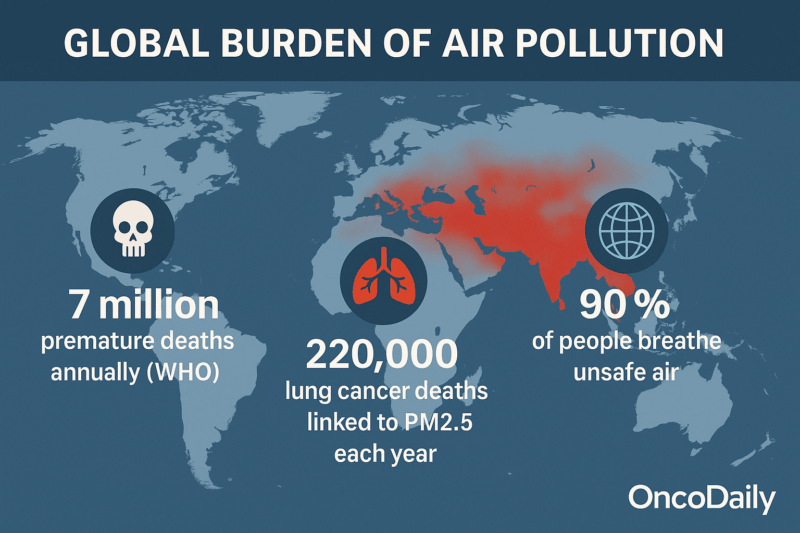
Air pollution remains one of the most significant environmental health risks worldwide, contributing to an estimated 7 million premature deaths annually according to the World Health Organization (WHO). Beyond its well-known impacts on respiratory and cardiovascular health, air pollution is increasingly recognized as a major contributor to cancer risk. Fine particulate matter (PM2.5), polycyclic aromatic hydrocarbons (PAHs), and heavy metals are among the key carcinogens in polluted air. Long-term exposure to PM2.5 alone is estimated to cause around 220,000 lung cancer deaths globally each year. These pollutants trigger carcinogenesis through mechanisms such as DNA damage, chronic inflammation, and oxidative stress.

Photo: Depositphotos
Global exposure varies, with over 90% of the world’s population living in areas where air pollution exceeds WHO safety guidelines. Urban and industrial regions demonstrate the highest exposure levels, as shown in data from the Global Burden of Disease (GBD) study. Cancer types linked to air pollution include predominantly lung cancer, with emerging evidence associating bladder and other cancers as well. Vulnerable populations children, elderly, and those with pre-existing health conditions face disproportionate risks. Understanding the pathophysiology and epidemiology of pollution-related cancers is essential for medical and public health strategies combining pollution control with targeted prevention.
This article explores the medical and cancer-related impacts of air pollution, detailing key carcinogenic pollutants, global exposure patterns, mechanisms of cancer development, affected populations, and strategies to reduce the cancer burden related to air pollution. These insights draw on current global health data and scientific literature from WHO and GBD reports, reflecting the growing challenge of reducing air pollution’s cancer burden worldwide.
Overview of Air Pollution and Its Impact on Human Health
Air pollution remains a critical global health crisis, responsible for an estimated 7 million premature deaths annually worldwide, according to the World Health Organization (WHO). This complex mixture of pollutants includes fine particulate matter (PM2.5), nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), and carbon monoxide (CO). Fine particulate matter, due to its small size, penetrates deep into the lungs and bloodstream, causing about 4.1 million deaths each year from heart disease, stroke, chronic respiratory diseases, and lung cancer. Exposure to nitrogen dioxide and ozone worsens respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD), affecting hundreds of millions globally. Vulnerable populations such as children, the elderly, pregnant women, and those with pre-existing conditions face heightened risks.
Scientific literature complements these findings by quantifying the burden and exploring biological mechanisms. For example, a 2023 European Environment Agency report estimates that lowering PM2.5 levels to WHO guidelines in Europe could prevent over 250,000 deaths annually, primarily from ischemic heart disease and lung cancer. A 2024 Lancet Public Health study highlights that short-term PM2.5 exposure contributes significantly to cardiovascular and respiratory mortality globally, with urban areas in Asia and Africa disproportionately affected. Moreover, research indicates that personal exposure to nitrogen dioxide can induce airway inflammation and impair lung function through epigenetic modifications, elucidating how NO2 exacerbates respiratory diseases.
Despite interventions, low- and middle-income countries endure a disproportionate share of air pollution exposure and health impacts, largely due to urbanization and less strict pollution controls. The WHO has recently updated air quality guidelines, lowering recommended safe PM2.5 exposure levels, reflecting growing evidence of harm even at low pollutant concentrations. Meeting these guidelines globally could dramatically reduce the death and disease burden. The World Health Assembly in 2025 endorsed a global roadmap targeting a 50% reduction in premature deaths from anthropogenic air pollution by 2040, emphasizing integrated policy actions across sectors such as energy, transport, and industry to achieve safer air quality and protect public health.
