At the MASCC 2025 Annual Meeting, Dr. Jose M. Garcia of the University of Washington and VA Puget Sound Health Care System delivered a comprehensive overview of the evolving landscape of cancer cachexia management, emphasizing hormonal and non-pharmacological interventions. His presentation focused on new strategies to mitigate muscle wasting, fatigue, and quality of life deterioration in patients with advanced cancer.
Understanding Cancer Cachexia: A Persistent Challenge
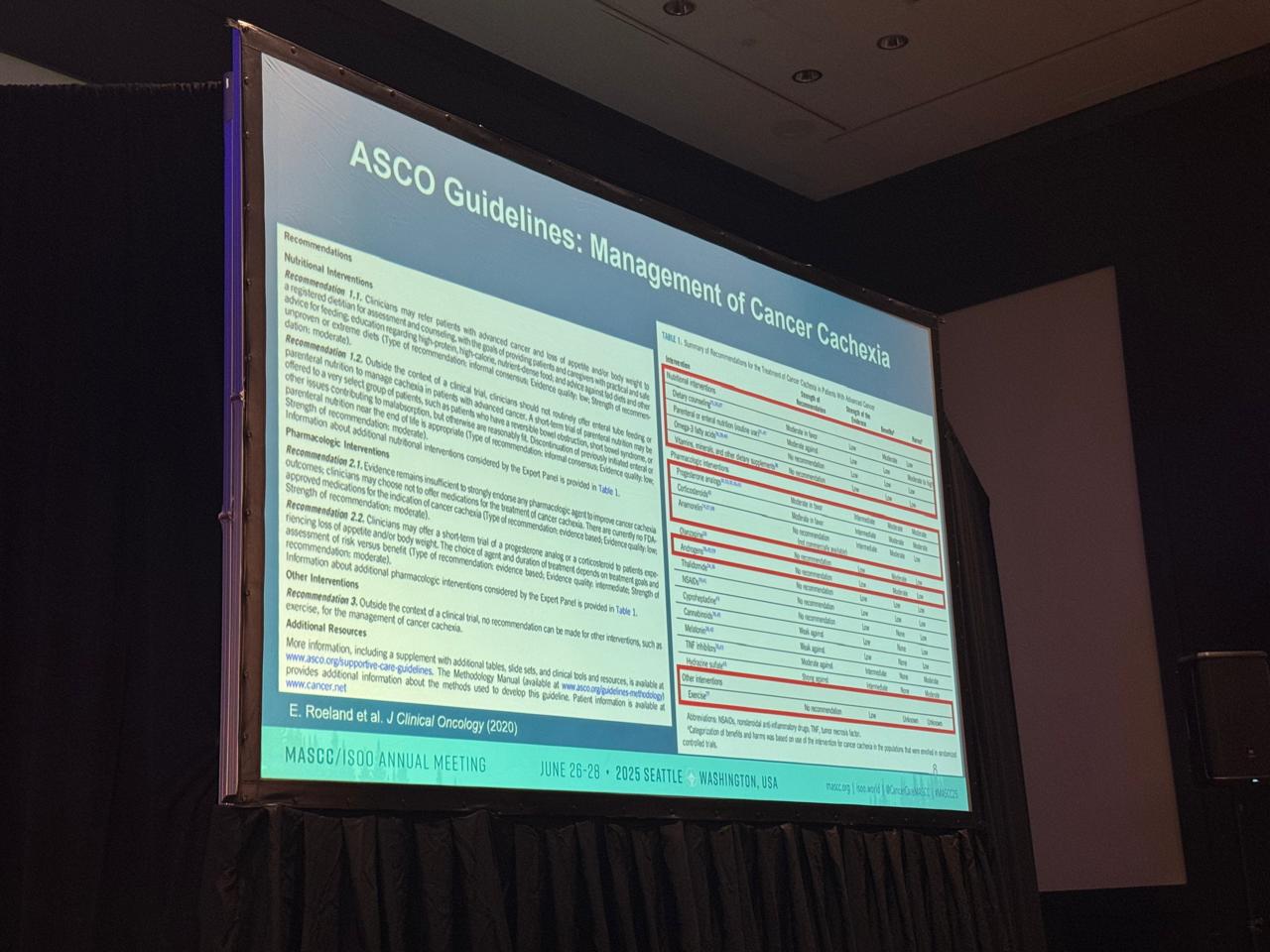
Cancer cachexia is a multifactorial syndrome characterized by involuntary loss of skeletal muscle mass—with or without fat loss—that cannot be reversed by conventional nutrition. It is associated with progressive functional impairment, poor treatment tolerance, and reduced survival. Despite its clinical significance, there are currently no approved treatments.
