During BGICC 2026, Prof. Frédérique Penault-Llorca delivered a focused and practice-oriented lecture examining the contemporary role of frozen section analysis in sentinel lymph node (SLN) evaluation. Her presentation emphasized that frozen section should no longer be considered a routine procedure, but rather a selective tool reserved for specific clinical scenarios where results may meaningfully alter management.
Changing Clinical Context of Sentinel Node Assessment
Prof. Penault-Llorca began by highlighting how advances in surgical de-escalation have fundamentally altered the relevance of intraoperative SLN assessment. Data from pivotal trials have demonstrated that patients with one or two positive sentinel nodes often do not require completion axillary dissection when treated with appropriate radiotherapy. As a result, immediate intraoperative decisions based on frozen section findings frequently no longer influence surgical management.
In this context, the central question has shifted from detecting every microscopic deposit to identifying nodal disease that carries sufficient burden to change postoperative treatment decisions.
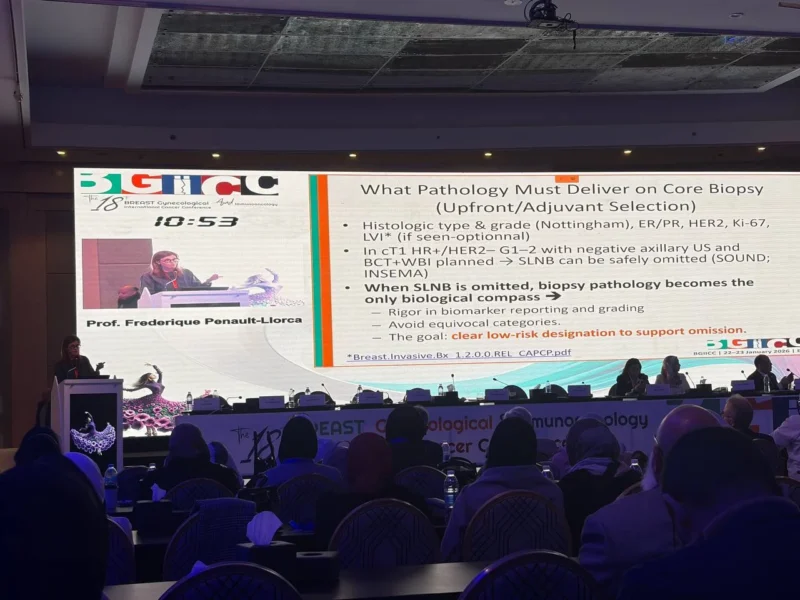
What Information Truly Matters in SLN Pathology
The lecture underscored that pathology reporting should focus on elements that influence downstream management. These include the number of involved nodes, the size of the largest metastatic focus, and clear classification of nodal involvement into isolated tumor cells (ITCs), micrometastases, or macrometastases.
While extracapsular extension should be documented when present, Prof. Penault-Llorca emphasized that limited extension does not necessarily translate into worse outcomes and does not automatically mandate escalation of axillary surgery. Its value lies primarily in comprehensive reporting rather than immediate surgical decision-making.
Frozen Section: From Routine to Selective Use
Frozen section analysis, once routinely performed during SLN surgery, has seen a substantial decline in use. Prof. Penault-Llorca explained that detecting ITCs or small micrometastases intraoperatively rarely impacts immediate management and may lead to unnecessary overtreatment.
Accordingly, frozen section should be reserved for cases where macrometastatic disease is strongly suspected and where identification would prompt an immediate change in surgical strategy, such as avoiding a second operation in selected patients.
Challenges in the Post-Neoadjuvant Setting
The role of frozen section becomes more complex after neoadjuvant systemic therapy. In this setting, lymph nodes may demonstrate fibrosis, treatment effect, or scattered residual tumor cells, making interpretation more challenging.
Prof. Penault-Llorca noted that patients may achieve pathological complete response in the breast while still harboring residual nodal disease. In such cases, accurate pathological assessment remains critical for guiding adjuvant systemic therapy escalation and radiotherapy planning. When uncertainty exists, comprehensive histological evaluation rather than reliance on frozen section alone is essential.
Importance of Detailed Pathology Reporting
The lecture emphasized the growing importance of meticulous pathology reporting in guiding personalized treatment. Key elements include documentation of clipped or targeted nodes, measurement of residual disease, assessment of treatment-related changes such as fibrosis or necrosis, and explicit description of extranodal extension when present.
Such detailed reporting supports multidisciplinary decision-making and ensures that axillary management aligns with the overall treatment strategy.
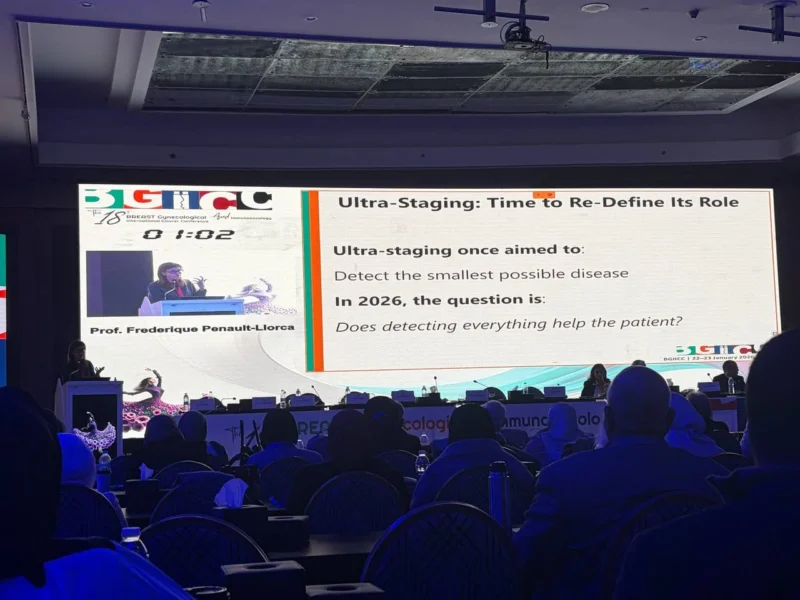
Does Detecting Everything Help the Patient?
A central theme of the presentation was a critical reassessment of pathological intensity. Prof. Penault-Llorca posed a fundamental question: does exhaustive detection of minimal disease improve patient outcomes? Based on current evidence, the answer is often no.
Excessively sensitive detection methods may identify disease that does not warrant treatment escalation, increasing the risk of overtreatment without clinical benefit. The modern goal of SLN pathology is therefore not maximal detection, but clinically meaningful stratification.
Current Position of Frozen Section
In conclusion, Prof. Penault-Llorca outlined a pragmatic role for frozen section analysis in contemporary breast cancer care. It is no longer a routine component of SLN evaluation, but a selective tool used primarily to avoid reoperation in carefully chosen cases. For most patients, definitive paraffin-section pathology provides sufficient information to guide optimal treatment.
As axillary management continues to evolve toward de-escalation, pathology practice must adapt accordingly—prioritizing relevance, precision, and multidisciplinary integration over exhaustive intraoperative detection.
More posts about BGICC on OncoDaily