A biopsy is a common and essential medical procedure used to better understand what’s happening inside the body. When something unusual is found—like a lump, a suspicious area on a scan, or ongoing unexplained symptoms—doctors may recommend a biopsy to investigate further. The procedure involves removing a small sample of tissue or cells from the affected area so it can be carefully examined under a microscope by a specialist called a pathologist.
This article will guide you through everything you need to know about biopsies: why doctors recommend them, the different types that exist, what happens during the procedure, what the results can show, and what risks or side effects to be aware of.
Why Might You Need a Biopsy?
Doctors may recommend a biopsy for a number of reasons, but most often it’s because something unusual has been found during an exam or on an imaging test. For example, if you or your doctor notice a lump, an area of swelling, or an unusual mass on an X-ray, mammogram, or CT scan, a biopsy can help determine what’s going on inside that area. Sometimes, a biopsy is ordered after seeing abnormal blood test results, noticing persistent inflammation, or observing unexplained bleeding—especially if symptoms don’t go away with initial treatment.
Biopsies are especially valuable in diagnosing cancer. They can tell doctors whether a growth is benign (non-cancerous) or malignant (cancerous), and help determine the type of cancer and how aggressive it is. But cancer isn’t the only reason for a biopsy. This procedure also plays an important role in identifying infections, such as tuberculosis or fungal diseases; autoimmune conditions, like lupus or vasculitis; and chronic organ damage, particularly in the liver, kidneys, or lungs.
By examining the tissue sample closely, doctors can learn not just what kind of disease is present, but also how advanced it is and how best to treat it. In this way, a biopsy serves as both a diagnostic tool and a guide to treatment planning.
