What is Glioblastoma?
Pediatric glioblastoma is a rare and aggressive brain tumor that primarily affects children. It accounts for approximately 3% of all childhood brain tumors and is characterized by rapid growth and a poor prognosis. Despite advances in treatment, the survival rate for pediatric glioblastoma remains low, necessitating a comprehensive understanding of the disease for patients and caregivers.
Prevalence and Epidemiology
Pediatric glioblastoma is a rare and aggressive brain tumor that accounts for approximately 2-3% of all childhood brain tumors. The incidence of pediatric high-grade gliomas, which includes pediatric glioblastoma, is around 0.85 per 100,000 children according to the Central Brain Tumor Registry of the United States (CBTRUS). This tumor represents 3-15% of all primary brain tumors in the pediatric population (0-18 years).
Causes and Risk Factors
The exact cause of pediatric glioblastoma is not well understood. However, several risk factors have been identified:
- Genetic predispositions: Conditions like neurofibromatosis type 1 (NF1), Li-Fraumeni syndrome, and tuberous sclerosis increase the risk of developing pediatric glioblastoma.
- Genetic mutations: Mutations in genes such as TP53, PDGFRA, MYCN, ATRX, and IDH have been implicated in the development of pediatric glioblastoma (these genes are involved in cell cycle regulation, growth, gene expression, chromatin remodeling, and metabolism).
The video is prepared by Ivy Brain Tumor Center.
Symptoms
Symptoms of pediatric glioblastoma can vary depending on the tumor’s location, size, and growth rate. Common symptoms include:
- Headaches: Frequent and severe headaches, often worse in the morning due to increased intracranial pressure when lying down.
- Nausea and Vomiting: Persistent nausea and vomiting, which can be due to increased pressure within the brain.
- Seizures: Seizures can occur depending on the tumor’s location and type. They are a significant symptom that warrants immediate medical attention.
- Vision Changes: Changes in vision, such as double vision, squinting, or covering one eye, can indicate a tumor affecting the visual pathways.
- Balance and Coordination Problems: Difficulty with balance and coordination, often due to tumors near the brainstem or cerebellum.
- Cognitive and Behavioral Changes: Memory problems, confusion, personality changes, and irritability can occur as the tumor affects different brain regions.
- Weakness or Sensory Loss: Weakness or loss of sensation in an arm or leg, or drooping on one side of the face, can indicate the tumor’s impact on motor and sensory pathways.
- Speech and Swallowing Difficulties: Slurred speech and trouble swallowing can be symptoms of a tumor affecting the brain areas responsible for these functions.
- Drowsiness and Lethargy: Increased sleepiness and lethargy, often due to the tumor’s pressure on brain structures.
- Hearing Problems: Hearing loss or changes can occur if the tumor affects the auditory pathways.
- Increased Head Size in Infants: In babies, a fuller soft spot on the skull or an increase in head size can be a sign of a brain tumor.
Diagnosis
Diagnosis of pediatric glioblastoma typically involves a combination of imaging studies and biopsy:
- Magnetic Resonance Imaging (MRI): MRI is the primary imaging modality used to detect and characterize brain tumors. It provides detailed images of the brain and helps determine the tumor’s size, location, and extent.
- Biopsy: A tissue sample is obtained to confirm the diagnosis and determine the tumor’s histological and molecular characteristics. Next-generation sequencing can be used to identify specific genetic mutations that may guide treatment.
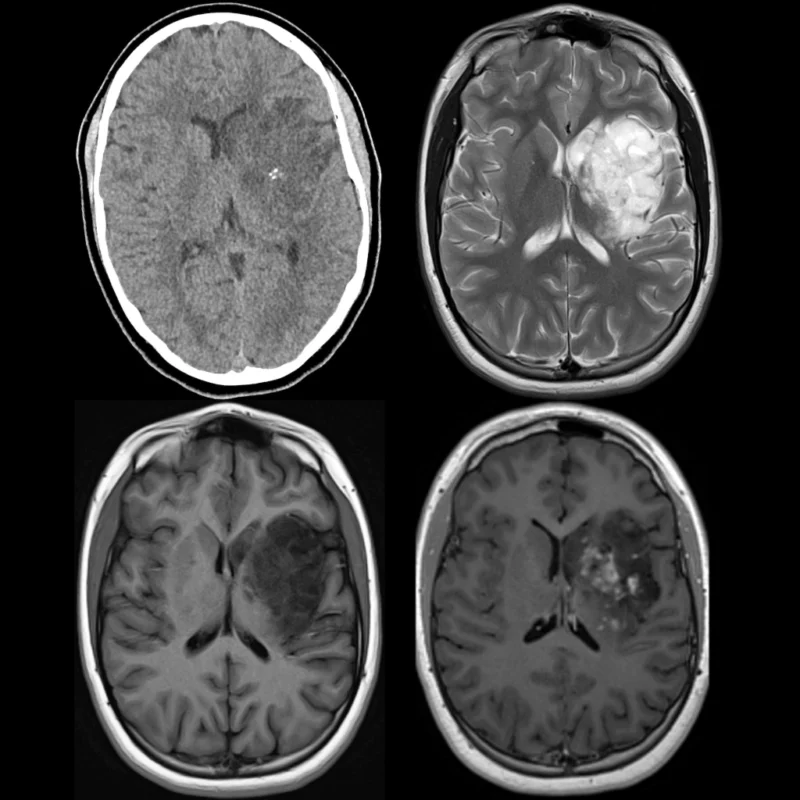
The CT (above left) and MRI scans (with and without contrast) of glioblastoma. The image is taken from pediatricimaging.org.
