
Oropharyngeal Cancer: What patients should know about
Oropharyngeal Cancer
Oropharyngeal cancer is a type of head and neck cancer that affects the tissues in the throat, including the tonsils, base of the tongue, and soft palate. It’s often associated with risk factors such as tobacco use, excessive alcohol consumption, and infection with certain strains of the human papillomavirus (HPV). Symptoms may include persistent sore throat, difficulty swallowing, ear pain, or a lump in the neck. Early detection through regular screenings can significantly improve outcomes, highlighting the importance of awareness and proactive healthcare practices.
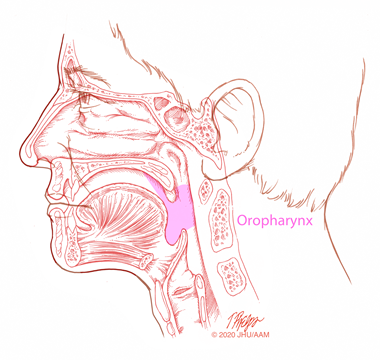
Oropharyngeal Cancer. This image is taken from hopkinsmedicine.org.
Prevalence
Oropharyngeal cancer is a relatively rare type of head and neck cancer, with an estimated 53,000 new cases diagnosed in the U.S. each year. However, its prevalence has been increasing in recent decades. According to data from the National Program of Cancer Registries and Surveillance Epidemiology and End Results program, the incidence of oropharyngeal cancer increased by 2.7% per year among men from 2001 to 2017, rising from 5.9 per 100,000 to 8.9 per 100,000. The incidence also increased among women during this period, though at a slower rate.
Only 0.4-0.6% of all oral and oropharyngeal cancers are diagnosed in patients younger than 20 years old. Most lesions found in the oral cavity of children are benign. Malignant tumors like lymphomas, sarcomas, and squamous cell carcinoma (commonly found in adults) are rarely reported in children.
In 2021, it was estimated that 434,915 people were living with oral cavity and pharynx cancer in the United States. Worldwide, an estimated 476,125 people were diagnosed with oral or oropharyngeal cancer in 2020. The rising incidence of oropharyngeal cancer, particularly among men, is largely attributed to the increasing prevalence of HPV-related disease. While smoking and alcohol use remain significant risk factors, HPV infection has become the leading cause of oropharyngeal cancer in many developed countries.
Causes and Risk Factors
The most common cause of oropharyngeal cancer is infection with HPV, particularly HPV type 16. HPV is a sexually transmitted virus that can interfere with genes that manage cell growth in the mouth and throat, leading to uncontrolled cell growth and tumor formation. HPV is found in about two-thirds of oropharyngeal cancers.
Other risk factors for oropharyngeal cancer include:
- Tobacco use (including smoking and chewing tobacco, is the single largest risk factor for oropharyngeal cancer)
- Heavy alcohol consumption
- Combination of tobacco and alcohol use
- Marijuana use
- Excess body weight
- Poor nutrition, especially a diet low in fruits and vegetables
- Older age (most common in those over 55)
- Weakened immune system
- Exposure to ultraviolet (UV) light from the sun or tanning beds (for lip cancer)
- Having a history of certain cancers, such as cervical, esophageal, or lung cancer, also increases the risk of developing oropharyngeal cancer
Prevention
The most effective ways to prevent oropharyngeal cancer are:
- Avoid tobacco use in any form. Quitting smoking can help reverse some of the damage and lower cancer risk
- Limit alcohol consumption. Heavy, long-term alcohol use increases the risk. Combining alcohol and tobacco use greatly multiplies the risk. Drink alcohol only in moderation (no more than 2 drinks per day for men, 1 for women)
- Maintain a healthy diet
- Eat plenty of fruits and vegetables. Avoid processed and red meats.
- Stay at a healthy body weight
- Protect against HPV infection. Get the HPV vaccine if eligible (recommended for preteens before exposure to HPV). Limit the number of oral sex partners. Use condoms during oral, vaginal, and anal sex (though condoms do not fully protect against HPV)
- Avoid excessive UV exposure. Use lip balm with sunscreen. Wear a wide-brimmed hat when outdoors.
