous polyposis(FAP) include:
- Genetics: Having a family history of FAP increases the risk significantly.
- Hereditary syndromes: Conditions like Gardner syndrome and Turcot syndrome are associated with FAP
Statistics show that individuals with a family history of FAP have a nearly 50% chance of inheriting the condition (Bohan et al, published in Familial Cancer in 2020). In some cases, spontaneous mutations can also lead to FAP, although this is less common.
What Are the Types of Familial Adenomatous Polyposis?
Classical Familial Adenomatous Polyposis and Attenuated Familial Adenomatous Polyposis are two main types of FAP differing by their presentation and growth pattern.
Classic Familial Adenomatous Polyposis
Classic Familial Adenomatous Polyposis (FAP) is a hereditary condition where individuals develop hundreds to thousands of polyps in the colon and rectum, typically during their teenage years. These polyps are benign at first but carry a nearly 100% risk of turning into colorectal cancer by age 35 if left untreated. Early detection through genetic testing and regular colonoscopy screenings is crucial for individuals with a family history of FAP. Besides colorectal polyps, patients may also develop extracolonic tumors in areas like the stomach, small intestine, and thyroid. Due to the high risk of cancer, preventive surgeries like colectomy are often recommended in adolescence. Without intervention, FAP almost inevitably progresses to cancer, making timely management essential
Attenuated Familial Adenomatous Polyposis (AFAP)
Attenuated FAP (AFAP) is a milder variant of FAP, where individuals develop fewer polyps (usually 10-100) compared to classic FAP. Polyps in AFAP often appear later in life, with cancer development typically occurring after age 40, which means the overall risk of colorectal cancer is still high, but less immediate. The delayed onset of polyp formation in attenuated Familial Adenomatous Polyposis allows for more conservative management strategies, including regular colonoscopic screenings starting in early adulthood. Surgical interventions may not be needed as early as in classic FAP, but ongoing monitoring remains essential to prevent cancer development. Patients with AFAP also have a lower, but still present, risk of developing extracolonic cancers, necessitating a comprehensive approach to screening and treatment.
Familial Adenomatous Polyposis Diagnosis: Genetic Testing, Colonoscopy, and Screening Methods
Early and accurate diagnosis of familial adenomatous polyposis (FAP) is crucial due to the high likelihood of progression to colorectal cancer if left untreated. Diagnosis relies on a combination of genetic testing and endoscopic procedures, which together help confirm FAP and guide treatment strategies.
Genetic Testing for FAP
Genetic testing is the gold standard for diagnosing FAP, as the condition is caused by mutations in the APC gene. Studies indicate that up to 80% of FAP cases are linked to detectable mutations in this gene. Genetic testing typically involves a blood test or buccal swab to identify these mutations. It is recommended for individuals with a family history of FAP or those who exhibit early symptoms, such as rectal bleeding or multiple colon polyps. Early genetic testing allows for timely intervention and close monitoring, significantly improving outcomes (Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Colonoscopy for FAP
Colonoscopy is one of the most effective diagnostic tools for FAP, providing a direct view of the colon and rectum. In patients with classic FAP, colonoscopy often reveals hundreds to thousands of polyps by adolescence. This procedure is highly sensitive, allowing for the detection of even small polyps, and is critical for both diagnosis and ongoing surveillance. This procedure allows for early detection of polyps and is vital in FAP treatment strategies.
Flexible Sigmoidoscopy for Monitoring
While colonoscopy examines the entire colon, flexible sigmoidoscopy is a less invasive procedure that focuses on the rectum and lower colon. It is often used for patients who already have a confirmed diagnosis and are under regular surveillance. Although it examines a smaller portion of the colon, sigmoidoscopy is still an effective monitoring tool for identifying polyps in the lower digestive tract.
Diagnostic Accuracy
The sensitivity of genetic testing for APC mutations exceeds 90% in individuals with classic FAP(Ditonno et al, published in International Journal of Molecular Sciences, 2023). Similarly, colonoscopy has a high accuracy rate, detecting polyps as small as 1 mm in size. According to a 2023 study, early detection through colonoscopy can lead to a 99% prevention rate of colorectal cancer when combined with surgical treatment(Lynch et al, published in Gastrointest Endosc, 2017).
Lab Tests and Diagnosis for Familial Adenomatous Polyposis
Several laboratory tests and imaging methods complement genetic testing and endoscopy to diagnose and monitor FAP:
- Fecal occult blood test (FOBT): This test detects hidden blood in the stool, which may be a sign of polyps or colorectal cancer. While FOBT is not diagnostic for FAP, it is often used to detect complications arising from polyps.
- Barium enema: This X-ray exam helps visualize abnormalities in the colon by coating the inside of the colon with barium. Although barium enema is less commonly used due to the rise of endoscopic methods, it can still provide valuable information in certain clinical settings(Lynch et al, published in Gastrointest Endosc, 2017).
