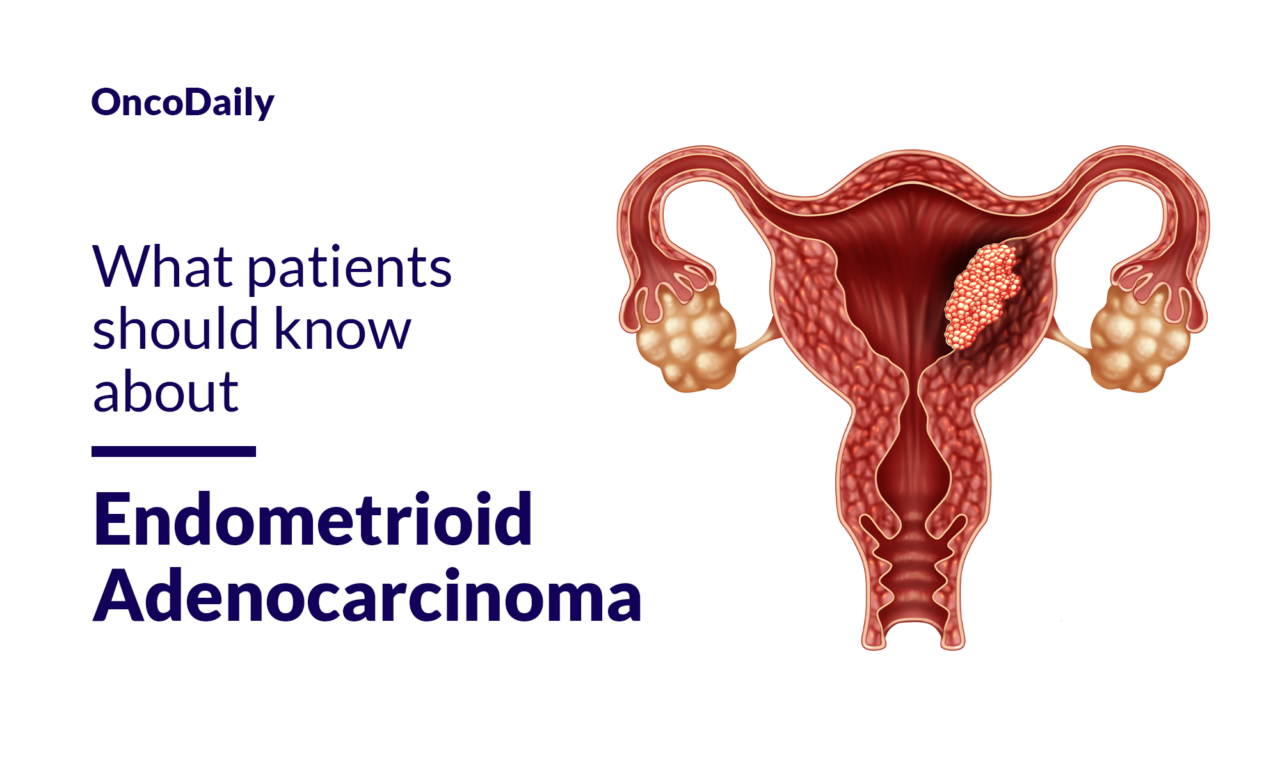
What is Endometrioid Adenocarcinoma?
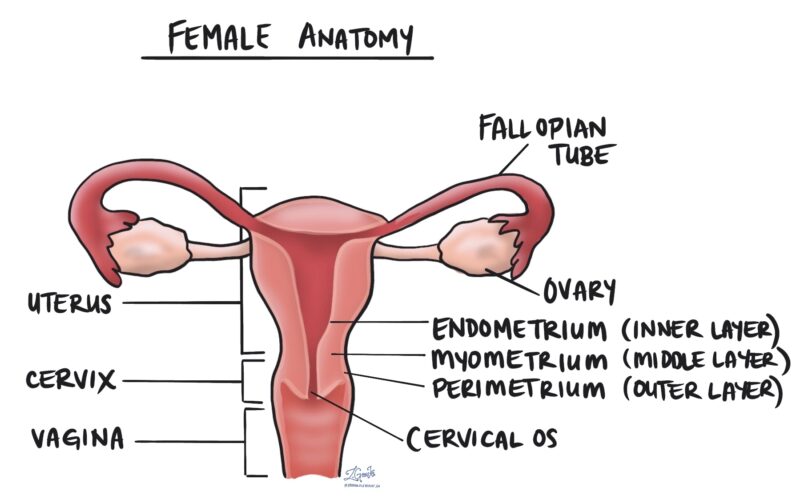
Endometrioid adenocarcinoma is a type of cancer that originates in the glandular tissue of the endometrium, which is the inner lining of the uterus. It is the most common histological subtype of endometrial carcinoma, accounting for 85-90% of cases. This cancer is characterized by the formation of glandular structures that resemble normal endometrial glands but with malignant cells.