One of the main barriers to therapeutic progress, Dr. Garcia noted, is the lack of consensus on clinically meaningful endpoints for assessing response to treatment. Measures of physical function, appetite, fatigue, and quality of life are often inconsistently applied across studies.
Hormonal Interventions: Repurposing for Cachexia Care
Dr. Garcia highlighted the potential of hormonal agents, particularly ghrelin receptor agonists and testosterone replacement, as emerging candidates in supportive care.
Macimorelin, an oral ghrelin receptor agonist approved for adult growth hormone deficiency diagnosis, was recently tested in a pilot study for cancer-related cachexia. In the study:
- Patients with unintentional weight loss were randomized to receive macimorelin or placebo for one week.
- The drug was well tolerated, with no significant adverse events.
- Some participants experienced numerical improvements in body weight, quality of life (QOL), and functional outcomes.
- The study showed that growth hormone levels increased post-dose with macimorelin but not with placebo. Though the results were preliminary, they suggest potential for longer-term evaluation of this agent.
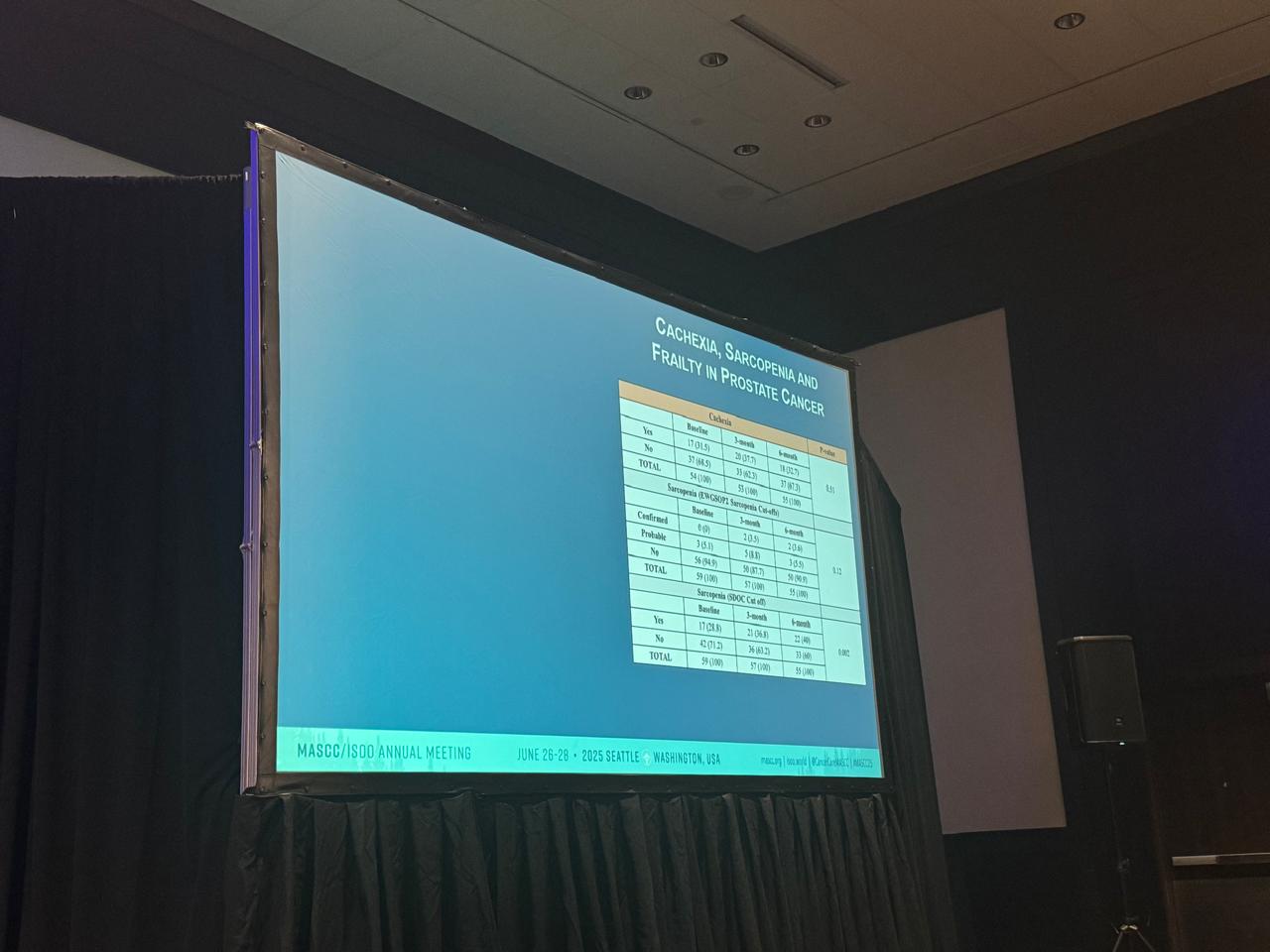
Separately, testosterone replacement therapy (TRT) was discussed as a promising strategy in hypogonadal men with cancer, a population frequently overlooked in supportive care trials. In studies such as TEMEC and TCS, TRT was associated with trends toward improved fatigue, sexual function, social well-being, and body composition—though larger trials are needed for confirmation.
Non-Pharmacological Approaches: From Exercise to Electrical Stimulation
Beyond drug therapy, Dr. Garcia emphasized non-pharmacological strategies, especially structured exercise programs and neuromuscular electrical stimulation (NMES).