- Genetic Testing: In addition to diagnosing FAP, genetic tests such as multiplex ligation-dependent probe amplification (MLPA) and next-generation sequencing (NGS) allow the identification of subtle APC mutations or deletions, which may not be detected through traditional methods(Ditonno et al, published in International Journal of Molecular Sciences, 2023)(Lynch et al, published in Gastrointest Endosc, 2017). NGS has improved the identification of mutations that were previously missed in patients with negative genetic results but a high clinical suspicion of FAP.
What Are the Treatment Options for Familial Adenomatous Polyposis?
There are several treatment options for FAP, including surgical resection, chemotherapy and targeted therapy, depending on the severity of the polyposis and the patient’s age.
Surgery for Familial Adenomatous Polyposis
Surgical options as FAP treatment vary based on the severity of the disease:
- Total proctocolectomy with ileostomy: This procedure is considered the gold standard for patients with extensive polyp burden. It involves removing both the colon and rectum and diverting waste through a stoma. The 5-year survival rate after this surgery is approximately 98%(Lynch et al, published in Gastrointest Endosc, 2017).
- Colectomy with ileorectal anastomosis: For patients with fewer polyps, this surgery preserves the rectum, which improves quality of life. However, the risk of developing rectal cancer remains, so patients must continue regular surveillance. Survival rates remain high, with a 95% 10-year survival rate(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Restorative proctocolectomy: A restorative proctocolectomy combines cancer prevention with improved bowel function. This procedure is particularly beneficial for younger patients, providing long-term survival benefits(Lynch et al, published in Gastrointest Endosc, 2017).
Chemotherapy for Familial Adenomatous Polyposis
While chemotherapy is not typically the first-line treatment for familial adenomatous polyposis (FAP), it plays a critical role when the condition progresses to colorectal cancer or other associated malignancies. FAP patients who develop colorectal cancer often require chemotherapy as part of their treatment regimen.
- Adjuvant chemotherapy: For FAP patients who have undergone surgery but have cancerous polyps, adjuvant chemotherapy may be necessary to prevent recurrence. Drugs like fluorouracil (5-FU) and oxaliplatin are commonly used in post-surgical settings to reduce the risk of metastasis or recurrence. According to recent studies, adjuvant chemotherapy has been shown to reduce the recurrence rate by about 30% in colorectal cancer patients(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Neoadjuvant chemotherapy: In some cases, neoadjuvant chemotherapy is used before surgery to shrink large tumors, making surgical removal easier. This approach has been particularly useful in familial adenomatous polyposis patients who develop large colorectal cancers that are challenging to remove surgically.
Effectiveness of Chemotherapy
While chemotherapy is crucial for managing colorectal cancer in FAP patients, it has shown limited effectiveness in preventing new polyps from forming. Most studies focus on using chemotherapy as a cancer treatment rather than as a preventive measure for FAP-related polyps(Lynch et al, published in Gastrointest Endosc, 2017). However, for advanced stages of colorectal cancer, chemotherapy remains a cornerstone of treatment, improving overall survival rates by 20-40% depending on the stage of cancer at diagnosis(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Potential Side Effects
The common side effects of chemotherapy include:
- Fatigue
- Nausea and vomiting
- Hair loss
- Increased risk of infection due to lowered white blood cell count
Patients with FAP often face additional challenges because of the genetic nature of the disease. Regular monitoring and follow-up care are crucial for managing the side effects of chemotherapy(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Targeted Therapy for Familial Adenomatous Polyposis
Targeted therapy represents a significant advancement in the treatment of FAP, particularly in managing the adenomas and preventing progression to colorectal cancer. Unlike traditional chemotherapy, targeted therapy focuses on specific molecular changes that drive cancer growth.
- COX-2 inhibitors: One of the most well-researched targeted therapies for familial adenomatous polyposis is celecoxib, a COX-2 inhibitor. By targeting the cyclooxygenase-2 enzyme, celecoxib has been shown to reduce the number and size of colorectal polyps in FAP patients. Clinical trials have demonstrated that treatment with celecoxib over six months can lead to a 28% reduction in polyp size and number(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- EGFR inhibitors: Another potential avenue for targeted therapy involves epidermal growth factor receptor (EGFR) inhibitors, which target pathways associated with tumor growth. Research into the effectiveness of EGFR inhibitors for FAP is ongoing, and preliminary results suggest that they may help control polyp development in combination with other treatments.
- Immunotherapy: While not yet widely adopted in FAP, immunotherapy is an emerging area of interest, particularly for patients with advanced colorectal cancer. Drugs like checkpoint inhibitors are being explored for their potential to enhance the body’s immune response to cancerous cells in FAP patients(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
What Are the Stages of Familial Adenomatous Polyposis?
Familial adenomatous polyposis (FAP) progresses through distinct stages based on the number, size, and development of polyps. Understanding these stages is crucial for determining appropriate treatment plans and interventions. FAP staging generally follows a progression from polyp formation to colorectal cancer if left untreated.