- Regular dental and medical checkups are also important for early detection of precancerous changes or early-stage cancers. Dentists and doctors should examine the mouth, throat, tongue, and neck for any abnormalities during routine exams.
People with a history of heavy tobacco and alcohol use or HPV infection should be especially vigilant about seeking medical attention for any persistent symptoms, such as a sore throat, difficulty swallowing, unexplained weight loss, a neck mass, or voice changes. While these measures can significantly reduce the risk of oropharyngeal cancer, they do not guarantee prevention. Regular screening and prompt treatment of any suspicious growth are also crucial.
Learn about the surging cases of HPV-related oral throat cancer, its transmission, risks, and symptoms, in this informative video.
Types
There are several main types of oropharyngeal cancer:
- Squamous Cell Carcinoma (SCC): The most common type, accounting for over 90% of cases. Starts in the flat squamous cells lining the mouth, nose, throat and larynx. Can be further classified as HPV-positive or HPV-negative based on HPV testing.
- Verrucous Carcinoma: A rare, slow-growing type of SCC. Rarely spreads to other parts of the body but can grow deeply into surrounding tissues.
- Salivary Gland Cancers: Develop in the minor salivary glands throughout the lining of the mouth and oropharynx
Most commonly adenocarcinomas start in the parotid glands. - Other Rare Types:
-
- Basal cell carcinoma (a type of skin cancer on the lips)
- Lymphoma (starting in the lymph tissue of the tonsils and base of the tongue)
- Melanoma (from pigment cells)
- Sarcoma (from connective tissues like bone and muscle)
The type of oropharyngeal cancer is determined by the specific cell of origin and helps guide treatment. Tonsil cancer is the most common subsite.
Symptoms
The most common symptoms of oropharyngeal cancer include:
- A sore throat (pharyngitis) that doesn’t go away
- Pain or difficulty with swallowing (dysphagia)
- A lump or mass in the neck, mouth, or throat
- Hoarseness or change in voice
- Ear pain
- Numbness of the tongue or mouth
- Unexplained weight loss
Other potential symptoms are:
- Red or white patch on the gums, tongue, tonsil, or lining of the mouth
- Pain in the mouth that doesn’t go away
- Trouble chewing or moving the jaws or tongue
- Loosening of teeth or toothache
- Dentures that no longer fit
- Chronic bad breath
- Changes in speech
- Fatigue
- Loss of appetite (in later stages)
It’s important to note that many of these symptoms can also be caused by other conditions and do not necessarily mean cancer is present. However, any persistent symptoms lasting more than 2 weeks should be evaluated by a doctor.
Diagnosis
Oropharyngeal cancer is diagnosed through a combination of physical examination, imaging tests, and biopsy. The key steps in diagnosis include:
Physical Examination: The doctor takes a complete medical history and asks about symptoms and risk factors. They examine the mouth, throat, tongue, and neck for any abnormalities or lumps. The lymph nodes in the neck are also felt for enlargement.
Endoscopy: An endoscope (a thin, flexible tube with a light and camera is inserted through the nose or mouth to examine the throat and take tissue samples. This allows the doctor to see inside the mouth and throat in detail.
Biopsy: A small tissue sample is removed from any suspicious areas for examination under a microscope. This is the only way to definitively diagnose cancer. Fine needle aspiration or oral brush biopsy may be used to collect cells.
Imaging Tests: CT, MRI, or PET scans may be done to determine the size and location of the tumor and if it has spread X-rays can also be used to look for abnormalities in the mouth or neck.
HPV Testing: HPV testing may be done on the biopsy sample to determine if the cancer is HPV-related. This helps guide treatment and determine the prognosis.
If cancer is diagnosed, further tests will be done to determine the stage, which helps guide treatment decisions. Getting a second opinion from another doctor is also an option for many patients.
Treatment
There are several main treatment options for oropharyngeal cancer:
Surgery
- Surgery is often used to remove small, early-stage oropharyngeal cancers.
- Transoral surgery through the mouth may be possible for some small cancers.