Source of image mypathologyreport.ca
Causes and Risk Factors
Hormonal Imbalance
One of the primary factors associated with endometrioid adenocarcinoma is an imbalance between estrogen and progesterone. Estrogen stimulates the growth of the endometrial lining, while progesterone counteracts this effect. When there is an excess of estrogen without sufficient progesterone, the endometrial lining can grow excessively, leading to hyperplasia and potentially cancer.
Obesity
Obesity is a significant risk factor for endometrioid adenocarcinoma. Fat tissue can convert androgens into estrogens, leading to higher levels of estrogen in the body, especially after menopause. This increased estrogen exposure can stimulate the endometrial lining and increase the risk of cancer.
Age and Menstrual History
- Age: The risk of endometrial cancer increases with age, particularly after menopause.
- Early Menarche and Late Menopause: Women who start menstruating before age 12 or enter menopause later than usual have a higher risk due to prolonged exposure to estrogen.
Reproductive History
- Nulliparity: Women who have never been pregnant have a higher risk of endometrial cancer. Pregnancy increases progesterone levels, which helps protect the endometrium.
- Infertility and Polycystic Ovarian Syndrome (PCOS): Conditions that affect ovulation, such as PCOS, can lead to prolonged exposure to estrogen without the balancing effect of progesterone, increasing cancer risk.
Hormone Therapy
- Unopposed Estrogen Therapy: Hormone replacement therapy (HRT) that includes estrogen without progesterone increases the risk of endometrial cancer.
- Tamoxifen: This drug, used to treat breast cancer, can act as an estrogen agonist in the uterus, increasing the risk of endometrial cancer.
Genetic Factors
- Lynch Syndrome: This hereditary condition significantly increases the risk of endometrial cancer, along with other cancers such as colorectal cancer.
- Other Genetic Mutations: Mutations in genes are commonly associated with endometrioid adenocarcinoma.
Lifestyle Factors
- Diet and Physical Activity: A diet high in animal fats and low physical activity levels are associated with an increased risk of endometrial cancer.
- Diabetes and Hypertension: These conditions are linked to an increased risk of endometrial cancer, possibly due to their association with obesity and hormonal imbalances.
Other Factors
- Radiation Exposure: Previous radiation therapy to the pelvis can increase the risk of developing endometrial cancer.
- Family History: A family history of endometrial or colorectal cancer can increase the risk, particularly if associated with genetic syndromes like Lynch syndrome.
Symptoms
Common Symptoms
Abnormal Vaginal Bleeding
- Postmenopausal Bleeding: Any vaginal bleeding after menopause is a significant symptom and should be evaluated by a healthcare provider.
- Bleeding Between Periods: Irregular bleeding or spotting between menstrual cycles can be an early sign of endometrioid adenocarcinoma.
- Heavy or Prolonged Menstrual Bleeding: Extremely heavy, long, or frequent episodes of vaginal bleeding, especially after age 40, can indicate the presence of endometrial cancer.
Pelvic Pain
- Persistent pain or a feeling of heaviness in the pelvic area is a common symptom, particularly as the cancer progresses.
Pain During Intercourse
- Dyspareunia, or pain during sexual intercourse, can be a symptom of endometrioid adenocarcinoma.
Painful or Difficult Urination
- Dysuria, or pain during urination, can occur if the cancer affects the urinary tract.
Abnormal Vaginal Discharge
- Discharge that is unusual in color, consistency, or smell, ranging from pink and watery to thick and brown, can be a symptom of endometrial cancer.
Unintended Weight Loss
- Significant weight loss without trying can be a symptom, especially in more advanced stages of the disease.
Fatigue and Nausea
- General feelings of fatigue and nausea can also be associated with endometrioid adenocarcinoma, particularly as the disease progresses.
Lower Abdominal or Back Pain
- Pain in the lower abdomen or back can occur, especially if the cancer has spread to other organs.
When to See a Doctor
It is crucial to seek medical attention if you experience any of the following:
- Any vaginal bleeding after menopause.