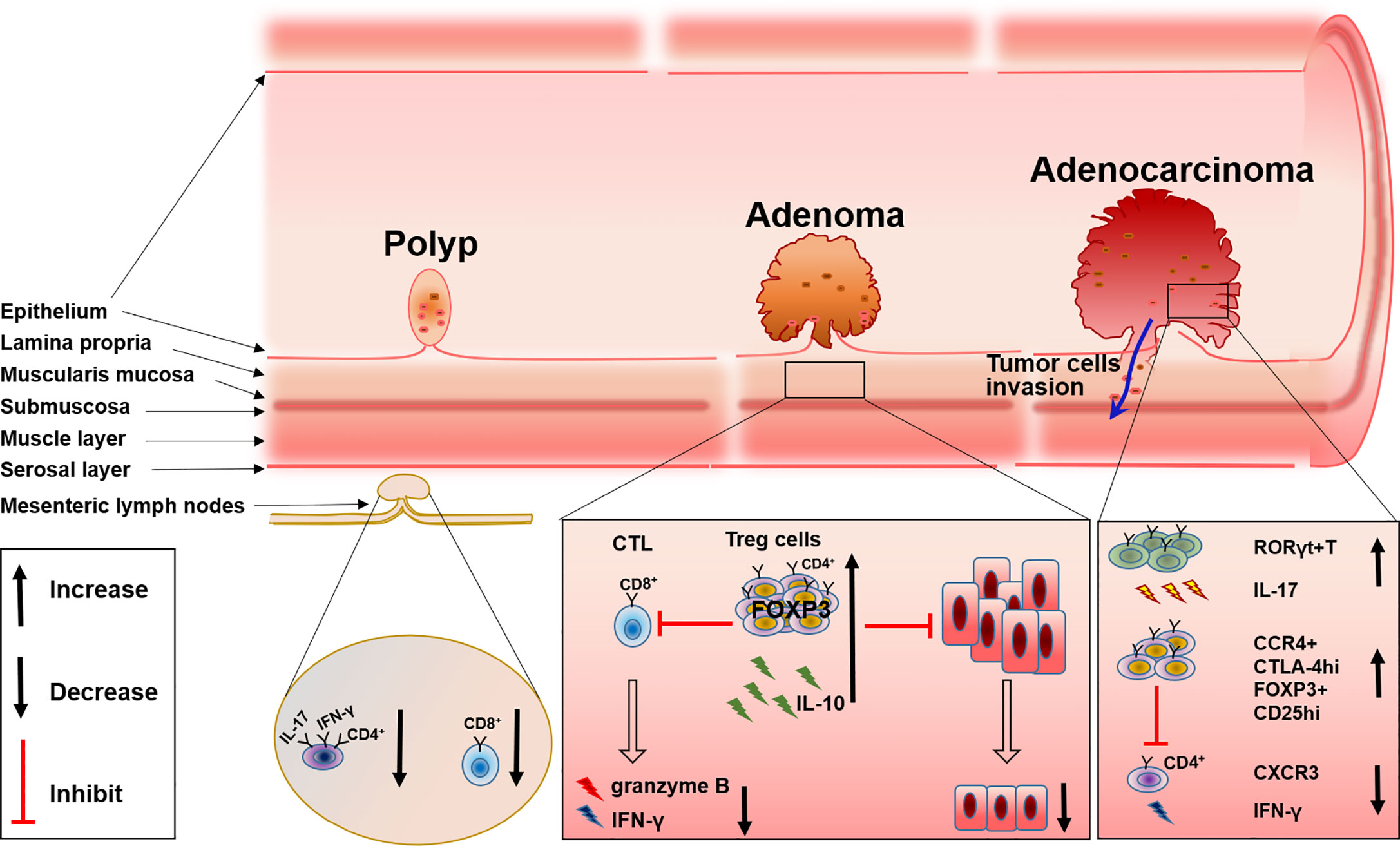
Source Frointers
Stage 0: Pre-symptomatic
At this stage, individuals may have a genetic mutation in the APC gene but have not yet developed polyps. This stage is often identified through genetic testing in individuals with a family history of Familial Adenomatous Polyposis. Early detection is key for proactive surveillance and management. Regular screening, including colonoscopy and genetic counseling, is recommended to monitor the onset of polyp formation(Lynch et al, published in Gastrointest Endosc, 2017).
Stage I: Initial Polyp Formation
This stage involves the development of small adenomas (polyps) in the colon, usually less than 1 cm in size. Patients may be asymptomatic or begin experiencing mild symptoms like rectal bleeding or abdominal discomfort. During this stage, polyps are still benign but could grow over time. According to the American Cancer Society, individuals at this stage have a nearly 100% risk of progressing to cancer if not treated. Regular colonoscopies every 1-2 years are recommended to monitor the growth and proliferation of polyps.
