
Bile Duct Cancer: Symptoms ,Causes, Stages, Diagnosis and Treatment
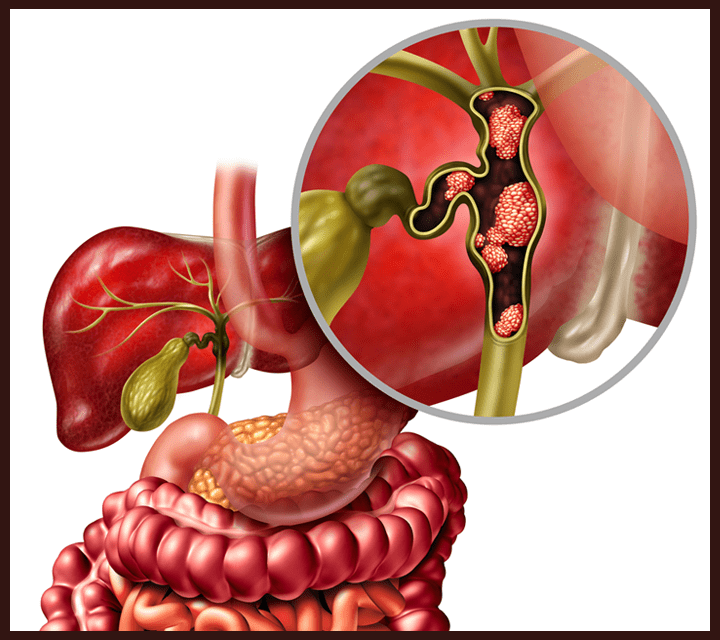
Bile duct cancer, also known as cholangiocarcinoma, is a rare but aggressive malignancy that originates in the bile ducts, which are responsible for transporting bile from the liver to the small intestine. This type of cancer can develop in different parts of the bile duct system, including intrahepatic (inside the liver), perihilar(at the liver hilum), and distal (closer to the small intestine).
Understanding the symptoms, causes, stages, diagnosis, and treatment options of cholangiocarcinoma is crucial for improving early detection and patient outcomes. This article will provide a comprehensive overview of these aspects, offering insights into current medical advancements and potential treatment approaches.
What Are the Symptoms of Bile Duct Cancer?
Jaundice is one of the earliest and most noticeable symptoms of bile duct cancer. It occurs when a tumor blocks bile flow, leading to a buildup of bilirubin in the blood, which causes yellowing of the skin and eyes. This symptom is often associated with advanced stages of the disease (Mayo Clinic). Itchy Skin (Pruritus) is caused by the accumulation of bile salts under the skin. It may develop before jaundice and can be intense, significantly affecting quality of life (American Cancer Society).
Abdominal Pain typically appears in the upper right side of the abdomen as the tumor grows and presses against surrounding structures. The pain can range from mild discomfort in early stages to severe pain in later stages (Mayo Clinic).Unintended Weight Loss is common in many cancer types, including bile duct cancer. Patients may experience a loss of appetite and significant weight reduction due to increased energy demands and cancer-related metabolic changes. Studies indicate that 40–50% of patients with gastrointestinal cancers experience unexplained weight loss (National Cancer Institute).

What are the Causes and Risk Factors for Bile Duct Cancer?
Bile duct cancer, or cholangiocarcinoma, arises from a combination of genetic, environmental, and lifestyle factors. A significant risk factor is primary sclerosing cholangitis (PSC), a condition characterized by chronic inflammation and scarring of the bile ducts. According to the American Cancer Society, individuals with PSC have an increased risk of developing bile duct cancer.Chronic liver diseases, such as hepatitis B and C infections, also elevate the risk. A study published in The Lancet Public Health in 2024 by Hyuna Sung and colleagues from the American Cancer Society highlighted that individuals born in the 1980s and 1990s have a higher risk of developing liver cancer compared to those born in the 1950s, suggesting a generational increase in risk factors.
