Introduction
Vulvar cancer is a rare type of cancer that affects the external part of the female genitalia, known as the vulva. This cancer can develop in various parts of the vulva, including the labia majora, labia minora, clitoris, and Bartholin’s glands. Understanding the causes, risk factors, symptoms, diagnosis, prevention, treatment options, and survivorship challenges is crucial for patients and their families.
Causes and Risk Factors
Causes
Vulvar cancer occurs when cells in the vulva undergo abnormal changes and begin to grow uncontrollably. These changes are often due to mutations in the DNA of the cells, which can be triggered by various factors.
Risk Factors
Several factors can increase the risk of developing vulvar cancer:
- Human Papillomavirus (HPV) Infection: HPV is a sexually transmitted virus that can cause changes in the cells of the vulva, leading to cancer. High-risk strains of HPV, such as types 16 and 18, are particularly associated with vulvar cancer.
- Age: The risk of vulvar cancer increases with age, with most cases occurring in women over 50.
- Smoking: Smoking can damage the DNA of cells and weaken the immune system, making it harder for the body to fight off infections like HPV.
- Immune System Deficiency: Conditions that weaken the immune system, such as HIV infection or immunosuppressive medications, can increase the risk of vulvar cancer.
- Precancerous Conditions: Conditions like vulvar intraepithelial neoplasia (VIN) and lichen sclerosus can increase the risk of vulvar cancer. VIN involves abnormal cell growth on the surface of the vulva, while lichen sclerosus causes thinning and itching of the vulvar skin.
- Other Cancers: A history of cervical or vaginal cancer can increase the risk of vulvar cancer due to shared risk factors like HPV infection.
Subtypes of Vulvar Cancer
Vulvar cancer can be classified into several subtypes based on the type of cells where the cancer begins:
- Squamous Cell Carcinoma: This is the most common type, accounting for about 90% of vulvar cancers. It starts in the thin, flat cells lining the surface of the vulva.
- Vulvar Melanoma: This type starts in the pigment-producing cells of the vulva and is less common.
- Basal Cell Carcinoma: A rare type that starts in the basal cells of the skin.
- Adenocarcinoma: This type begins in the glandular cells of the vulva, such as those in the Bartholin’s glands.
- Sarcoma: A rare type that starts in the connective tissues of the vulva.
Symptoms
Itching and Burning – Persistent itching and burning in the vulvar area are common symptoms of vulvar cancer. These symptoms occur because the cancerous cells can cause inflammation and irritation of the skin.
Lumps and Bumps – The presence of lumps, bumps, or wart-like growths on the vulva can indicate vulvar cancer. These growths result from the abnormal proliferation of cancerous cells.
Skin Changes Changes – in the color or texture of the vulvar skin, such as thickened, raised patches, can be a sign of vulvar cancer. These changes occur because the cancer cells alter the normal structure and function of the skin.
Pain and Soreness – Pain or soreness in the vulvar area, especially during urination or sexual intercourse, can be a symptom of vulvar cancer. This pain is due to the invasion of cancer cells into the surrounding tissues, causing inflammation and damage.
Bleeding and Discharge – Unusual bleeding or discharge from the vulva, not related to the menstrual cycle, can be a sign of vulvar cancer. This occurs because the cancerous growths can disrupt the normal blood vessels and glands in the vulva.
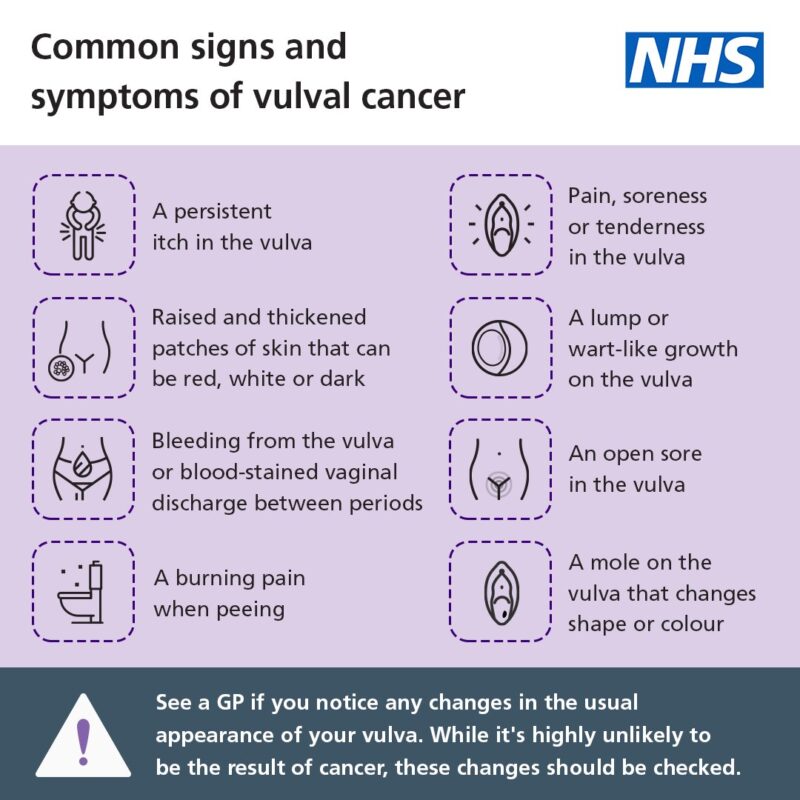
This image is taken from nhs.uk
Diagnosis
Physical Examination
A thorough physical examination of the vulva may be performed to check for any abnormalities, such as lumps, sores, or changes in skin color and texture.