This body of evidence underscores the urgent need for coordinated healthcare and policy strategies to reduce air pollution exposure and mitigate its extensive health consequences, including the heightened risks of cancer and chronic diseases linked to ongoing global exposure.
Carcinogenic Components of Air Pollution and Their Medical Significance
Carcinogenic components of air pollution exert profound molecular and medical effects that significantly elevate cancer risk, particularly lung cancer. Fine particulate matter (PM2.5), laden with polycyclic aromatic hydrocarbons (PAHs) and heavy metals such as cadmium, lead, and chromium, initiates carcinogenesis through a cascade of complex biological mechanisms. Upon inhalation, PM2.5 and its toxic constituents penetrate deep into the respiratory tract, triggering chronic inflammation and oxidative stress by generating reactive oxygen species (ROS). This pro-inflammatory milieu activates signaling pathways such as NF-κB and PI3K/Akt, which promote cellular proliferation, migration, and epithelial-mesenchymal transition (EMT), all key steps in tumor progression.
At the epigenetic level, PM2.5 exposure disrupts DNA methylation patterns, particularly in tumor suppressor genes like TP53, and alters the expression of DNA repair genes including ERCC1 and MGMT. Changes in DNA methyltransferases (DNMTs) and ten-eleven translocation (TET) enzymes modulate DNA repair capacity, influencing mutation accumulation. Moreover, air pollution induces differential expression of oncogenic and tumor suppressive microRNAs and long non-coding RNAs, reshaping gene regulatory networks that govern cancer cell survival and metastasis. Experimental models highlight the role of PM2.5-induced hypomethylation and transcriptional activation of genes promoting malignancy, such as STC2, implicated in immune evasion and cancer progression.
Elevated PAH concentrations in PM2.5 create DNA adducts that can evade repair, leading to stable mutations. These molecular insults are corroborated by epidemiological evidence demonstrating that lung tumors in highly polluted regions harbor triple the number of mutations compared to low-exposure areas. This multi-hit process involves initiation, promotion, and progression phases, with disruption of cell cycle regulators, induction of chromosomal instability, and inhibition of apoptosis fueling tumorigenesis. These intricate molecular events underscore the critical medical significance of carcinogenic components in air pollution, emphasizing the urgent need for targeted public health interventions and cancer prevention strategies.
Air Pollution: Unequal Exposure and Health Effects Worldwide
Global air pollution exposure exhibits stark disparities between low-income and high-income countries, profoundly influencing health outcomes. According to a 2025 study covering the Western Pacific Region (WPRO), high-income countries such as Australia, New Zealand, and Japan exhibit markedly lower mean PM2.5 concentrations ranging from approximately 7 to 13 μg/m³ compared to upper-middle and lower-middle-income countries like China and Cambodia, where levels reach as high as 50 μg/m³ and above. These differences correlate strongly with diverse regulatory frameworks, technological advances, and healthcare infrastructure.
Low- and middle-income countries (LMICs) disproportionately bear the brunt of unsafe air pollution exposure. Data from a 2022 World Bank report indicate that about 80% of the population exposed to unhealthy PM2.5 levels live in LMICs, including 716 million people living in extreme poverty (under $1.90/day). Major contributors include rapidly industrializing economies relying on polluting industries and biomass burning for cooking and heating. In contrast, high-income countries benefit from stricter environmental regulations, cleaner energy sources, and expansive monitoring networks, leading to lower population-weighted PM2.5 averages and delayed onset of air pollution-related health declines.
Unequal capacity for pollution control has manifested in health disparities: in WPRO countries, the adverse impact of PM2.5 on healthy life expectancy (HALE) occurs at younger ages in LMICs (around 74 years) compared to high-income countries (around 79 years), confirming a more significant and earlier burden of disease. Furthermore, income-related resilience factors, such as policy enforcement, healthcare access, and public awareness, mitigate the health consequences in wealthier nations.
However, despite improvements in some regions, global inequalities in air pollution exposure remain high and are increasing, as documented by a 2025 Nature study showing that developing regions experience PM2.5 inequalities over 60% higher than developed countries. Strong policy shifts in major economies like China and the US have shown that reducing inequalities is possible but requires sustained investment.
This gap underscores the urgent need for targeted air quality interventions in low-income settings, addressing both outdoor and indoor sources of PM2.5 to alleviate the disproportionate cancer and health burdens borne by the world’s most vulnerable populations.