Environmental exposures play a crucial role as well. In regions like Southeast Asia, infection with liver flukes, such as Opisthorchis viverrini and Clonorchis sinensis, is a known risk factor for cholangiocarcinoma. Additionally, exposure to certain chemicals, including Thorotrast (a radiographic contrast agent used in the past), has been linked to an increased risk of bile duct cancer.Lifestyle factors, particularly obesity and diabetes, have been associated with a higher incidence of bile duct cancer. The same study by Sung et al. reported that sedentary behavior and dietary changes contribute to rising cancer rates among younger populations.
Understanding these risk factors is essential for early detection and prevention strategies, especially given the increasing incidence of bile duct cancer in younger generations.
What Are the Types of Bile Duct Cancer?
Bile duct cancer, or cholangiocarcinoma, is classified based on its location within the bile duct system. The three main types are Intrahepatic Cholangiocarcinoma, Perihilar (Hilar) Cholangiocarcinoma and Distal Cholangiocarcinoma.
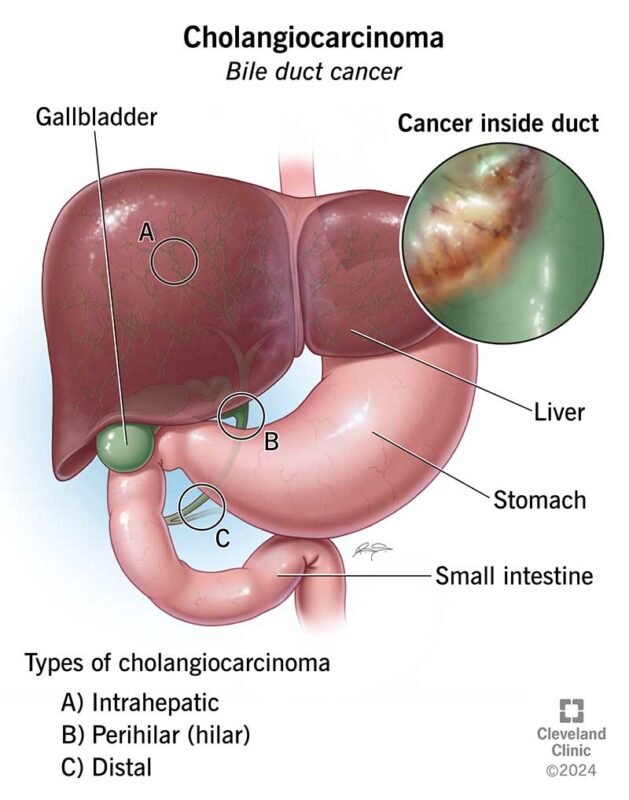
Intrahepatic Cholangiocarcinoma
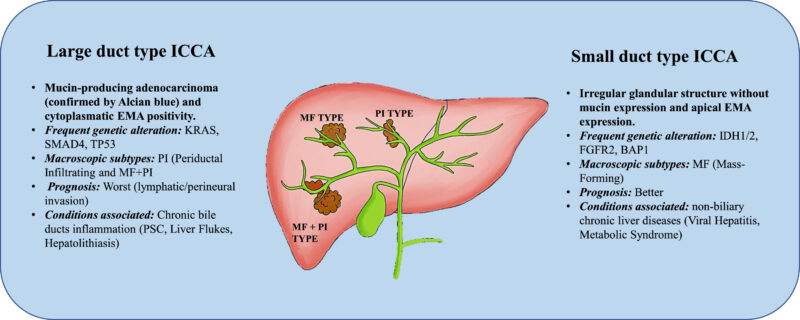
Intrahepatic cholangiocarcinoma (ICC) is a form of bile duct cancer that originates within the liver’s bile ducts. These ducts are responsible for transporting bile—a digestive fluid produced by the liver—to the gallbladder and small intestine. Unlike other types of cholangiocarcinoma that occur outside the liver, ICC arises from the intricate network of ducts located within the liver itself.