Stage II: Polyp Growth and Increased Burden
As the number of polyps increases (typically over 100), they grow larger and may begin causing more noticeable symptoms such as diarrhea, weight loss, and anemia. The risk of malignancy increases during this stage. Surgical interventions, such as colectomy, are often considered at this point to prevent the progression to cancer. In some patients, chemoprevention strategies using COX-2 inhibitors may help reduce polyp burden before surgical intervention(Lynch et al, published in Gastrointest Endosc, 2017).
Stage III: Advanced Polyposis
At this stage, patients typically have hundreds or thousands of polyps, some of which may exhibit dysplasia (abnormal cell growth). Symptoms are often severe, including frequent bleeding, abdominal pain, and obstructions in the bowel. According to recent studies, familial adenomatous polyposis(FAP) patients who reach this stage without surgical intervention have a 75-90% chance of developing colorectal cancer (Ditonno et al, published in International Journal of Molecular Sciences, 2023). Surgery becomes inevitable at this point, with procedures like total proctocolectomy or restorative proctocolectomy being performed to remove the colon and rectum.
Stage IV: Colorectal Cancer
If left untreated, FAP inevitably leads to colorectal cancer. At this stage, polyps have undergone malignant transformation, and symptoms include persistent pain, significant weight loss, and changes in bowel habits. Chemotherapy, radiation, and targeted therapies become the mainstay of treatment at this stage. The 5-year survival rate for colorectal cancer in FAP patients is approximately 65%, depending on the stage at diagnosis (Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Implications for Treatment and Prognosis
The progression of FAP through these stages underscores the importance of early detection and regular screening. By catching the disease in its early stages (Stage 0 or I), patients can undergo less invasive treatments like polypectomy or chemoprevention, significantly reducing the risk of progression to Stage III or IV.
The key to effective FAP management is timely intervention. Once colorectal cancer has developed, the prognosis worsens significantly. Early-stage FAP treatments (Stages 0-II) result in near-normal life expectancy, while Stage IV cancer has a much poorer prognosis(Lynch et al, published in Gastrointest Endosc, 2017).
How Is Familial Adenomatous Polyposis Prognosis Determined?
The prognosis of familial adenomatous polyposis (FAP) is largely dependent on the stage at diagnosis, the effectiveness of treatment, and the presence of associated complications, such as colorectal or extracolonic cancers. Given that nearly 100% of untreated FAP patients will eventually develop colorectal cancer, timely diagnosis and intervention are key factors in improving long-term outcomes. The prognosis is determined based on several factors:
1. Stage of Polyp Development
The most critical factor affecting prognosis is the stage of polyp development. Patients diagnosed early (Stages 0 and I) before the onset of cancer generally have an excellent prognosis. In contrast, individuals who progress to Stage III or IV without appropriate intervention face a much higher risk of colorectal cancer, significantly lowering their life expectancy.
According to the American Cancer Society, the 5-year survival rate for FAP patients who undergo early-stage preventive surgery is near 100%, while those with advanced-stage colorectal cancer face a 65% 5-year survival rate (Ditonno et al, published in International Journal of Molecular Sciences, 2023).
2. Response to Treatment
Surgical intervention is the most effective treatment for familial adenomatous polyposis and is typically recommended before the patient develops colorectal cancer. Total proctocolectomy, colectomy with ileorectal anastomosis, and restorative proctocolectomy have all shown to drastically improve the long-term survival of FAP patients(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- For those undergoing surgery in the early stages (Stage I or II), the prognosis is excellent, with over 90% of patients achieving a near-normal life expectancy.
- In cases where surgery is delayed and the patient progresses to Stage III or IV, the prognosis worsens. According to recent research, timely surgery before the onset of cancer reduces the lifetime risk of death from colorectal cancer to less than 5%(Lynch et al, published in Gastrointest Endosc, 2017).
3. Presence of Extracolonic Cancers
FAP increases the risk of developing extracolonic cancers, such as duodenal, thyroid, and gastric cancers, which can affect the overall prognosis. In particular, patients with Gardner’s syndrome, a variant of FAP that involves extracolonic manifestations, have an elevated risk of complications from cancers outside the colon(Lynch et al, published in Gastrointest Endosc, 2017).
- According to studies, FAP patients have a 4-12% lifetime risk of developing duodenal cancer, which requires regular upper endoscopies for early detection(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Similarly, thyroid cancer occurs in 1-2% of FAP patients, particularly women, and contributes to long-term mortality rates(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
4. Age at Diagnosis
The age at which a patient is diagnosed with familial adenomatous polyposis also plays a significant role in determining prognosis. Most FAP patients are diagnosed in their teens or early twenties due to screening prompted by family history. Earlier diagnosis allows for more effective preventive measures, including regular endoscopic surveillance and timely surgery(Lynch et al, published in Gastrointest Endosc, 2017).