- Surgeons often use laser or robotic techniques to remove cancers in the back of the throat.
- If the cancer is larger or in a difficult position, it may require an incision in the neck to remove it.
- Reconstructive surgery using tissue, skin or bone from elsewhere in the body may be needed to rebuild the areas removed.
Radiation Therapy
- Radiotherapy uses high-energy rays to destroy cancer cells.
- It can be given alone for early-stage cancers or with chemotherapy for more advanced diseases.
- Radiotherapy may also be used after surgery to reduce the risk of the cancer returning.
- Side effects include sore throat, difficulty swallowing, and changes to taste and saliva.
Chemotherapy
- Chemotherapy uses anti-cancer drugs to kill rapidly dividing cells.
- It is often given with radiation therapy (chemoradiation) for locally advanced oropharyngeal cancer.
- Chemotherapy alone may be used if the cancer has spread to other parts of the body.
- Common chemotherapy drugs include cisplatin, fluorouracil, carboplatin, docetaxel and paclitaxel.
Targeted Therapy
- Targeted therapies like cetuximab block proteins that cancer cells need to grow and divide.
- Side effects may include skin rash, fatigue, fever, and infusion reactions
Immunotherapy
- Immunotherapies like pembrolizumab and nivolumab help the immune system attack cancer cells.
- They may be used if other treatments have not been effective or the cancer has spread.
- Side effects are usually mild and may include fatigue, rash, and joint pain
Treatment is tailored to each patient based on factors like the stage of cancer, HPV status, age, and overall health. Surgery, radiation, and chemotherapy are often combined for the best outcomes.
Oropharyngeal cancer can recur (come back) after initial treatment, with roughly 10-20% of patients developing recurrent disease within 5 years. Recurrences can occur in the oropharynx, lymph nodes, or other parts of the body like the lungs, bone, or liver. Recurrence rates are about half in HPV-positive oropharyngeal cancer compared to HPV-negative disease. Patients with solitary recurrences (single site) have more favorable long-term outcomes compared to those with multi-site recurrences. Treatment options for recurrent disease depend on location, prior treatments, and overall health, and may include surgery, radiation, chemotherapy, targeted therapies, and immunotherapies.
Prognosis
The prognosis for oropharyngeal cancer depends on several factors, including the stage at diagnosis, HPV status, and overall health.
Prognostic Factors
- HPV status is a key prognostic factor
- HPV-positive oropharyngeal cancers have a better prognosis than HPV-negative cancers
- Smoking history is also important. Patients with a smoking history of 10 or more pack years have worse outcomes.
- Tumor stage and nodal status at diagnosis also impact prognosis. More advanced stage and nodal involvement are associated with poorer survival.
Patient’s Survivorship
Patients with oropharyngeal cancer face several challenges during and after treatment. Here are some of the key challenges and ways to manage them:
- Treatment Side Effects: Radiation therapy can cause a sore throat, difficulty swallowing, dry mouth, changes in taste, and fatigue. Chemotherapy can cause nausea, vomiting, fatigue, and an increased risk of infection. Surgery may lead to difficulty swallowing, changes in speech, and the need for a feeding tube. Supportive care is crucial to help manage side effects, including pain medication, anti-nausea drugs, nutritional support, and speech therapy. Maintaining good oral hygiene and staying hydrated can also help.
- Difficulty Swallowing (Dysphagia): Radiation, chemotherapy, and surgery can all cause swallowing problems that may persist long after treatment ends. Speech and language therapists can provide swallowing therapy and recommend dietary modifications. In some cases, a feeding tube may be needed temporarily or permanently.
- Changes in Speech and Voice: Tumors in the throat and treatment effects can alter speech and voice quality. Speech therapy is important to help patients regain communication abilities. Voice amplifiers or speaking valves may be helpful in some cases.
- Dry Mouth (Xerostomia): Radiation to the salivary glands often causes chronic dry mouth. Sipping water frequently, using saliva substitutes, and practising good oral hygiene can help. Medications to stimulate saliva production may also be prescribed.