Biopsy
A biopsy involves taking a small sample of tissue from the suspicious area of the vulva. This sample is then examined under a microscope to check for cancerous cells.
Imaging Tests
Imaging tests, such as CT scans, MRI scans, and PET scans, may be used to determine the extent of the cancer and whether it has spread to other parts of the body.
Colposcopy
Colposcopy is a procedure that uses a special magnifying device to closely examine the vulva, vagina, and cervix for any abnormal areas. If any suspicious areas are found, a biopsy may be performed.
Prevention
HPV Vaccination
The HPV vaccine can protect against the high-risk strains of HPV that are associated with vulvar cancer. It is recommended for preteens and young adults, but older individuals can also benefit from the vaccine.
Safe Sexual Practices
Practicing safe sex, such as using condoms and limiting the number of sexual partners, can reduce the risk of HPV infection and, consequently, vulvar cancer.
Regular Gynecological Exams
Regular gynecological exams, including pelvic exams and Pap tests, can help detect precancerous conditions and early-stage vulvar cancer, making treatment more effective.
Quitting Smoking
Quitting smoking can reduce the risk of vulvar cancer and improve overall health. Smoking cessation programs and support groups can help individuals quit smoking.
Prognosis
The prognosis for vulvar cancer depends on several factors, including the stage of the cancer at diagnosis, the type of cancer, and the patient’s overall health. Early-stage vulvar cancer has a better prognosis and is more likely to be successfully treated.
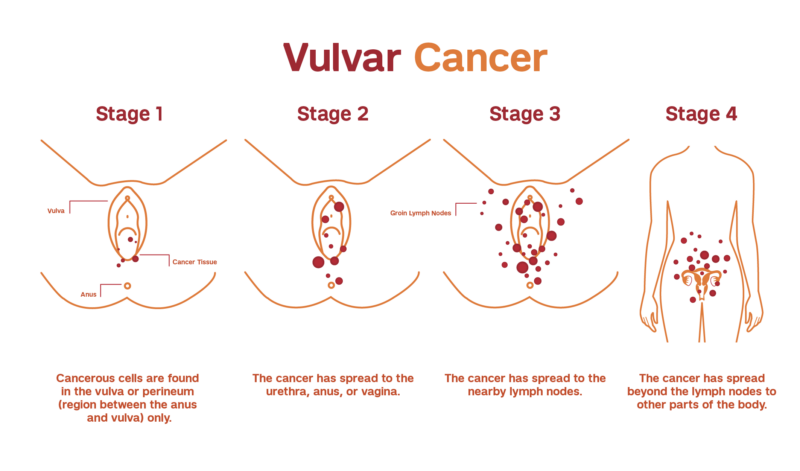
This image is taken from weillcornell.org
Treatment and Side Effects
Surgery
Surgery is the most common treatment for vulvar cancer. The goal is to remove all the cancer while preserving as much normal tissue as possible. Types of surgery include:
- Wide Local Excision: This involves the removal of the cancerous tissue along with a margin of healthy tissue. This margin helps ensure that all cancer cells are removed, reducing the risk of recurrence.
- Vulvectomy: This procedure involves the removal of part or all of the vulva, depending on the extent of the cancer. There are different types of vulvectomies:
- Partial Vulvectomy: Only a portion of the vulva is removed.
- Radical Vulvectomy: The entire vulva, including the inner and outer labia, and possibly the clitoris, is removed.
- Lymph Node Dissection: This involves the removal of nearby lymph nodes to check for the spread of cancer. If cancer is found in the lymph nodes, additional treatment may be necessary.
Side Effects of Surgery:
- Nausea and Vomiting: These can occur due to anesthesia or the body’s response to surgery.
- Infection or Fever: Surgical wounds can become infected, leading to fever and other symptoms.
- Wound Problems: Issues such as poor healing or wound separation can occur.
- Lymphedema: Swelling, usually in the legs, can result from the removal of lymph nodes, disrupting normal lymphatic drainage.
- Pain: Post-surgical pain is common and can be managed with medications.
- Changes in Appearance: Surgery can alter the appearance of the vulva, which may affect body image and sexual function.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells. It can be used before surgery to shrink the tumor or after surgery to destroy any remaining cancer cells. Radiation therapy can also be used as the primary treatment if surgery is not an option.
