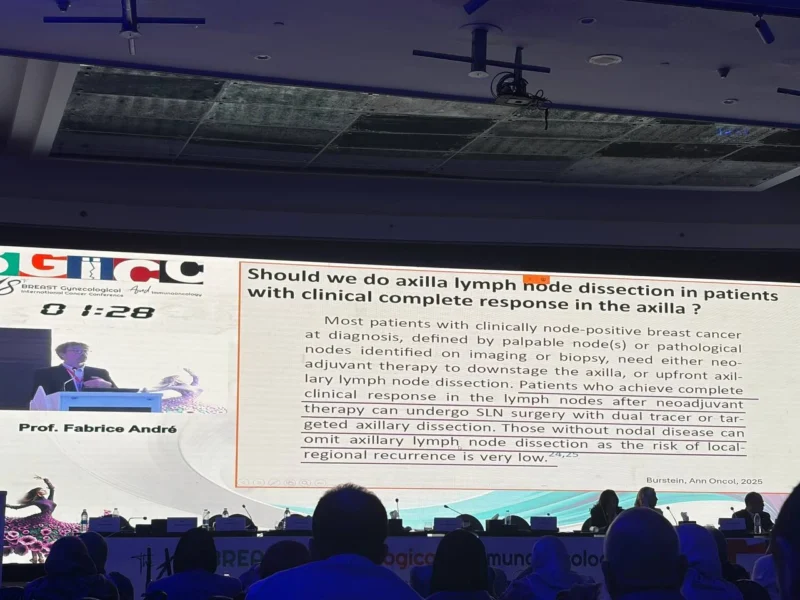
During Breast Gynecological & Immunooncology International Cancer Conference (BGICC) 2026, on Day 2, within the session “Solving the Axillary Dilemma 2026,” Prof. Fabrice André, ESMO President 2025-2026, Institut Gustave Roussy, delivered a forward-looking lecture on how major advances in systemic therapies are fundamentally reshaping the role of axillary surgery in breast cancer.
His presentation focused on how improved tumor control at the systemic level increasingly enables surgical de-escalation without compromising oncologic outcomes.

Systemic Therapy as a Driver of Surgical De-escalation
Prof. André began by emphasizing a paradigm shift: the extent of surgery is no longer determined solely by anatomical disease burden, but increasingly by biological response to systemic treatment. Modern systemic therapies—particularly targeted agents and immunotherapy—have substantially increased rates of deep pathological response, directly affecting the necessity of extensive axillary interventions.
He highlighted that across multiple disease subtypes, effective systemic treatment can eradicate microscopic nodal disease, thereby reducing the added value of aggressive axillary surgery.
Pathological Complete Response and Axillary Management
A central theme of the lecture was the growing relevance of pathological complete response (pCR) as a decision-modifying endpoint. Prof. André reviewed data showing that patients achieving pCR after neoadjuvant systemic therapy—especially in HER2-positive and triple-negative breast cancer—exhibit very low residual nodal burden.
These findings support strategies that avoid axillary lymph node dissection in favor of less invasive approaches such as sentinel lymph node biopsy or targeted axillary dissection, and in selected cases, raise the question of whether surgery can be omitted altogether.
Conversion to Breast-Conserving and Less Morbid Surgery
Advances in systemic therapy were also shown to increase conversion rates from mastectomy to breast-conserving surgery, indirectly contributing to axillary de-escalation. As tumor downstaging improves, the surgical objective shifts from maximal clearance to optimal balance between disease control and long-term morbidity.
Prof. André stressed that this evolution reflects a broader move toward personalized local therapy, aligned with systemic treatment response rather than historical staging rules.
Evidence Supporting Reduced Axillary Intervention
The lecture reviewed accumulating clinical and real-world evidence demonstrating low axillary recurrence rates in patients managed with reduced surgical approaches following favorable systemic responses. Studies evaluating sentinel node biopsy, targeted axillary dissection, and radiotherapy-based strategies consistently show excellent regional control in carefully selected patients.
Importantly, Prof. André underscored that these outcomes are achieved while significantly reducing complications such as lymphedema, pain, and functional impairment.
Omission of Axillary Surgery: Where Are We Now?
While acknowledging the promise of complete omission of axillary surgery, Prof. André was cautious. He noted that such strategies must remain biologically driven and evidence-based, with careful patient selection. Ongoing trials are expected to clarify which subgroups can safely avoid axillary surgery entirely without jeopardizing long-term outcomes. He emphasized that systemic therapy response, imaging assessment, and tumor biology must be integrated to guide these decisions.
Future Directions
In closing, Prof. André highlighted that the future of axillary management lies in interdisciplinary integration—linking systemic therapy efficacy, imaging, pathology, and surgical strategy. As systemic treatments continue to improve, axillary surgery is likely to become increasingly selective, individualized, and in some cases unnecessary. The key message was clear: advances in systemic therapy are not merely complementary to surgery—they are redefining its role.