In a study published in 2025, Obaid Ur Rehman and colleagues analyzed intrahepatic cholangiocarcinoma (ICC) mortality trends in the United States from 1999 to 2020. They found that the age-adjusted mortality rate (AAMR) increased from 5.6 per 100,000 individuals in 1999 to 14.3 in 2020, reflecting an annual percentage change (APC) of 3.59% (95% CI: 3.34 to 3.83, p < 0.05). The study also noted higher AAMRs in males (1.7, 95% CI: 1.6 to 1.7) compared to females (1.3, 95% CI: 1.3 to 1.3). Geographically, the Northeast region exhibited the highest mortality rates, with urban areas showing an AAMR of 1.4 (95% CI: 1.3 to 1.5). Among racial groups, non-Hispanic Asian or Pacific Islanders had the highest AAMR at 1.9 (95% CI: 1.9 to 2)
One of the defining characteristics of ICC is its tendency to remain asymptomatic in its early stages, often leading to late diagnoses when the disease has advanced.
Pathologically, ICC is an epithelial neoplasm with biliary differentiation, typically presenting with abundant fibrous tumor stroma. This fibrous tissue contains cancer-associated fibroblasts, as well as innate and adaptive immune cells. Recent classifications have identified two subtypes of ICC: small duct type and large duct type, each with distinct histological features.
Extrahepatic Cholangiocarcinoma
Extrahepatic cholangiocarcinoma is a form of bile duct cancer that arises in the bile ducts located outside the liver. These ducts play a crucial role in transporting bile from the liver and gallbladder to the small intestine, facilitating digestion. When malignant cells develop in these external ducts, they can obstruct bile flow, leading to noticeable symptoms.
Due to the tumor’s location, symptoms often prompt earlier medical evaluation compared to intrahepatic forms. Despite earlier symptom presentation, the prognosis for extrahepatic cholangiocarcinoma remains challenging. According to the American Cancer Society, the five-year relative survival rate for localized extrahepatic bile duct cancers is approximately 18%. This rate decreases significantly if the cancer has spread to regional tissues or lymph nodes.
Early detection and prompt treatment are vital for improving outcomes in individuals with extrahepatic cholangiocarcinoma. However, the disease’s aggressive nature and tendency for late diagnosis often complicate effective management.
Perihilar Cholangiocarcinoma
Perihilar cholangiocarcinoma (pCCA), also known as a Klatskin tumor, is a type of bile duct cancer that arises at the confluence of the right and left hepatic ducts, where the bile ducts exit the liver. This anatomical positioning makes pCCA particularly challenging to diagnose and treat. According to a review by first author Andrea Donisi in the World Journal of Gastrointestinal Oncology, pCCA is the most common form of cholangiocarcinoma and is burdened by a complicated diagnostic process due to its anatomical location, which makes surgical approaches challenging.
The tumor’s proximity to major vascular structures and its tendency to cause biliary obstruction often lead to symptoms such as jaundice, itching, and abdominal pain. The complex location of pCCA complicates surgical interventions, often resulting in poor outcomes. Donisi et al. emphasize that a multimodal diagnostic approach should be carried out by specialized centers to avoid misdiagnosis.
Histologically, pCCA typically presents as an adenocarcinoma with abundant fibrous stroma. The tumor’s desmoplastic nature can make it difficult to distinguish from surrounding tissues during imaging and surgical procedures.Early detection of pCCA is crucial but challenging due to its deep location and non-specific initial symptoms.
How Is Bile Duct Cancer Diagnosed?
Early and accurate diagnosis of bile duct cancer is crucial for effective treatment. Various diagnostic methods are employed, each with specific advantages.
- Blood Tests: Elevated levels of enzymes such as alkaline phosphatase and gamma-glutamyl transferase can indicate bile duct obstruction. However, these markers are not specific to bile duct cancer and can be elevated in other conditions.