Side Effects of Radiation Therapy:
- Skin Irritation: The skin around the vulva and groin may become dry, irritated, and sensitive.
- Fatigue: Tiredness is a common side effect and can become severe as treatment progresses.
- Bladder and Bowel Changes: Radiation can cause frequent urination, a burning sensation when urinating, abdominal cramps, and diarrhea.
- Vaginal Changes: The vagina may become dry, narrow, and less stretchy, which can make sexual intercourse and internal examinations uncomfortable.
- Lymphedema: Radiation to the lymph nodes can lead to swelling in the legs.
- Menopause: In younger women, radiation can cause early menopause, leading to symptoms like hot flashes and infertility.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It can be administered orally, intravenously, or topically (applied directly to the vulva). Chemotherapy is often used for advanced vulvar cancer or in combination with radiation therapy (chemoradiation) to enhance the effectiveness of treatment.
Side Effects of Chemotherapy:
- Nausea and Vomiting: Common side effects that can be managed with medications.
- Loss of Appetite: Patients may experience changes in taste and a reduced desire to eat.
- Mouth Sores: Painful sores can develop in the mouth, making eating and drinking difficult.
- Increased Risk of Infection: Chemotherapy can lower white blood cell counts, increasing the risk of infections.
- Bleeding or Bruising Easily: Low platelet counts can lead to easy bruising and bleeding.
- Hair Loss: Temporary hair loss is a common side effect.
- Fatigue: Severe tiredness can occur, affecting daily activities.
Targeted Therapy
Targeted therapy involves drugs that specifically target cancer cells without affecting normal cells. This type of therapy is still being studied for vulvar cancer and may be available through clinical trials. Targeted therapies work by interfering with specific molecules involved in cancer cell growth and survival.
Side Effects of Targeted Therapy:
- Skin Reactions: Rashes and other skin issues can occur.
- Diarrhea: Gastrointestinal disturbances are common.
- Liver Problems: Elevated liver enzymes may indicate liver irritation or damage.
- High Blood Pressure: Some targeted therapies can cause hypertension.
Immunotherapy
Immunotherapy is a newer treatment option that helps the body’s immune system recognize and attack cancer cells. It is still being studied for vulvar cancer and may be available through clinical trials.
Side Effects of Immunotherapy:
- Fatigue: Common and can be severe.
- Skin Reactions: Rashes and itching are common.
- Flu-like Symptoms: Fever, chills, and muscle aches can occur.
- Autoimmune Reactions: The immune system may attack normal tissues, leading to inflammation in organs such as the lungs, liver, and intestines.
Clinical Trials
Patients with vulvar cancer may consider participating in clinical trials to access new and innovative treatments. Clinical trials are research studies that test new treatments or new combinations of treatments to determine their safety and effectiveness.
Benefits of Clinical Trials:
- Access to New Treatments: Patients can receive cutting-edge therapies that are not yet widely available.
- Close Monitoring: Participants are closely monitored by a team of healthcare professionals.
- Contribution to Research: Participation helps advance medical knowledge and improve future cancer treatments.
Considerations for Clinical Trials:
- Eligibility: Not all patients are eligible for every trial. Eligibility criteria vary based on the study.
- Risks and Benefits: Patients should discuss the potential risks and benefits with their healthcare team.
- Informed Consent: Patients must provide informed consent before participating, ensuring they understand the study and its potential impacts.
More information about ongoing clinical trials can be found on clinicaltrial.gov
Patient Survivorship
Physical Challenges
Survivors of vulvar cancer may face physical challenges, such as changes in the appearance and function of the vulva, pain, and sexual dysfunction. Physical therapy and counseling can help address these issues.
Emotional and Psychological Challenges
The diagnosis and treatment of vulvar cancer can be emotionally and psychologically challenging. Survivors may experience anxiety, depression, and body image issues. Support groups and mental health professionals can provide valuable support.
Follow-Up Care
Regular follow-up care is essential for monitoring for any signs of recurrence and managing any long-term side effects of treatment. This may include physical exams, imaging tests, and consultations with specialists.
Lifestyle Changes
Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption, can improve overall health and reduce the risk of cancer recurrence.
This informative video is taken from WFAA
Conclusion
Vulvar cancer is a rare but serious condition that requires prompt diagnosis and treatment. Understanding the causes, risk factors, symptoms, and treatment options can help patients make informed decisions about their care. Survivors of vulvar cancer may face ongoing challenges, but with the right support and follow-up care, they can lead healthy and fulfilling lives.
Resources
- American Cancer Society – cancer.org
- Vulvar Cancer Causes & Risk Factors | moffitt.org
- National Cancer Institute – cancer.gov
- US Centers for disease control and prevention – CDC.gov
- Treatment options for vulval cancer | CancerResearchuk.org
- Modern Treatment of Vulvar Cancer – PubMed
- Vulva Cancer – StatPearls – PubMed