Although exercise is known to improve physical function, its clinical uptake remains limited. Dr. Garcia’s team found that only 10–26% of eligible patients are referred to therapy, often due to fatigue, treatment-related precautions, or lack of guidelines.
NMES was explored as a practical alternative that can activate muscle contractions in weak or fatigued patients. In a recent study, NMES:
- Helped preserve hand grip strength
- Improved appendicular muscle mass
- Was well tolerated and feasible in outpatient settings
These interventions may become essential tools in mitigating functional decline in cachexia and sarcopenia.
Barriers and Research Gaps
Despite progress, several systemic challenges remain:
- Incomplete understanding of cachexia’s mechanisms in humans
- Lack of validated tools to assess physical function and treatment response
- Limited biomarkers to identify patients most likely to benefit
- Regulatory and funding gaps that delay intervention development
Dr. Garcia called for multidisciplinary approaches and the development of a clinical trials network focused on cachexia phenotyping, endpoint validation, and implementation science.
Conclusion: A Roadmap for the Future
The session concluded with a clear message: addressing cachexia in advanced cancer will require a coordinated effort spanning hormonal therapies, exercise, device-based interventions, and robust clinical endpoints.
“We need to move beyond body weight,” Dr. Garcia said, emphasizing the importance of patient-reported outcomes like fatigue, mobility, and quality of life.
With deeper mechanistic understanding and collaborative trial design, the field is finally positioned to make meaningful strides against a condition that has too long been left untreated.