- Bleeding between periods or unusually heavy menstrual bleeding.
- Persistent pelvic pain or a feeling of heaviness in the pelvic area.
- Pain during intercourse or urination.
- Unusual vaginal discharge.
- Unintended weight loss or persistent fatigue.
Diagnosis
Diagnosing endometrioid adenocarcinoma involves a series of tests and procedures to confirm the presence of cancer and determine its extent. Here are the primary diagnostic methods:
Pelvic Examination
- A pelvic exam is often the first step in diagnosing endometrial cancer. During this exam, a healthcare provider checks the reproductive organs for abnormalities by inserting one or two gloved fingers into the vagina while pressing on the abdomen with the other hand. This helps to feel the uterus, ovaries, and other organs for any irregularities.
Transvaginal Ultrasound
- A transvaginal ultrasound uses a wand-like device called a transducer, which is inserted into the vagina. The transducer emits sound waves to create images of the pelvic organs, allowing the healthcare provider to assess the thickness and texture of the endometrium. This test helps in identifying any abnormal growths or changes in the endometrial lining.
Hysteroscopy
- Hysteroscopy involves inserting a thin, flexible, lighted tube called a hysteroscope through the vagina and cervix into the uterus. This allows the healthcare provider to visually examine the inside of the uterus and the endometrium for any abnormalities.
Endometrial Biopsy
- An endometrial biopsy is a crucial diagnostic test where a sample of tissue is removed from the lining of the uterus. This sample is then examined under a microscope to check for cancer cells. The biopsy can often be performed in a healthcare provider’s office and is highly accurate, especially in postmenopausal women.
Dilation and Curettage (D&C)
- If an endometrial biopsy does not provide enough tissue or if the results are unclear, a D&C procedure may be performed. During D&C, tissue is scraped from the lining of the uterus and examined under a microscope for cancer cells. This procedure may require general anesthesia.
Imaging Tests
- Imaging tests such as MRI, CT scans, and PET scans are used to determine the extent of the cancer and whether it has spread to other parts of the body. These tests provide detailed images that help stage the cancer and plan treatment.
Blood Tests
- Blood tests, including a complete blood count (CBC) and a complete metabolic panel (CMP), may be performed to assess the patient’s overall health and detect any abnormalities. Additionally, a CA 125 test may be used, as endometrial cancers sometimes release this substance into the blood.
Genetic Testing
- If there is a suspicion of hereditary non-polyposis colon cancer (HNPCC) as an underlying cause, the tumor cells can be tested for specific protein and gene changes. This includes testing for defects in mismatch repair genes (dMMR) and high levels of microsatellite instability (MSI-H).
Staging*
Once endometrioid adenocarcinoma is diagnosed, staging is performed to determine the extent of the cancer. Staging involves a combination of physical exams, imaging tests, and sometimes surgical procedures to assess how far the cancer has spread. The staging system used is typically the FIGO (International Federation of Gynecology and Obstetrics) system or the TNM (Tumor, Node, Metastasis) system.
*Cancer staging is the process of determining the extent to which a cancer has grown and spread. A number from I to IV is assigned, with I being an isolated cancer and IV being a cancer that has metastasized and spread from its origin.
Treatment
Stage I Endometrioid Adenocarcinoma
- Surgery: The primary treatment for stage I endometrioid adenocarcinoma is surgery, which typically involves a total hysterectomy (removal of the uterus) and bilateral salpingo-oophorectomy (removal of both fallopian tubes and ovaries). Lymph node dissection may also be performed to check for cancer spread.
- Radiation Therapy: For higher-grade* tumors, radiation therapy may be recommended after surgery. This can include vaginal brachytherapy (VB), pelvic radiation, or both.
- Fertility-Sparing Treatment: For young women with stage IA grade 1 endometrioid cancers who wish to preserve fertility, progestin therapy may be used to treat the cancer temporarily. This approach requires close monitoring with regular biopsies and is considered experimental.
*Tumor grade describes how normal or abnormal cancer cells look under a microscope. The higher the grade, the more abnormal the cells look and the faster it is likely to grow and spread.
Stage II Endometrioid Adenocarcinoma
- Surgery: Treatment usually involves a hysterectomy, removal of the fallopian tubes and ovaries, and removal of surrounding tissues and lymph nodes. The upper portion of the vagina may also be removed.
- Radiation Therapy: Postoperative radiation therapy is often recommended to eliminate any remaining cancer cells.