Types of Biopsies
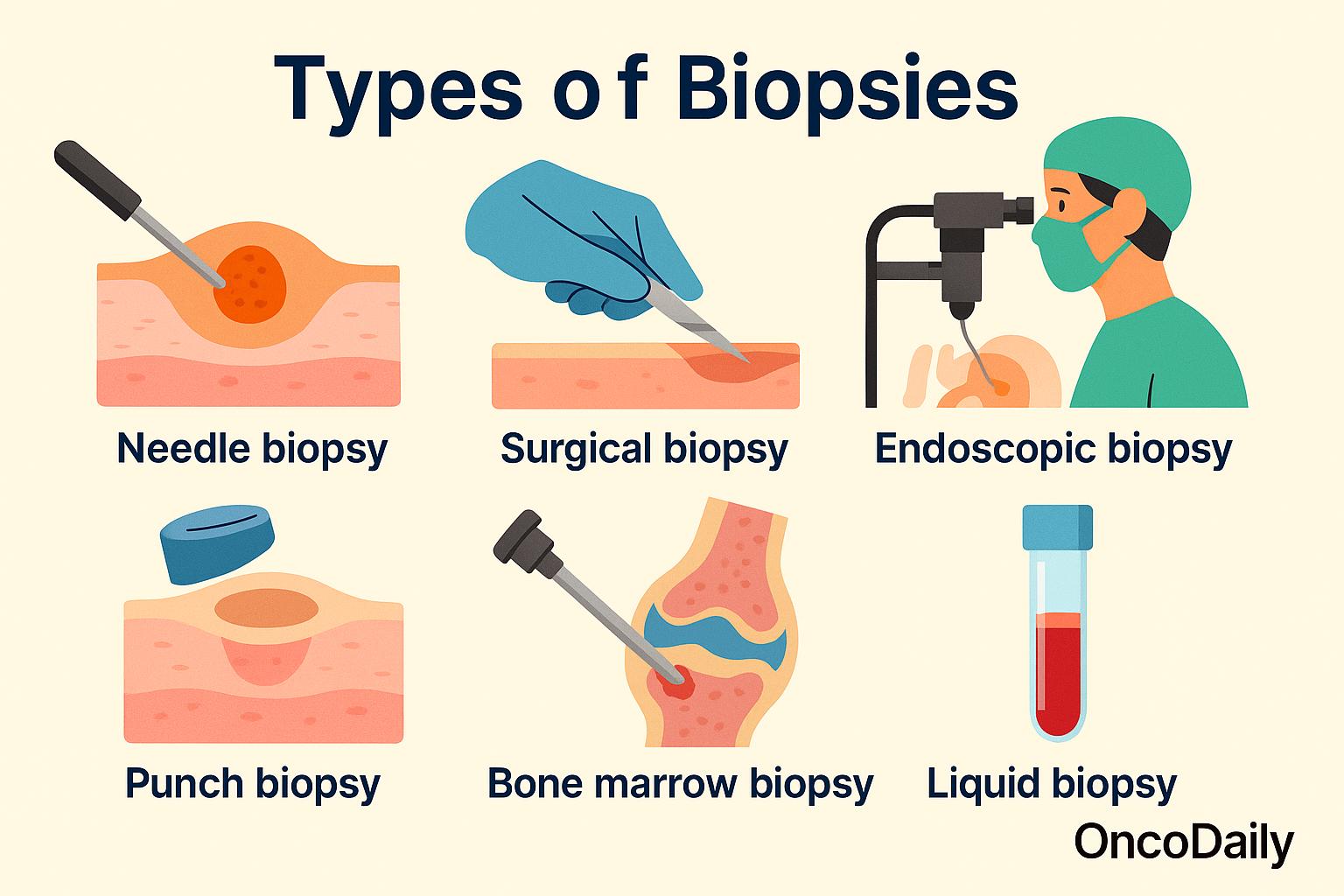
There are several different types of biopsies, and the method your doctor chooses depends largely on two things: the location of the tissue being tested and the reason for the biopsy. Some biopsies are very simple and can be done in a clinic with local anesthesia, while others require more advanced procedures in a hospital or surgical setting. Each type has its own purpose and approach.
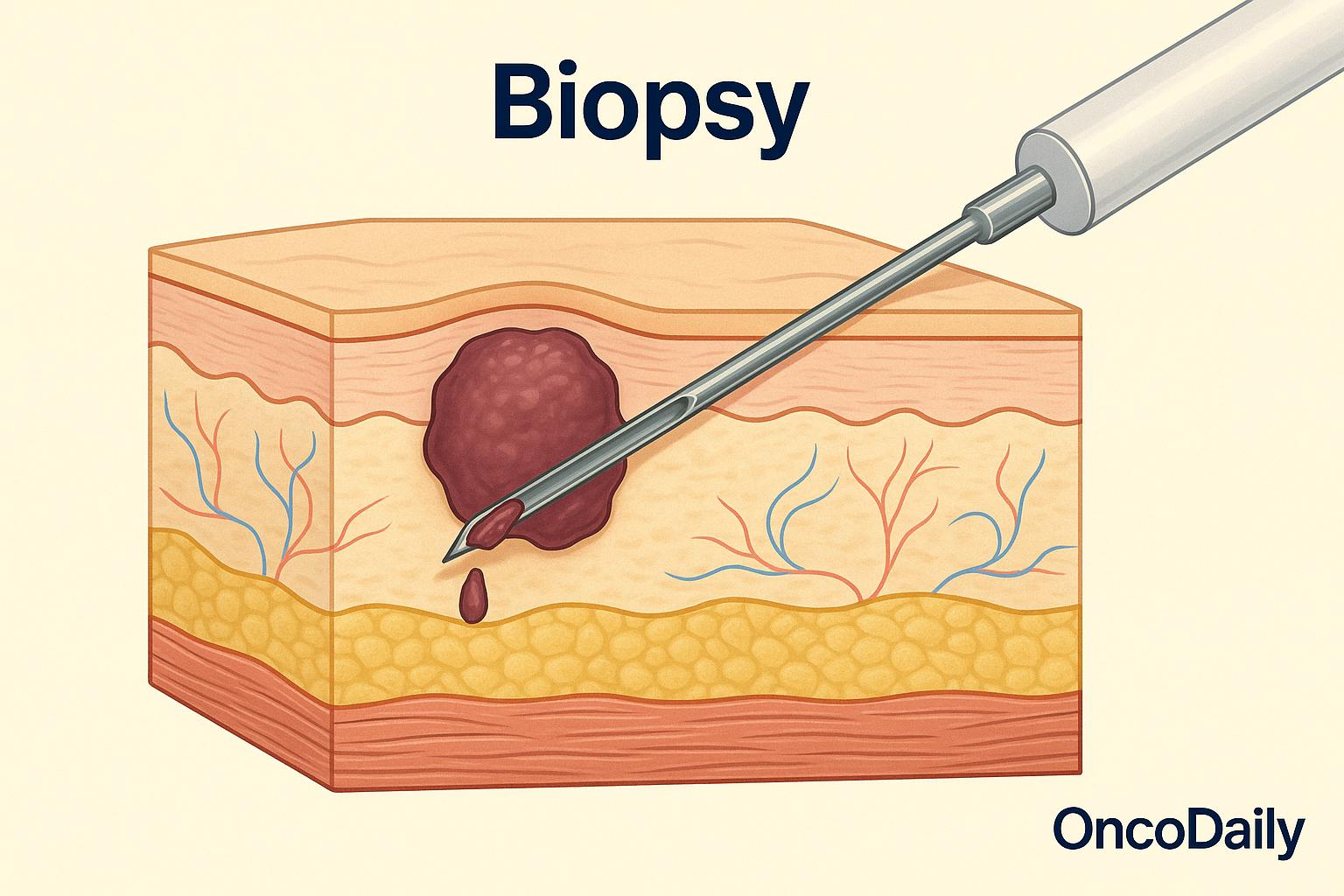
One of the most common methods is the needle biopsy. This involves using a thin, hollow needle to extract tissue or fluid from a suspicious area. There are two main types: fine-needle aspiration (FNA), which uses a very thin needle to withdraw cells, and core needle biopsy, which uses a slightly larger needle to remove a small cylinder of tissue. These procedures are often used for lumps in the breast, thyroid, or lymph nodes, and they are typically quick and minimally invasive.
If more tissue is needed, a surgical biopsy may be performed. In an incisional biopsy, only a small part of the abnormal area is removed, while in an excisional biopsy, the entire lump or suspicious tissue is taken out. These are more involved procedures, often done in an operating room, but they can provide a more complete picture of what’s going on.
In certain areas of the body—like the digestive tract or lungs—doctors may use an endoscopic biopsy. This involves inserting a thin, flexible tube with a camera and tiny instruments through the mouth, nose, or rectum to reach the area in question. A small piece of tissue can then be collected during the procedure. For skin problems or surface lesions, a punch biopsy is often used. In this procedure, a small, circular blade is used to remove a sample of all layers of skin, which is especially helpful in diagnosing skin cancers, rashes, or infections.