Treatment Options
Treatment for pediatric glioblastoma involves a multimodal approach, including surgery, radiation therapy, and chemotherapy. Emerging therapies such as targeted molecular therapy and immunotherapy are also being explored.
- Surgery: The primary goal of surgery is to remove as much of the tumor as possible while preserving neurological function. Advanced techniques such as intraoperative MRI and neuronavigation are used to maximize tumor resection. However, complete removal is often challenging due to the tumor’s infiltrative nature.
- Radiation Therapy: Radiation therapy is a cornerstone of pediatric glioblastoma treatment. Techniques such as proton therapy and stereotactic radiosurgery allow for precise targeting of the tumor, minimizing damage to surrounding healthy tissue. Radiation therapy is typically administered postoperatively to control local tumor growth.
- Chemotherapy: Chemotherapeutic agents are often administered concurrently with radiation therapy and as adjuvant therapy. However, its efficacy in children is less clear than in adults.
- Targeted Molecular Therapy: Advances in molecular profiling have identified specific genetic mutations and pathways that drive pediatric glioblastoma. Targeted therapies aim to inhibit these pathways. Despite promising preclinical results, targeted therapies have yet to show significant clinical benefit in pediatric glioblastoma patients.
- Immunotherapy: Immunotherapy, including immune checkpoint inhibitors and CAR-T cell therapy, is an emerging area of research in pediatric glioblastoma. These therapies aim to harness the body’s immune system to target and destroy tumor cells. Early-phase clinical trials are ongoing to evaluate their safety and efficacy in pediatric patients.
- Combination Therapy: Given the complexity of pediatric glioblastoma, combination approaches are being explored to target multiple pathways simultaneously, such as:
- Immunotherapy combined with chemotherapy or targeted therapy
- Multi-agent targeted therapy regimens
More information about completed and ongoing clinical trials for pediatric glioblastoma can be found here – clinicaltrials.gov.
Problems During and After Treatment and How to Manage Them
- Cognitive and Psychosocial Effects: Cognitive deficits and psychosocial issues are common in pediatric glioblastoma survivors. These can impact education, professional career, and quality of life. Cognitive rehabilitation, psychological support, and educational interventions are essential components of survivorship care.
- Endocrine and Metabolic Disorders: Endocrine dysfunctions, such as growth hormone deficiency and hypothyroidism, are common due to the effects of radiation therapy. Regular endocrine evaluations and appropriate hormone replacement therapies are necessary to manage these conditions.
- Cardiovascular and Cerebrovascular Complications: Survivors are at increased risk for cardiovascular and cerebrovascular diseases. Regular monitoring, lifestyle modifications, and early interventions are crucial to mitigate these risks.
- Secondary Cancers: The risk of secondary cancers is elevated in pediatric glioblastoma survivors, particularly those who have received radiation therapy. Lifelong surveillance and early detection strategies are important for managing this risk.
Prognosis
The prognosis for pediatric glioblastoma is generally poor, but it can vary based on several factors:
- Extent of Resection: Complete surgical resection of the tumor is associated with significantly better outcomes. Studies have shown that gross total resection correlates with longer overall survival compared to subtotal resection or biopsy alone.
- Adjuvant Therapy: The use of adjuvant therapies such as radiation and chemotherapy can improve survival rates. For instance, the combination of radiation therapy with temozolomide has been shown to enhance survival, although its benefit in children is less clear than in adults.
- Tumor Location and Molecular Characteristics: Tumors located in superficial areas of the brain and those with specific molecular profiles tend to have better prognoses.
Conclusion
Pediatric glioblastoma is undoubtedly a challenging and aggressive disease, but there is hope on the horizon. Advances in medical research and treatment strategies are continually improving our understanding and management of this complex condition. The integration of cutting-edge surgical techniques, innovative radiation therapies, and promising new drugs, including targeted molecular therapies and immunotherapies, offers a beacon of hope for better outcomes.
Moreover, the focus on comprehensive survivorship care ensures that the journey does not end with treatment. Survivors are provided with the necessary support to manage long-term health issues, improve their quality of life, and achieve their personal and professional goals. The dedication of healthcare professionals, researchers, and support networks plays a crucial role in this ongoing battle.
Sources
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- American Brain Foundation
- American Society of Clinical Oncology – asco.org
- Children’s Hospital of Philadelphia – chop.edu
- Dana-Farber Cancer Institute
- Radiopaedia – radiopedia.org
- Novel Pharmacological Treatment Options in Pediatric Glioblastoma—A Systematic Review – Cancers