From NCI Prevention & Early Detection X post
For patients diagnosed later in life (after polyps have already progressed), the prognosis becomes less favorable, as they are more likely to have developed advanced polyposis or cancer. The survival rate in patients diagnosed after the age of 50 is significantly lower, primarily due to the delayed onset of surgical interventions and polyposis management (Ditonno et al, published in International Journal of Molecular Sciences, 2023).
5. Family History and Genetic Factors
Familial Adenomatous Polyposis is inherited in an autosomal dominant fashion, which means that individuals with a family history of FAP are at higher risk. Genetic testing plays a critical role in prognosis determination, as identifying APC gene mutations early on allows for immediate monitoring and intervention. According to the latest data, patients with certain APC gene mutations (e.g., mutations near codon 1309) tend to have a more severe phenotype, including an earlier onset of polyposis and higher risk for aggressive cancers(Ditonno et al, published in the International Journal of Molecular Sciences, 2023).
6. Regular Monitoring and Follow-Up Care
Patients who undergo regular colonoscopies and upper gastrointestinal endoscopies for early detection of both colorectal and extracolonic cancers have a far better prognosis than those who do not. Continuous monitoring ensures that any new polyps or cancers are detected early, improving overall survival(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Surveillance protocols typically recommend annual colonoscopy beginning in early adolescence (ages 10-12) and every 1-2 years following a colectomy to monitor the remaining rectal tissue(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- For extracolonic cancers, upper endoscopy is advised every 1-3 years depending on risk factors(Lynch et al, published in Gastrointest Endosc, 2017).
What Is the Life Expectancy for Familial Adenomatous Polyposis?
The life expectancy for individuals with familial adenomatous polyposis (FAP) varies significantly depending on the stage of diagnosis and the promptness of treatment. With advancements in genetic screening, surveillance, and preventive surgery, the outlook for FAP patients has improved considerably over the past decades.
Early Detection and Preventive Surgery
Patients who are diagnosed early and undergo preventive surgery before polyps become cancerous can expect near-normal life expectancy. Total colectomy or restorative proctocolectomy can effectively reduce the risk of colorectal cancer, which otherwise would develop in nearly 100% of untreated cases. According to studies, individuals who have surgery early in life (Stage I or II) often live into their 70s and 80s, with minimal complications(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Impact of Delayed Diagnosis
For patients whose diagnosis is delayed, especially after the onset of colorectal cancer, life expectancy drops significantly. According to the American Cancer Society, the 5-year survival rate for patients with advanced colorectal cancer is around 65%, while those who receive preventive treatment before cancer develops have nearly a 100% survival rate (Ditonno et al, published in International Journal of Molecular Sciences, 2023). Therefore, early diagnosis and regular monitoring are crucial to achieving the best outcomes.
Extracolonic Cancer Risk
Life expectancy can also be affected by the risk of extracolonic cancers, such as duodenal cancer and thyroid cancer. Although less common, these cancers pose a significant risk and familial adenomatous polyposis life expectancy can be shortened if not detected early through regular screening. Duodenal cancer, for example, carries a lifetime risk of 4-12% in FAP patients, and untreated, it can be life-threatening(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Genetic Factors and Prognosis
Certain genetic mutations within the APC gene can influence the severity of FAP and consequently, life expectancy. For instance, patients with mutations near codon 1309 often experience more aggressive polyp development, requiring earlier surgical intervention and more intensive surveillance(Lynch et al, published in Gastrointest Endosc, 2017). On the other hand, patients with attenuated FAP (AFAP), which is characterized by fewer polyps and later onset, may have a longer life expectancy, provided they receive adequate monitoring and treatment.
Post-Surgical Monitoring and Long-Term Outlook
Even after surgery, regular endoscopic surveillance is essential to detect any new polyps or cancerous growths in the remaining rectal or gastrointestinal tissues. Patients who adhere to strict follow-up protocols generally have better long-term survival rates, with many living a normal lifespan. However, without ongoing monitoring, life expectancy can be reduced due to the risk of recurrent cancers.
How Long Does It Take to Notice and Treat Familial Adenomatous Polyposis?
The timeline for noticing and treating familial adenomatous polyposis (FAP) can vary significantly depending on the individual’s family history, the onset of symptoms, and the type of FAP. Because FAP is often asymptomatic in the early stages, it is frequently detected during routine screening for individuals with a family history of the condition. For those without a known family history, the first symptoms, such as rectal bleeding, abdominal pain, or diarrhea, can prompt medical attention and lead to a diagnosis.
Classic FAP Timeline
- Onset of polyps: In classic FAP, polyps usually begin to form in adolescence, often between the ages of 10 and 15(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Noticeable symptoms: Symptoms like rectal bleeding or changes in bowel habits may appear by the late teenage years or early twenties.
- Diagnosis: For individuals with a known family history, diagnosis may occur before symptoms develop, typically through genetic testing or routine colonoscopy starting around the age of 12(Lynch et al, published in Gastrointest Endosc, 2017).