- Chemotherapy: In some cases, chemotherapy may be added, especially for high-grade cancers.
Stage III Endometrioid Adenocarcinoma
- Surgery: If the cancer has spread beyond the uterus but is still operable, surgery is performed to remove as much of the cancer as possible, including the uterus, fallopian tubes, ovaries, and lymph nodes.
- Radiation Therapy and Chemotherapy: A combination of radiation therapy and chemotherapy is typically used after surgery to target any remaining cancer cells.
Stage IV Endometrioid Adenocarcinoma
- Chemotherapy and Radiation Therapy: For advanced stage IV cancer, surgery may not always be an option. Instead, chemotherapy and radiation therapy are used to manage the disease.
- Hormone Therapy: Hormone therapy may be considered for patients who cannot undergo surgery or radiation therapy.
- Targeted Therapy and Immunotherapy: These treatments may be used for advanced or recurrent endometrial cancer. Targeted therapies like mTOR inhibitors and monoclonal antibodies targeting various proteins are options, as well as immunotherapy agents like immune checkpoint inhibitors.
Recurrent Endometrioid Adenocarcinoma
- Surgery: If the cancer recurs locally and is operable, surgery may be performed to remove the recurrent tumor.
- Radiation Therapy and Chemotherapy: These treatments are often used to manage recurrent cancer, especially if surgery is not an option.
- Hormone Therapy and Targeted Therapy: These therapies may be used for recurrent disease, particularly in cases where the cancer is hormone receptor-positive or has specific genetic mutations.
The treatment of endometrioid adenocarcinoma is highly individualized and depends on the stage of the cancer, the patient’s overall health, and other factors. Surgery is the cornerstone of treatment for early-stage disease, often followed by radiation therapy and/or chemotherapy for higher-risk cases. Advanced and recurrent cancers may require a combination of chemotherapy, radiation therapy, hormone therapy, targeted therapy, and immunotherapy. Fertility-sparing options are available for select patients but require careful monitoring and are not considered standard care.
Common side effects of treatment include
Surgery
- Menopause Symptoms: Women who have a hysterectomy and removal of the ovaries will experience immediate menopause, which can cause hot flashes and other menopausal symptoms that may be more severe than natural menopause.
- Impact on Sexual Intimacy: A hysterectomy can affect sexual intimacy, causing changes in sexual function and desire.
Radiation Therapy
- Fatigue: A common side effect that can become severe after a few weeks of treatment.
- Gastrointestinal Issues: Nausea, vomiting, diarrhea, and other digestive problems are common.
- Vaginal Symptoms: Dryness, itching, tightening, and burning in the vagina, which can affect sexual activity.
- Skin Changes: Redness, peeling, blistering, and potential infections in the treated area.
- Bladder and Bowel Irritation: Radiation cystitis (bladder irritation) and radiation proctitis (rectal irritation) can occur, causing discomfort and bleeding.
Chemotherapy
- Nausea and Vomiting: Common side effects that can often be managed with medication.
- Hair Loss: Temporary hair loss is a frequent side effect.
- Fatigue: Feeling tired is a common issue during chemotherapy.
- Mouth and Vaginal Sores: Sores can develop in the mouth and vagina, causing discomfort.
- Blood Cell Count Changes: Low white blood cells (increased infection risk), low red blood cells (anemia), and low platelets (increased bleeding risk).
Hormonal Therapy
- Fluid Retention and Weight Gain: Common side effects of progesterone therapy.
- Menstrual Changes: Women who are still menstruating may experience changes in their periods.
Immunotherapy
- Fatigue: A common side effect of PD-1 (checkpoint) inhibitors.
- Skin Reactions: Rash and itching are frequent.
- Gastrointestinal Issues: Diarrhea is a common side effect
Prognosis and Survivorship
Endometrioid adenocarcinoma, a common type of endometrial cancer, generally has a good prognosis, especially when caught early. Regular follow-up visits are crucial to monitor for recurrence, especially in the first few years after treatment. Survivors may experience anxiety and need emotional support, but many report a good quality of life after recovery.
Watch Wendy’s survivor story from Cancer Center with endometrioid adenocarcinoma.
Survivorship Challenges
Quality of Life (QOL)
- Impact of Disease Grade: Survivors of high-grade endometrioid adenocarcinoma report significantly lower QOL compared to those with low-grade disease. This difference is primarily due to lower physical and functional well-being.