- Dental Problems: Radiation can increase the risk of cavities, gum disease, and tooth loss. Seeing a dentist who specializes in treating head and neck cancer patients is important before, during, and after treatment. Fluoride treatments, dental work, and regular cleanings are crucial.
- Lymphedema: Radiation and surgery can cause swelling in the neck and face due to lymph fluid buildup. Massage, compression garments, and physical therapy can help manage lymphedema.
- Psychosocial Challenges: The physical and emotional impact of oropharyngeal cancer can be significant. Patients may experience depression, anxiety, body image issues, and difficulty with relationships and intimacy. Counseling, support groups, and connecting with other survivors can help patients cope. Involving family members in care and support is also important.
Regular follow-up care with the multidisciplinary cancer team is essential to monitor for and manage any long-term or late effects of treatment. With proper supportive care, many patients can overcome the challenges of oropharyngeal cancer and its treatment.
Palliative care
Palliative care is an important aspect of managing oropharyngeal cancer, especially for patients with advanced, metastatic, or recurrent disease. The goals of palliative care are to relieve symptoms, improve quality of life, and provide support for patients and their families. Key components of palliative care for oropharyngeal cancer include:
- Pain Management – Opioid analgesics may be needed to control pain from the tumor or treatment side effects. Radiation therapy can help relieve pain from metastatic lesions.
- Nutritional Support – Many patients require feeding tubes to maintain adequate nutrition and hydration. Speech therapists can help with swallowing therapy and dietary modifications.
- Symptom Relief – Medications and supportive care can help manage symptoms like nausea, fatigue, and dry mouth. Oxygen therapy may be needed for breathing difficulties.
- Psychosocial Support – Counseling, support groups, and palliative care specialists can help patients and families cope with the emotional and practical challenges of advanced cancer. Advance care planning discussions about goals of care are important.
- End-of-Life Care – Hospice provides comprehensive support for patients nearing the end of life. Comfort measures and pain relief are the focus in the final stages.
Palliative care should be integrated early in the disease course, alongside disease-directed treatments. An interdisciplinary team approach involving oncologists, palliative care specialists, nurses, social workers, and chaplains provides the best support for patients with advanced oropharyngeal cancer.
Recommendations for Patients
- Seek Treatment at a Specialized Cancer Center
- Understand Treatment Options: The specific treatment plan depends on factors like cancer stage, HPV status, location of the tumor, and overall health. You should discuss the risks and benefits of each option with your oncology team.
- Quit Smoking and Limit Alcohol: Patients who smoke or drink alcohol heavily should quit or cut back, as these habits can worsen outcomes and increase the risk of recurrence. Support is available to help with smoking cessation and alcohol reduction.
- Attend All Follow-Up Appointments: Regular follow-up visits are crucial to monitor for recurrence or new cancers. Checkups are typically every 6-12 weeks for the first year, then less frequently. You should report any new symptoms promptly.
- Manage Side Effects: Treatment side effects like difficulty swallowing, dry mouth, and changes in taste are common but can be managed with supportive care. You should work closely with their healthcare team to address any side effects.
David discusses his experience coping with oropharyngeal cancer.
Conclusion
In conclusion, while oropharyngeal cancer presents significant challenges, advancements in treatment options, supportive care, and ongoing research offer hope for improved outcomes. By seeking care at specialized centers, understanding treatment choices, and actively managing side effects, patients can navigate their journey with confidence. With the support of dedicated healthcare teams and a proactive approach to follow-up care, individuals facing oropharyngeal cancer can embrace optimism and strive for successful treatment and recovery.
An inspiring video follows Joe’s journey from routine sore throat check-up to battling cancer, enduring treatment side effects, and ultimately triumphing, now sharing his recovery insights.
Resources
- Memorial Sloan Kettering Cancer Center – mskcc.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research UK – cancerresearchuk.org
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- Surgical clinical trials for HPV-positive oropharyngeal carcinoma – PubMed
- Oropharyngeal Squamous Cell Carcinoma – PubMed
- City of Hope – cancercenter.com
- Canadian Cancer Society – cancer.ca
- Clinicaltrials.gov
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