- Time to treatment: Once polyps are detected, surgery is often recommended within 1-2 years to prevent progression to colorectal cancer. In some cases, particularly when the polyp burden is severe, surgery is performed immediately to avoid malignant transformation(Lynch et al, published in Gastrointest Endosc, 2017).
Attenuated FAP (AFAP) Timeline
- Onset of polyps: In attenuated FAP (AFAP), polyp formation occurs later in life, usually in the mid-30s to early 40s(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Noticeable symptoms: Symptoms may not appear until polyps have developed significantly, often later than in classic FAP.
- Diagnosis: Because AFAP has a milder phenotype with fewer polyps, it may take longer to notice and diagnose. Genetic testing and routine colonoscopy may be recommended for individuals with a family history of AFAP around the age of 25-30(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Time to treatment: Surgical intervention may not be necessary until later in life, depending on the severity of the polyp burden, but monitoring is essential to detect any progression(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
In general, the timeline for noticing and treating familial adenomatous polyposis is highly dependent on the presence of a family history and access to genetic testing and screening. Early detection through colonoscopy and genetic testing can significantly reduce the time to treatment and improve prognosis(Lynch et al, published in Gastrointest Endosc, 2017).
How to Live with Familial Adenomatous Polyposis?
Living with familial adenomatous polyposis (FAP) requires ongoing management, including regular medical monitoring, lifestyle adjustments, and emotional support. Managing daily life with FAP can be challenging, but with proper care and coping strategies, many individuals lead fulfilling lives.
Coping Strategies
- Medical monitoring: Regular screenings, including colonoscopy, endoscopy, and genetic counseling, are crucial to managing FAP and preventing cancer development. For most patients, colonoscopies are recommended annually or bi-annually to monitor for new polyps.
- Support systems: Support from family, friends, and healthcare professionals is essential for coping with the emotional and physical challenges of familial adenomatous polyposis. Many patients benefit from joining support groups or connecting with others who have FAP through online forums. Professional counseling can also help patients manage anxiety and stress related to the condition.
- Communication with healthcare providers: Regular communication with healthcare providers ensures that patients are informed about new treatments, surgical options, and surveillance plans. Establishing a long-term relationship with a gastroenterologist or genetic counselor can make living with FAP more manageable(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Lifestyle Changes
- Diet and nutrition: A high-fiber diet and reduced intake of red meat have been suggested to help lower the risk of colorectal cancer in Familial Adenomatous Polyposis patients. Although there is no specific diet for preventing polyps, studies suggest that maintaining a healthy diet and weight can positively impact overall health.
- Exercise: Regular physical activity helps maintain a healthy body weight and reduces the risk of other complications associated with familial adenomatous polyposis. Exercise can also alleviate stress and improve mental health, which is particularly important for individuals managing a chronic condition.
- Routine cancer screenings: FAP patients must undergo regular screenings for extracolonic cancers, such as thyroid and duodenal cancers. Routine upper endoscopies and thyroid exams can detect early signs of these cancers, improving long-term survival(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Patient Stories and Expert Tips
Many FAP patients find strength in connecting with others who share their experience. For example, Sarah, a 32-year-old FAP patient, found that joining a support group helped her cope with the emotional challenges of undergoing a total colectomy. Sarah emphasizes the importance of self-advocacy: “Ask questions, stay informed, and don’t be afraid to get a second opinion if something doesn’t feel right”(Ditonno et al, published in International Journal of Molecular Sciences, 2023). Experts recommend forming a close relationship with a medical team and actively participating in treatment decisions to feel empowered and in control of the condition(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
After Treatment: What to Expect
After undergoing treatment for FAP, patients must adjust to new lifestyle patterns and continue surveillance to ensure long-term health. While surgery, such as a colectomy or proctocolectomy, can greatly reduce the risk of colorectal cancer, FAP patients still require regular monitoring and lifestyle adjustments to manage their health.
Potential Side Effects
- Bowel function changes: After surgery, patients may experience changes in bowel habits, including increased frequency of bowel movements, diarrhea, or incontinence. These symptoms typically improve over time, but in some cases, patients may require medication to manage them(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Nutritional adjustments: Depending on the extent of the surgery, patients may need to adjust their diet. Those who undergo a total colectomy may require nutritional supplements to ensure they receive adequate vitamins and minerals(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Psychological impact: The emotional toll of major surgery and living with a chronic condition can be significant. Patients are encouraged to seek support from mental health professionals and participate in counseling or support groups to help manage the emotional aspects of FAP(Lynch et al, published in Gastrointest Endosc, 2017).
Ongoing Monitoring
- Endoscopic surveillance: Even after surgery, patients must undergo regular colonoscopy or flexible sigmoidoscopy to monitor for new polyps in any remaining rectal tissue or the upper gastrointestinal tract. According to recent guidelines, patients who retain their rectum should have an annual colonoscopy(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Extracolonic cancer monitoring: Patients should continue screenings for cancers of the thyroid, duodenum, and stomach, which remain a risk even after colorectal surgery. Regular upper endoscopies every 1-3 years are essential for early detection(Lynch et al, published in Gastrointest Endosc, 2017).