- Imaging Studies: Ultrasound is typically the first imaging modality used to detect biliary dilatation. For more detailed assessment, Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) are utilized to evaluate the extent of the disease and its relationship to surrounding structures. Magnetic Resonance Cholangiopancreatography (MRCP), a specific type of MRI, provides detailed images of the bile ducts and is non-invasive, making it a valuable tool in diagnosis.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): ERCP combines endoscopy and fluoroscopy to visualize the bile ducts. It allows for direct imaging, biopsy, and therapeutic interventions such as stent placement to relieve obstructions. While ERCP is invasive and carries risks, it is particularly useful when tissue sampling is necessary.
- Biopsy: Obtaining a tissue sample is essential for definitive diagnosis. Biopsies can be performed during ERCP or through percutaneous approaches guided by imaging. Histological examination of the tissue confirms the presence of malignancy and provides information on tumor type and grade.
Early detection significantly improves prognosis, as bile duct cancer often presents with non-specific symptoms and is diagnosed at advanced stages. Detecting the disease early increases the likelihood of successful surgical resection, which is currently the only potential cure.
Genetic Testing for Bile Duct Cancer
Genetic testing is pivotal in identifying individuals at elevated risk for cholangiocarcinoma, particularly those with specific genetic mutations. In a study published in JAMA Oncology, first author Ghassan K. Abou-Alfa reported that mutations in the isocitrate dehydrogenase 1 (IDH1) gene are detected in approximately 13% of intrahepatic cholangiocarcinomas.
Detecting such mutations is crucial, as they can inform treatment strategies. For example, the presence of an IDH1 mutation may make a patient eligible for targeted therapies like ivosidenib, which has been shown to improve progression-free survival in patients with IDH1-mutated cholangiocarcinoma.
Given the implications for treatment, it is recommended that patients diagnosed with cholangiocarcinoma undergo comprehensive genomic profiling to identify actionable mutations. This approach enables personalized treatment plans, potentially improving outcomes.
What Are the Treatment Options for Bile Duct Cancer?
The management of cholangiocarcinoma is determined by tumor location, stage, and molecular characteristics. Current treatment strategies include:
- Surgical Resection – The only potentially curative approach, applicable in localized disease.
- Systemic Chemotherapy – Standard first-line treatment for unresectable or metastatic cases.
- Radiation Therapy – Used as an adjunct for local control in select patients.
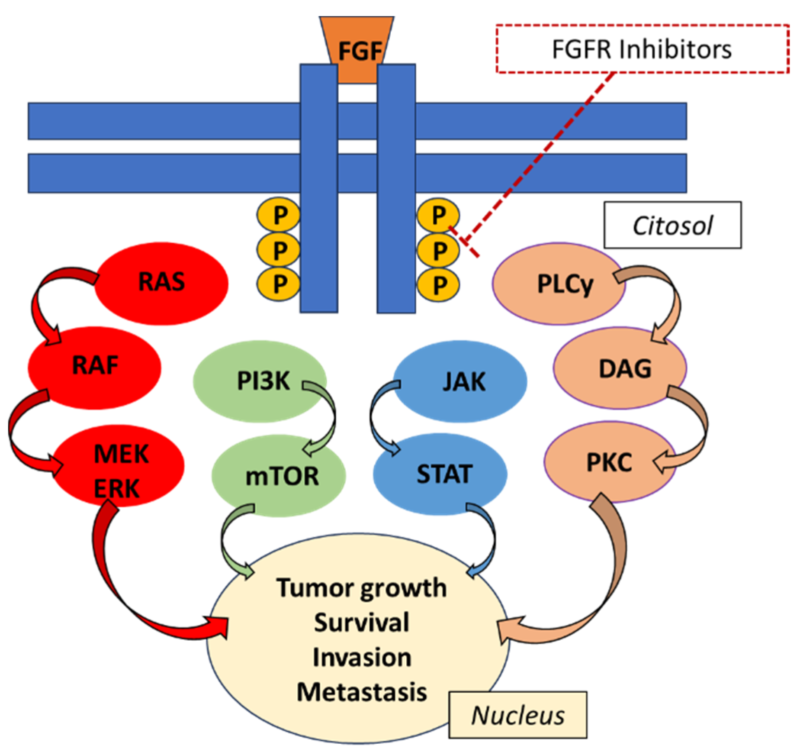
- Targeted Therapy – Precision treatments based on molecular profiling, including IDH1 and FGFR inhibitors.