How Air Pollution Contributes to Cancer Development or Pathophysiology
Air pollution contributes to cancer development through several biological mechanisms that start when harmful pollutants enter the lungs and bloodstream. Fine particulate matter (PM2.5), polycyclic aromatic hydrocarbons (PAHs), and heavy metals present in polluted air generate reactive oxygen species (ROS), which cause damage to DNA and cell structures. This oxidative stress triggers chronic inflammation, a key driver of cancer initiation and progression.
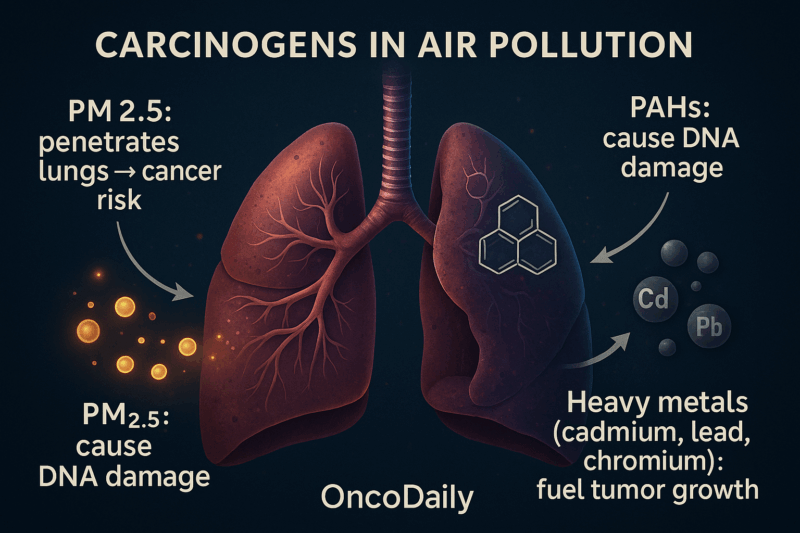
These pollutants also lead to genetic mutations and changes in gene regulation, such as DNA methylation alterations that can silence tumor suppressor genes like TP53. These molecular changes disrupt normal cell repair and death processes, allowing abnormal cells to grow uncontrollably. Studies show that for every 10 µg/m³ increase in long-term PM2.5 exposure, lung cancer risk rises by 8-15%. The World Health Organization estimates that ambient air pollution causes about 220,000 lung cancer deaths globally each year.
Chronic inflammation caused by air pollution creates an environment that supports tumor growth by promoting cell proliferation, new blood vessel formation, and preventing programmed cell death. This combination of effects makes air pollution an important but often overlooked cause of cancer, especially lung cancer, emphasizing the need for pollution reduction to protect public health.
Epidemiology of Air Pollution-Related Cancers
Air pollution has emerged as a major environmental risk factor for cancer, particularly lung cancer, contributing substantially to the global disease burden. Epidemiological evidence, especially from large cohort studies and meta-analyses, shows that every 10 µg/m³ increase in fine particulate matter (PM2.5) is linked to an 8–15% higher risk of lung cancer incidence and mortality. Globally, ambient air pollution was responsible for an estimated 265,000 lung cancer deaths in 2017—about 14% of all such deaths—making it the second leading cause after tobacco smoking. The risk is unevenly distributed, with higher population-attributable fractions in low- and middle-income countries (LMICs) such as China (20.5%) compared to high-income countries like the United States (4.7%).
Advanced statistical models combine air pollution exposure data from monitoring stations with cancer registry information and socio-demographic factors to refine risk estimates. Spatial and temporal analytics identify pollution hotspots where cancer incidence rates are disproportionately higher, especially in urban and industrial areas. Studies also report associations between air pollution and other cancers, including breast, liver, bladder, and nasopharyngeal cancers, though evidence is strongest for lung cancer.
Machine learning and geospatial analysis enable integration of satellite data, ground-based sensors, and health records, improving accuracy in exposure assessment and risk prediction. These epidemiological and analytical insights emphasize the urgent need for targeted pollution control measures and cancer prevention strategies, particularly in vulnerable and highly exposed populations worldwide.
What Medical and Public Health Strategies Can Reduce Cancer Risk from Air Pollution?