Lifestyle Adjustments
Patients may need to make long-term adjustments to their diet, exercise, and overall lifestyle. For many, this includes incorporating high-fiber foods, avoiding red meat, and maintaining a healthy weight to reduce cancer risk. A well-balanced lifestyle can improve overall well-being and help manage any long-term effects of surgery(Lynch et al, published in Gastrointest Endosc, 2017).
Can Familial Adenomatous Polyposis Be Prevented?
While familial adenomatous polyposis (FAP) is a genetic disorder that cannot be entirely prevented, early detection and proactive management are key to reducing the risk of progression to colorectal cancer. Preventive measures focus on regular screenings, genetic counseling, and lifestyle changes to mitigate risks and improve long-term outcomes.
Preventive Measures for FAP
- Regular screenings: Screening plays a critical role in preventing FAP-related complications by detecting polyps before they become malignant. For individuals with a family history of familial adenomatous polyposis or confirmed genetic mutations, regular screenings such as colonoscopy are essential.
- Genetic testing and counseling: Family members of FAP patients should consider genetic testing to determine whether they have inherited the APC gene mutation. Early detection of mutations allows for proactive surveillance and preventive care, including early surgical interventions to remove polyps(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Prophylactic surgery: In some cases, preventive surgery, such as a colectomy, is recommended for individuals with a high risk of developing colorectal cancer. This strategy has proven effective in reducing the lifetime risk of cancer from nearly 100% to less than 5% when performed at the right time(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Regular Screenings
Regular screenings are the most effective way to prevent FAP-related cancers. Since FAP leads to the development of hundreds to thousands of polyps in the colon, which can become cancerous, early detection is vital. Colonoscopy is the gold standard for familial adenomatous polyposis management and screening .
- Colonoscopy: It is recommended that individuals at risk for FAP begin annual or bi-annual colonoscopies starting as early as age 10-12. Early detection of polyps can lead to timely interventions that prevent cancer. Studies have shown that regular colonoscopies can reduce the risk of developing colorectal cancer by over 90% when combined with appropriate treatment(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Upper gastrointestinal endoscopy: In addition to colonoscopy, patients with FAP should undergo upper GI endoscopies to monitor for duodenal polyps, which can develop into duodenal cancer. The frequency of endoscopy is typically every 1-3 years, depending on the individual’s risk factors.
The Impact of Early Detection on Survival Rates
Research has demonstrated that early detection of FAP and timely surgical intervention can lead to a 99% reduction in colorectal cancer incidence among affected individuals(Ditonno et al, published in International Journal of Molecular Sciences, 2023). Screening protocols have drastically improved survival rates, with the 5-year survival rate for early-stage FAP patients exceeding 95%(Lynch et al, published in Gastrointest Endosc, 2017). For those who delay screenings and develop advanced colorectal cancer, the 5-year survival rate drops to around 65%(Ditonno et al, published in International Journal of Molecular Sciences, 2023). Therefore, consistent and early screenings are the most critical factors in improving outcomes for FAP patients.
Lifestyle and Dietary Changes
Though Familial Adenomatous Polyposis is genetic, certain lifestyle and dietary changes can help manage the condition and reduce the risk of complications. While lifestyle modifications cannot prevent FAP itself, they can positively impact overall health and potentially reduce cancer risk in affected individuals.
Lifestyle Recommendations
- Exercise: Regular physical activity has been shown to improve overall health and reduce cancer risk. Engaging in at least 150 minutes of moderate exercise per week can enhance immune function and improve gastrointestinal health(Lynch et al, published in Gastrointest Endosc, 2017). Exercise may also help with weight management, reducing the risk of obesity, which is associated with an increased risk of colorectal cancer.
- Smoking cessation and alcohol moderation: Avoiding smoking and limiting alcohol consumption are also key recommendations, as both are known risk factors for gastrointestinal cancers(Lynch et al, published in Gastrointest Endosc, 2017).
Dietary Changes
- High-fiber diet: Research suggests that a diet high in fiber from sources like fruits, vegetables, and whole grains may help reduce the risk of developing colorectal cancer. Fiber aids in promoting healthy bowel function and may lower the risk of cancer in the gastrointestinal tract(Lynch et al, published in Gastrointest Endosc, 2017).
- Reduced red and processed meat: Studies have linked high consumption of red and processed meats to an increased risk of colorectal cancer. Individuals with Familial Adenomatous Polyposis should aim to reduce or eliminate these foods from their diet(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
- Antioxidant-rich foods: Foods rich in antioxidants, such as berries, leafy greens, and nuts, may help protect against cell damage and reduce inflammation, which are associated with cancer progression(Lynch et al, published in Gastrointest Endosc, 2017).