Each modality is selected based on tumor biology and patient condition, often requiring a multidisciplinary approach for optimal outcomes.
Surgery for Bile Duct Cancer
Surgical interventions are pivotal in the management of bile duct cancer, with procedures tailored to tumor location and extent. The primary surgical options include bile duct resection and liver transplantation, each presenting distinct risks and benefits.
- Bile Duct Resection: This procedure involves the excision of the affected bile duct segment, often accompanied by partial hepatectomy or pancreaticoduodenectomy, depending on tumor location. Achieving a microscopically negative margin (R0 resection) is crucial for improved survival outcomes. However, these extensive radical procedures are not always safe, because there are risks of postoperative liver failure and pancreatic leakage.
- Liver Transplantation: For select patients with early-stage, unresectable perihilar cholangiocarcinoma, liver transplantation following neoadjuvant therapy offers a potential cure. This approach has demonstrated favorable outcomes in carefully selected patients. However, the scarcity of donor organs and stringent selection criteria limit its applicability. Additionally, the risk of tumor recurrence and complications related to immunosuppression are significant considerations.
Chemotherapy for Bile Duct Cancer
Chemotherapy is a cornerstone in the management of advanced biliary tract cancers, particularly when surgical options are not feasible. The combination of gemcitabine and cisplatin has been established as a standard first-line treatment. In a pivotal study published in the New England Journal of Medicine, first author Juan W. Valle reported that this regimen resulted in a median overall survival of 11.7 months, compared to 8.1months with gemcitabine alone, indicating a 35% reduction in the risk of death.
Despite its efficacy, chemotherapy is associated with notable adverse effects. In a real-world study published in the Journal of Gastrointestinal Oncology, first author Yuki Sugiura observed that 81.3% of patients experienced grade 3 or higher severe adverse events. Specifically, 54.2% of patients developed neutropenia, 20.8% experienced anemia, and 12.5% had thrombocytopenia.
For patients whose disease progresses after first-line therapy, second-line treatments are considered. The ABC-06 trial, led by Angela Lamarca and published in The Lancet Oncology, demonstrated that the addition ofFOLFOX chemotherapy to active symptom control improved median overall survival to 6.2 months, compared to 5.3 months with symptom control alone. However, grade 3 to 5 adverse events were reported in 69% of patients receiving FOLFOX, with neutropenia (12%), fatigue (11%), and infection (10%) being the most common.
Latest Advance Treatment in Bile Duct Cancer
Recent advancements in the treatment of bile duct cancer have introduced targeted therapies and immunotherapies that offer new hope for patients.
- Pemigatinib: Approved by the U.S. Food and Drug Administration (FDA) in 2020, pemigatinib targets fibroblast growth factor receptor 2 (FGFR2) fusions or rearrangements, which occur in approximately 14% of bile duct cancers.
- Futibatinib: This next-generation FGFR inhibitor has shown promise in clinical trials, particularly for patients who developed resistance to earlier FGFR inhibitors. In a study led by Dr. Milind Javle at MD Anderson Cancer Center, futibatinib demonstrated a median progression-free survival of seven months.
- Ivosidenib: Targeting isocitrate dehydrogenase 1 (IDH1) mutations, ivosidenib received FDA approval in 2021 for patients with previously treated, locally advanced, or metastatic cholangiocarcinoma harboring this mutation.
- Durvalumab: The TOPAZ-1 trial demonstrated that adding durvalumab to standard chemotherapy modestly improved survival in patients with advanced biliary tract cancers. This combination received FDA approval in 2022.
These developments represent significant progress in the management of bile duct cancer, offering personalized treatment options that improve patient outcomes
What Are the Stages of Bile Duct Cancer?
Bile duct cancer, or cholangiocarcinoma, is staged using the TNM system, which assesses tumor size and extent (T), lymph node involvement (N), and metastasis (M). This staging informs treatment decisions and prognostic expectations.