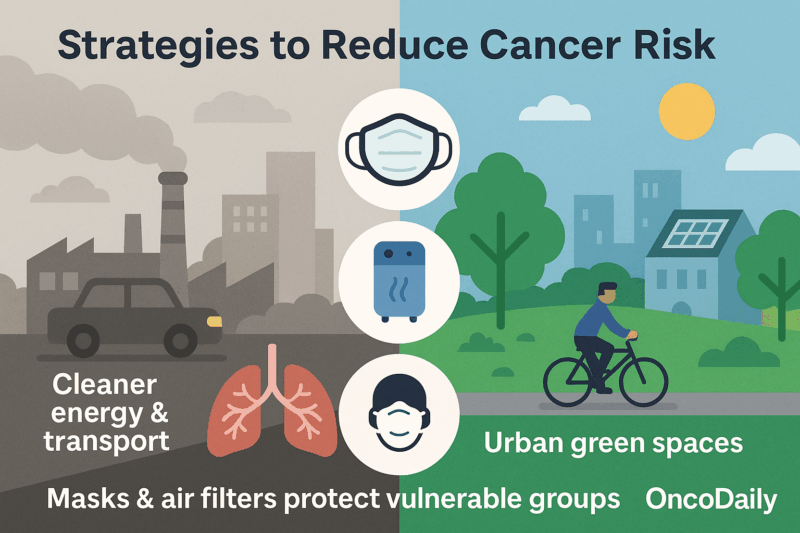
Medical and public health strategies to mitigate cancer risk from air pollution focus on reducing exposure through multi-level interventions informed by robust evidence. According to the World Health Organization (WHO), more than 99% of the global population breathes polluted air, contributing to roughly 18.6% of lung cancer deaths globally. Effective mitigation involves stringent air quality standards and regulations targeting emissions from industry, transportation, and residential sources. Transitioning to cleaner energy, promoting electric vehicles, and expanding green urban spaces reduce both pollution levels and associated cancer risk.
From a medical perspective, healthcare providers play a crucial role in prevention by raising awareness, advising patients especially those vulnerable such as children, the elderly, and cancer survivors to minimize exposure on high pollution days, and integrating environmental risk factors into cancer screening and care plans. Public health campaigns promoting active transport (walking, cycling) not only reduce air pollution but also confer broad health benefits, including lower cancer risks linked to improved physical activity and reduced obesity.
Policy-driven emission reductions, combined with technological innovations and community engagement, have proven successful in lowering pollution levels and related cancer incidence in high-income countries, as shown by the ESCAPE cohort studies in Europe. However, low- and middle-income countries face greater challenges due to limited resources and regulatory enforcement, underscoring the need for international support and equity-focused interventions. Continuous monitoring, data-driven risk assessment, and cross-sector collaboration are essential to optimize these strategies and achieve meaningful reductions in air pollution-related cancer burden worldwide.
You Can Also Read How Aging Populations Are Reshaping Global Cancer Trends or The Silent Shift by OncoDaily

Protecting Yourself from Air Pollution: Practical Steps for Health
Air pollution poses serious risks to human health, but there are effective steps individuals can take to reduce their exposure and protect themselves. First, it is important to stay informed by regularly checking local air quality forecasts and alerts through apps, websites, or news outlets. On days when pollution levels are high, especially for fine particulate matter (PM2.5), limit outdoor activities and avoid intense exercise outdoors, which increases pollutant inhalation.
Improving indoor air quality is also crucial since people spend much of their time indoors. Keep windows and doors closed during high pollution periods to prevent outdoor pollutants from entering. Use air purifiers equipped with HEPA filters that can trap harmful particles like dust, pollen, and PM2.5. Avoid smoking indoors and minimize the use of products that emit volatile organic compounds (VOCs), such as certain cleaners or paints.
When air pollution is elevated, wearing protective masks like N95 respirators can significantly reduce inhalation of fine particles and harmful gases. Masks should fit properly to be effective, particularly for vulnerable groups, including children, elderly, pregnant women, and those with heart or lung diseases.
Lifestyle adjustments can also help – opt for cleaner forms of transportation such as walking, cycling, carpooling, or public transit to reduce pollution emissions. Limit burning wood, coal, or biomass for heating and cooking, as these contribute locally to indoor and outdoor pollution. Planning outdoor activities for times of better air quality, usually early morning or after rain, also reduces exposure.
Finally, supporting public policies aimed at reducing emissions from vehicles, industry, and other sources is essential for lasting improvements. Community advocacy can encourage stricter air quality regulations and the expansion of monitoring networks.
By combining personal protection measures with broader environmental actions, individuals and communities can lower health risks posed by air pollution and contribute toward cleaner, healthier air for all. These recommendations align with guidance from the World Health Organization and leading environmental health agencies worldwide.
In conclusion, air pollution is a major and preventable cause of cancer, particularly lung cancer, accounting for approximately 220,000 deaths worldwide each year. Research shows that every 10 µg/m³ increase in PM2.5 exposure raises lung cancer risk by up to 15%. While smoking remains a leading cause, air pollution poses a substantial and growing threat, especially in urban and low-income areas. Reducing air pollution through stricter regulations, cleaner energy, and public awareness can significantly lower cancer risk and improve global health outcomes. Continued research and policy action are essential to protect vulnerable populations and reduce the cancer burden linked to polluted air.
You Can Also Read The Day After a Nuclear Bomb: Generational Damage and the Silent Cancer Epidemic by OncoDaily
Written by Marine Marashlian, MDc.