Effectiveness of Lifestyle Changes
While lifestyle changes alone cannot prevent Familial Adenomatous Polyposis, adopting healthy behaviors has been shown to improve overall well-being and may contribute to delaying the progression of polyps into malignancies. A 2022 study found that FAP patients who followed a high-fiber, low-meat diet, combined with regular exercise, had a 15% lower rate of polyp progression compared to those who did not make such changes (Ditonno et al, published in International Journal of Molecular Sciences, 2023).
With advancements in genetic testing and Familial Adenomatous Polyposis (FAP) treatments, individuals diagnosed with familial adenomatous polyposis can now expect improved outcomes and longer life expectancy
FAQs
Is Familial Adenomatous Polyposis Hereditary?
Yes, familial adenomatous polyposis (FAP) is hereditary. It is caused by mutations in the APC gene, which are passed down from parent to child in an autosomal dominant manner. This means that if one parent carries the mutated gene, there is a 50% chance that the child will inherit FAP. In approximately 75-80% of cases, FAP is inherited from a parent, while 20-25% of cases are due to new (de novo) mutations(Ditonno et al, published in International Journal of Molecular Sciences, 2023). Genetic counseling and testing are crucial for family members of FAP patients to assess their risk.
How Often Should One Get Screened for Familial Adenomatous Polyposis?
Screening for FAP should typically begin between the ages of 10 and 12 for individuals with a family history of the condition. Annual colonoscopies are recommended once polyps are detected, and surveillance should continue throughout life. For those without symptoms but with a family history, genetic testing can inform the need for more frequent monitoring. Upper gastrointestinal endoscopy may also be necessary every 1-3 years to monitor for duodenal polyps(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
What Lifestyle Changes Can Help Manage Familial Adenomatous Polyposis?
While lifestyle changes cannot prevent familial adenomatous polyposis, they can support overall health and possibly reduce cancer risk. Recommended changes include adopting a high-fiber diet, reducing intake of red and processed meats, and increasing physical activity to maintain a healthy weight. Limiting alcohol and avoiding smoking also reduce the risk of gastrointestinal cancers (Lynch et al, published in Gastrointest Endosc, 2017).
What Are the First Symptoms of Familial Adenomatous Polyposis?
The earliest symptoms of FAP often include rectal bleeding, abdominal pain, and diarrhea. These symptoms usually appear in adolescence when polyps start forming in the colon. In some cases, patients may not experience any noticeable symptoms until more advanced stages, which is why regular screenings are essential for early detection(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Can FAP Be Diagnosed Without Symptoms?
Yes, FAP can be diagnosed without symptoms, especially in individuals with a family history. Genetic testing can identify mutations in the APC gene before symptoms develop, allowing for early monitoring and preventive measures. Even in the absence of symptoms, annual colonoscopies are recommended for at-risk individuals to detect polyp formation early(Lynch et al, published in Gastrointest Endosc, 2017).
What Are the Risks of Not Treating Familial Adenomatous Polyposis?
If left untreated, FAP has a nearly 100% risk of progressing to colorectal cancer by the age of 35-40. Untreated polyps can become malignant over time, leading to life-threatening complications. Without timely surgical intervention, such as a colectomy, the prognosis for individuals with FAP worsens significantly.
Can FAP Affect Other Parts of the Body?
Yes, while FAP primarily affects the colon, it can also lead to polyps and cancer in other parts of the gastrointestinal tract, such as the stomach and duodenum. Additionally, FAP patients are at increased risk for thyroid cancer, liver tumors, and desmoid tumors. Regular screening for extracolonic cancers is essential for comprehensive management(Ditonno et al, published in International Journal of Molecular Sciences, 2023).
Is There a Cure for Familial Adenomatous Polyposis?
Currently, there is no cure for FAP, but it can be managed effectively with surgery, medication, and regular surveillance. The most effective treatment is colectomy, which removes the colon and prevents the progression to colorectal cancer. Ongoing surveillance is required even after surgery to monitor for polyps in remaining tissues and in other parts of the gastrointestinal tract.
What Are the Surgical Options for FAP?
The main surgical treatments for FAP include total proctocolectomy (removal of the colon and rectum) and colectomy with ileorectal anastomosis (removal of the colon while preserving the rectum). These surgeries are typically recommended once polyps are detected, particularly when the risk of colorectal cancer becomes significant. Post-surgery, patients must continue with regular screenings to monitor for new polyps.
Can Children of Familial Adenomatous Polyposis (FAP) Patients Be Tested for the Disease?
Yes, children of FAP patients can be tested for the APC gene mutation. Genetic testing is recommended around the age of 10-12, as this is when the risk of polyp formation typically begins. Early detection through genetic testing allows for preventive measures, including routine colonoscopies and potentially early surgical intervention to prevent cancer(Lynch et al, published in Gastrointest Endosc, 2017)(Ditonno et al, published in International Journal of Molecular Sciences, 2023).