- Long-Term Symptoms: More than seven years after treatment, patients who underwent external beam radiation therapy (EBRT) reported persistent bowel and urinary symptoms that affected daily activities, although these did not significantly impact overall QOL.
Physical Health
- Recurrence and Survival: The risk of recurrence varies by stage and grade, with higher recurrence rates associated with advanced stages and higher grades. Recurrence significantly decreases survival rates.
- Secondary Cancers: Survivors are at increased risk for developing secondary cancers, particularly after treatments like EBRT, which can increase the risk of cancers in the irradiated field.
Lifestyle and Health Behaviors
- Obesity and Inactivity: Many endometrial cancer survivors are overweight or obese, have poor diets, and are physically inactive. These factors are linked to worse QOL and increased morbidity.
- Exercise and Weight Management: Regular physical activity and maintaining a healthy weight are crucial for improving QOL and reducing the risk of recurrence, but many survivors struggle to adopt these lifestyle changes.
Emotional and Psychological Support
- Anxiety and Depression: Survivors often experience anxiety and depression related to the fear of recurrence. Emotional support from family, friends, support groups, and professional counselors is essential for managing these feelings.
Follow-up Care
Follow-up care is a crucial aspect of managing endometrioid adenocarcinoma after the completion of primary treatment. The primary goals of follow-up care are to monitor for cancer recurrence, manage any long-term side effects of treatment, and provide psychosocial support. Here are the key components and strategies for follow-up care:
Frequency and Type of Follow-Up Visits
- Initial Follow-Up: The first check-up typically occurs about 4 to 6 weeks after treatment ends.
- Regular Follow-Up Schedule: For most women, follow-up visits are recommended every 3 to 6 months for the first 2 to 3 years, then every 6 to 12 months thereafter. This schedule may vary based on the stage and grade of the cancer.
- High-Risk Patients: Women with higher stage or grade cancers (e.g., stages III or IV, or grade III cancers) may require more frequent follow-ups, including CT scans of the chest, abdomen, and pelvis every 6 months for the first 3 years, then every 6 to 12 months for at least the next 2 years.
Components of Follow-Up Care
- Physical Examination: Each visit typically includes a pelvic exam to check for any signs of recurrence, as well as an assessment of the patient’s overall health and any new symptoms.
- Imaging and Tests: Imaging tests (such as CT scans or ultrasounds) and blood tests (such as CA 125) may be performed based on symptoms or physical exam findings, but routine use of these tests in asymptomatic patients is not generally recommended.
- Patient-Initiated Follow-Up (PIFU): Some follow-up care models allow patients to initiate appointments based on their symptoms or concerns, which can help tailor care to individual needs and reduce unnecessary visits.
Managing Long-Term Side Effects
- Monitoring and Managing Side Effects: Follow-up care includes monitoring for and managing long-term side effects of treatment, such as fatigue, gastrointestinal issues, and menopausal symptoms.
- Psychosocial Support: Emotional and psychological support is an important part of follow-up care, as many survivors experience anxiety and depression related to the fear of recurrence.
Importance of Adherence to Follow-Up
- Early Detection of Recurrence: Most recurrences are detected based on symptoms reported by the patient, making it crucial for patients to attend all scheduled follow-up appointments and report any new symptoms promptly.
- Patient Education: Patients are educated about the signs and symptoms of recurrence, such as vaginal bleeding, pelvic pain, and unexplained weight loss, and are encouraged to contact their healthcare provider if they notice any of these symptoms.
Transition to Primary Care
- Long-Term Follow-Up: As the need for frequent follow-up decreases, care may be transitioned to a primary care physician or gynecologist, with continued monitoring for late effects of treatment and overall health maintenance
Resources
- American Cancer Society – Cancer.org
- National Cancer Institute – Cancer.gov
- Cancer Research Institute – cancerresearch.org
- Endometrioid endometrial adenocarcinoma in a premenopausal woman with multiple organ metastases – PubMed
- Risk factors for endometrial cancer – PubMed
- Risk factors for endometrial cancer: An umbrella review of the literature – PubMed
- Surgical Management and Postoperative Treatment of Endometrial Carcinoma – PubMed
- Long-term survival of endometrioid endometrial cancer patients – PubMed
- Quality of life in endometrial cancer survivors by grade of disease – PubMed
- Long-Term Impact of Endometrial Cancer Diagnosis and Treatment on Health-Related Quality of Life and Cancer Survivorship: Results From the Randomized PORTEC-2 Trial – PubMed
- Follow‐up strategies for women with endometrial cancer after primary treatment – PubMed