In cases where blood or bone marrow disorders are suspected, a bone marrow biopsy may be necessary. A needle is inserted, typically into the back of the hip bone, to remove a sample of bone marrow for testing. This type of biopsy helps diagnose conditions like leukemia, lymphoma, or anemia.
Finally, there is a newer, less invasive technique called a liquid biopsy. Instead of removing tissue, this method analyzes a sample of blood for tiny fragments of cancer DNA that tumors release into the bloodstream. While still being refined, liquid biopsies are showing promise in detecting certain cancers, monitoring treatment response, and spotting recurrence earlier than imaging alone.
What Happens During the Procedure?
For most people, the idea of a biopsy can sound intimidating, but the procedure is often simpler and quicker than expected. Many biopsies are outpatient procedures, meaning you can go home the same day. In most cases, local anesthesia is used to numb the area, so you won’t feel pain during the sampling—only a bit of pressure or mild discomfort.
If the biopsy is more involved, such as when a large tissue sample needs to be removed or the area is difficult to reach, sedation or general anesthesia may be used. This is more common with surgical biopsies, which are done in a hospital setting. Your doctor will explain in advance what type of anesthesia you’ll receive, and how to prepare. Biopsy procedures are typically minimally invasive, especially with needle, punch, or endoscopic biopsies.
Most take only a few minutes to an hour, depending on the method and location. After the sample is collected, it is carefully preserved and sent to a pathology laboratory. There, a pathologist—a doctor specially trained in examining cells and tissues—looks at the sample under a microscope.