- Stage I (Localized Disease): At this initial stage, the cancer is confined to the bile duct without lymph node involvement or distant spread. Surgical resection is the primary treatment, offering the best chance for cure. However, even with surgery, recurrence rates are significant. A study by Nathan H. Cho in the Japanese Journal of Clinical Oncology reported that disease relapse after resection occurs in up to two-thirds of patients.
- Stage II (Locally Advanced Disease): Cancer has extended beyond the bile duct into nearby tissues or organs but remains resectable. Surgical intervention is still considered, often supplemented by adjuvant therapies. The prognosis is less favorable than Stage I, with five-year survival rates varying based on tumor location and surgical success. For instance, a study in the British Journal of Surgery by first author T. Miurafound that the overall five-year survival rate after resection was 39%.
- Stage III (Regional Spread): The cancer involves regional lymph nodes or major blood vessels, complicating surgical options. Treatment may include a combination of surgery, chemotherapy, and radiation therapy. The prognosis is guarded, with five-year survival rates significantly decreasing. According to a study in Scientific Reports by first author Jae Hoon Lee, prognostic factors included age, surgery, primary tumor size, multiple tumors, vascular invasion, and negative surgical margin.
- Stage IV (Metastatic Disease): Cancer has spread to distant organs, such as the liver, lungs, or bones. Surgical options are typically not viable. Systemic chemotherapy is the mainstay of treatment, aiming to prolong survival and alleviate symptoms. The prognosis is poor, with a five-year survival rate of less than 5%in general. Overall mean duration of survival is less than 6 months in people with metastatic disease.
After Treatment: What to Expect
Recovery after bile duct cancer treatment varies based on the type of intervention, with patients often experiencing fatigue, digestive issues, and liver function complications.Fatigue is common, sometimes lasting for months, while liver function must be closely monitored to detect complications early.Digestive problems, including nausea and diarrhea, can arise, especially after surgery, requiring dietary adjustments.
Follow-up care is essential, with regular check-ups scheduled every few months to monitor recovery and detect any signs of recurrence.Doctors typically use blood tests and imaging scans to assess the liver and ensure the cancer has not returned.
While the road to recovery can be challenging, ongoing medical supervision and lifestyle adjustments play a crucial role in improving long-term outcomes.
How Is Bile Duct Cancer Prognosis Determined?
The prognosis of bile duct cancer is influenced by factors such as the stage at diagnosis, tumor location, and the patient’s overall health. Early-stage detection, where the cancer is localized, offers a more favorable outlook compared to advanced stages with regional or distant spread. For instance, the five-year relative survival rate for localized intrahepatic bile duct cancer is approximately 23%, but it decreases to 3% when the disease has metastasized.
Tumor location also plays a significant role; cancers located at the perihilar region (where the bile ducts exit the liver) are often diagnosed at a more advanced stage, leading to a poorer prognosis.
How Long Does It Take to Notice and Cure Bile Duct Cancer?
The timeline from the onset of symptoms to the diagnosis and treatment of bile duct cancer can vary significantly. Symptoms such as jaundice, abdominal pain, and weight loss often lead individuals to seek medical attention. Upon presentation, diagnostic procedures—including imaging studies and biopsies—are conducted to confirm the presence of cancer. This diagnostic phase may span several weeks, depending on the availability of medical services and the complexity of the case.
Once diagnosed, the treatment plan is tailored to the cancer’s stage and location, as well as the patient’s overall health. Surgical interventions, such as bile duct resection or liver transplantation, are considered when feasible. Post-surgery, hospitalization typically lasts 1 to 2 weeks, with full recovery extending over several weeks to months, contingent on the surgery’s extent and the patient’s health status.
How to Live with Bile Duct Cancer?
Managing life with bile duct cancer involves addressing physical health, mental well-being, and lifestyle adjustments.
- Mental Health Support: Engaging in activities that bring joy, such as reading or spending time outdoors, can alleviate stress. Complementary therapies like yoga and guided imagery may also reduce anxiety.