The goal is to determine whether the tissue is normal or abnormal, and if abnormal, to identify the cause. For example, the pathologist might look for signs of cancer, infection, inflammation, or other changes in the tissue structure. In most cases, you can return to normal activities shortly after a biopsy, although your doctor may ask you to rest for the remainder of the day, especially if sedation was used.
What Can the Results Show?
Once your biopsy sample has been examined in the pathology lab, the results can provide crucial information to help guide your care. One of the most important things a biopsy can do is confirm or rule out cancer. If cancer is present, the pathologist can often determine the type of cancer, how aggressive it is, and whether it has features that might affect treatment.
In cancers like breast or prostate cancer, a biopsy can also reveal details such as tumor grade (how abnormal the cells look), hormone receptor status, or molecular markers like HER2 or BRCA mutations. These findings are key in choosing the most effective treatment plan. But biopsies are not just for cancer. They can also identify other conditions, such as infections, chronic inflammation, autoimmune diseases, or fibrosis (scarring) in organs like the liver or kidneys. This helps doctors determine the cause of symptoms and tailor treatment accordingly.
Sometimes, though, the results may be inconclusive. This means the sample didn’t contain enough tissue, or the changes were unclear. If that happens, your doctor may recommend a repeat biopsy or use additional tests to get a clearer answer. Whatever the outcome, biopsy results are a vital step in forming an accurate diagnosis and creating a plan that fits your specific condition.
Are There Any Risks?
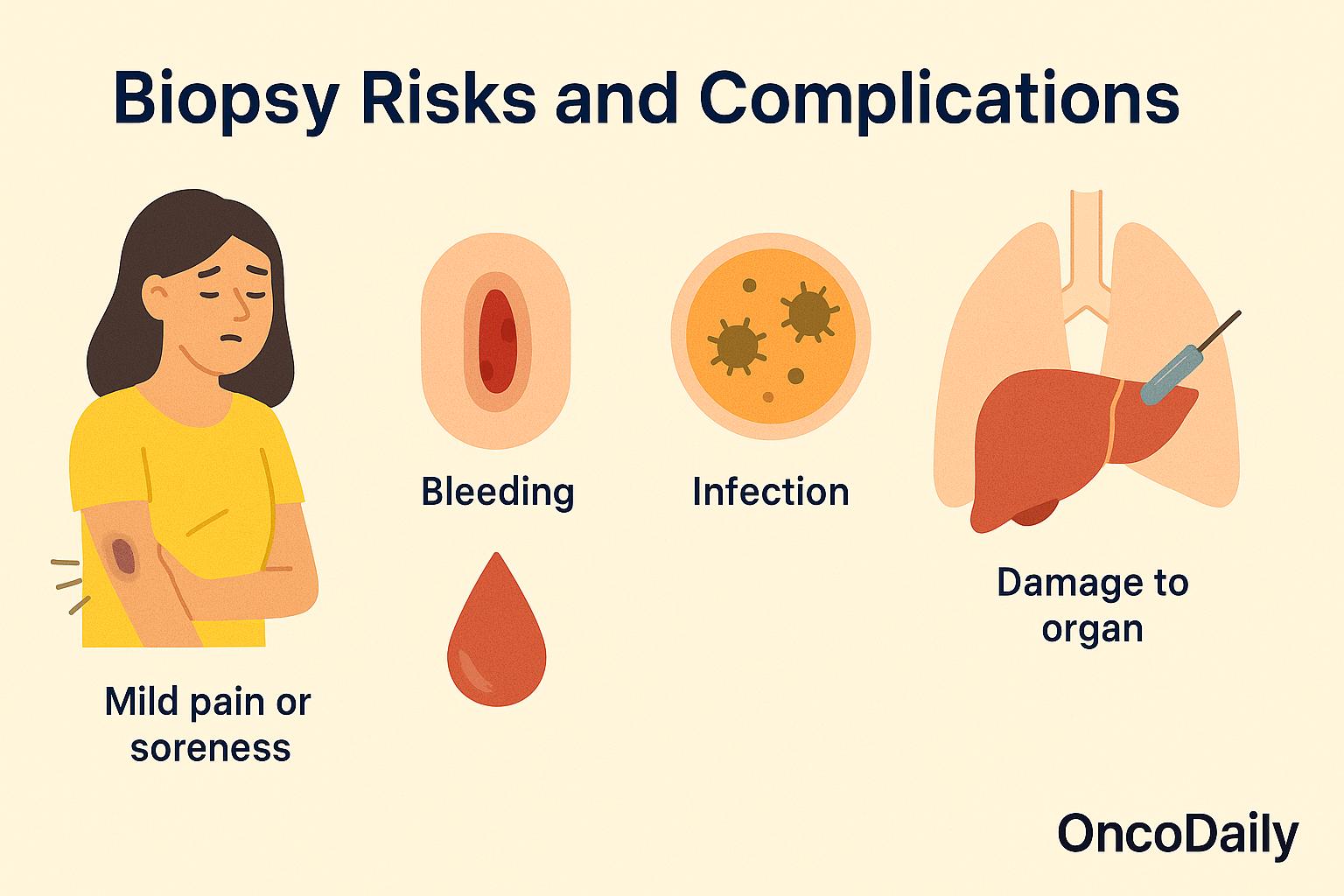
For most people, biopsies are low-risk procedures. They are done safely every day in clinics and hospitals around the world. Still, like any medical procedure, a biopsy can come with some minor side effects. The most common ones include bruising, mild pain or soreness at the site, and a small amount of bleeding. These symptoms usually go away within a few days and can be managed with rest, ice packs, or over-the-counter pain relievers if needed.
In some cases, there is a small risk of infection, especially if the biopsy involves deeper tissues or internal organs. Your doctor will take steps to reduce this risk, such as using sterile techniques and sometimes prescribing antibiotics. More serious complications are rare, but they can happen depending on the location and type of biopsy. For example, a lung or liver biopsy may carry a slightly higher risk of internal bleeding or injury to nearby structures. That’s why biopsies of these organs are usually done under image guidance—using ultrasound, CT, or MRI—to improve accuracy and safety.