- Dietary Changes: Consuming small, frequent meals and opting for full-fat versions of foods can help maintain weight and energy levels. Incorporating nutritious snacks ensures adequate calorie intake.
- Exercise: Regular physical activity, such as daily 30-minute walks, can boost energy, improve digestion, and enhance mood. Exercise also aids in maintaining a healthy weight and may reduce the risk of cancer recurrence.
By focusing on these areas, individuals can improve their quality of life during and after treatment.
Can Bile Duct Cancer Be Prevented?
Maintaining liver health is crucial in reducing the risk of bile duct cancer. Adopting a healthy lifestyle, including regular physical activity and a balanced diet rich in fruits, vegetables, and whole grains, can help achieve and maintain a healthy weight, thereby potentially lowering cancer risk. Avoiding exposure to known carcinogens is another important preventive measure. For instance, refraining from tobacco use and limiting alcohol consumption can reduce the risk of liver-related cancers.
Regular medical checkups play a vital role in early detection, which is crucial for successful treatment outcomes. Being aware of risk factors and symptoms can lead to earlier diagnosis and more effective treatment. By implementing these preventive strategies, individuals can significantly reduce their risk of developing bile duct cancer and promote overall liver health.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is bile duct cancer, and why is it significant?
Bile duct cancer (cholangiocarcinoma) is a rare but aggressive malignancy that develops in the bile ducts, which transport bile from the liver to the small intestine. Due to its aggressive nature and late-stage diagnosis, early detection and treatment are crucial for improving survival rates.
What are the early symptoms of bile duct cancer?
Early symptoms include jaundice (yellowing of the skin and eyes), itchy skin, abdominal pain, unexplained weight loss, and fatigue. However, these symptoms are often subtle and can be mistaken for other liver or gastrointestinal conditions.
What are the main risk factors for developing bile duct cancer?
Major risk factors include primary sclerosing cholangitis (PSC), chronic liver diseases (such as hepatitis B and C), liver fluke infections, obesity, diabetes, and exposure to certain chemicals. Genetic mutations, such as IDH1 and FGFR2, have also been linked to this cancer.
How is bile duct cancer diagnosed?
Diagnosis involves blood tests, imaging studies (ultrasound, MRI, CT scan, and MRCP), and biopsy procedures. Endoscopic retrograde cholangiopancreatography (ERCP) is often used to obtain tissue samples and detect bile duct obstructions.
Can bile duct cancer be treated with targeted therapy?
Yes. Targeted therapy drugs, such as pemigatinib (FGFR2 inhibitor) and ivosidenib (IDH1 inhibitor), have been approved for use in patients with specific genetic mutations. These treatments offer a more personalized approach to managing advanced bile duct cancer.
Can bile duct cancer be prevented?
Although bile duct cancer cannot always be prevented, reducing risk factors such as avoiding liver fluke infections, managing liver disease, maintaining a healthy weight, quitting smoking, and limiting alcohol consumption can lower the risk. Regular screening in high-risk individuals is also recommended.
What is the latest research on bile duct cancer treatment?
Recent advances focus on immunotherapy and molecular-targeted treatments. Durvalumab (immunotherapy), combined with chemotherapy, has shown promise in improving survival rates. Researchers are also investigating CAR-T cell therapy and gene-based treatments to enhance patient outcomes.
Is bile duct cancer hereditary?
Bile duct cancer is not typically hereditary, but certain genetic conditions, such as Lynch syndrome, can increase the risk. Genetic testing may help assess predisposition.
Can bile duct cancer be misdiagnosed?
Yes, bile duct cancer can be misdiagnosed as gallstones, hepatitis, or other liver diseases due to similar symptoms. Advanced imaging and biopsy are crucial for accurate diagnosis.
What is the survival rate for bile duct cancer?
Survival rates depend on the cancer stage. Early-stage (localized) cases have a 5-year survival rate of ~23%, while advanced-stage (metastatic) cases have a much lower rate (~3%).
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