Waiting for Results: What Comes Next?
After a biopsy, one of the most common questions patients have is, “When will I get my results?” In most cases, results are available within a few days to a week, depending on the complexity of the analysis. Some specialized tests—like genetic or molecular profiling—may take a little longer.
Once the results are ready, your doctor will schedule a follow-up visit to go over what they mean. This is an important conversation, as the biopsy results will help guide your next steps. You’ll learn whether the tissue showed signs of cancer, inflammation, infection, or another condition, and what kind of treatment or further testing might be needed. It’s important to remember that a biopsy is just one part of the larger diagnostic picture.
Doctors always interpret biopsy results in the context of your symptoms, imaging scans, blood tests, and medical history. Sometimes, the biopsy may raise more questions than answers, or show unclear results—especially if the sample was small or the abnormality is difficult to define. In such cases, your care team may recommend additional testing or even another biopsy to be certain.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is a biopsy?
A biopsy is a medical procedure where a small tissue or cell sample is taken from the body to examine it under a microscope.
Why do doctors recommend a biopsy?
Biopsies help diagnose conditions like cancer, infections, autoimmune diseases, or organ damage when something abnormal is found on an exam or scan.
Are all biopsies the same?
No, there are different types like needle biopsies, surgical biopsies, endoscopic biopsies, punch biopsies, and liquid biopsies—chosen based on location and purpose.
Does a biopsy mean I have cancer?
Not necessarily. A biopsy is used to determine if a mass or abnormality is cancerous, benign, infected, or related to another condition.
What happens during a biopsy?
Depending on the type, you may receive local anesthesia or sedation. A tissue sample is collected and sent to a lab for analysis.
How long does it take to get biopsy results?
Results usually come back within a few days to a week, though some genetic or molecular tests may take longer.
Is a biopsy painful?
Most biopsies involve only mild discomfort, especially with local anesthesia. More involved biopsies may cause temporary soreness.
Are biopsies safe?
Yes, biopsies are generally safe. Minor risks include bruising, soreness, bleeding, or infection—especially for deeper biopsies.
What do biopsy results show?
They can show whether the tissue is normal, cancerous, inflamed, infected, or damaged—helping guide treatment decisions.
What if the biopsy results are inconclusive?
Sometimes the sample may not provide clear answers. In such cases, doctors may recommend another biopsy or additional tests.