Oral mucositis and dysphagia are two of the most debilitating toxicities experienced by patients undergoing chemoradiation therapy (CRT) for head and neck cancers (HNC). At MASCC 2025 Parallel Session 13, Dr. Satheesh Kumar Poolakkad Sankaran and colleagues presented a landmark meta-analysis investigating the causal association between these conditions. Their findings were featured in the session titled “The hidden role of the nervous system in mucositis-associated pain and gastrointestinal dysfunction caused by cancer therapy,” highlighting the complex interplay between treatment-related toxicities and neural pathways.
While both OM and DYS are well-documented complications of CRT in HNC patients, the synchronistic development and interrelated pathophysiology of these two toxicities have not been rigorously explored. This meta-analysis represents the first systematic effort to quantify their association and evaluate comparative treatment approaches.
Background: Why Study OM and Dysphagia Together?
Oral mucositis, characterized by painful ulcerations and inflammation of the oral mucosa, occurs in up to 80% of patients receiving CRT for HNC. It often leads to significant nutritional compromise, treatment interruptions, and reduced quality of life. Dysphagia—difficulty swallowing—is another debilitating toxicity that may arise concurrently but is frequently considered independently. Given their temporal overlap and anatomical proximity, the hypothesis of a causal relationship warrants thorough investigation.
Methods: A Rigorous PRISMA-Based Approach
The investigators conducted a comprehensive literature review using PubMed and EBSCO databases through December 2024, adhering to PRISMA guidelines. Of 2,458 screened articles, 53 studies passed initial quality assessments and were included for causal pathway analysis. A total of 13 randomized controlled trials (RCTs) comprising 1,776 patients (669 in experimental arms and 1,107 receiving standard care) were included in the final meta-analysis and comparative effectiveness research (CER).
The statistical methodology included a fixed-effects meta-analysis using the inverse variance method to calculate pooled risk ratios (RRs). In parallel, a network meta-analysis created a hierarchy of CRT regimens based on the likelihood of OM-DYS co-occurrence.
Results: A Modest but Statistically Significant Link
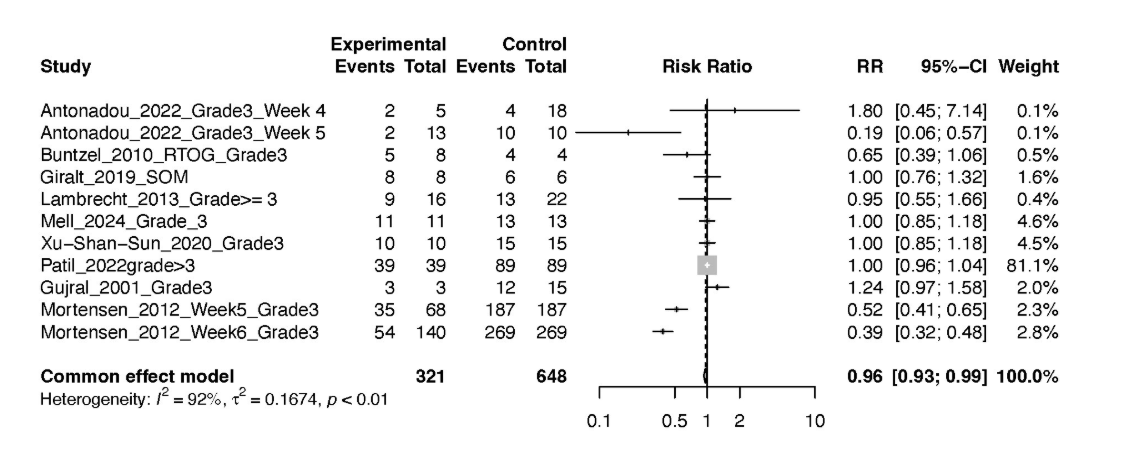
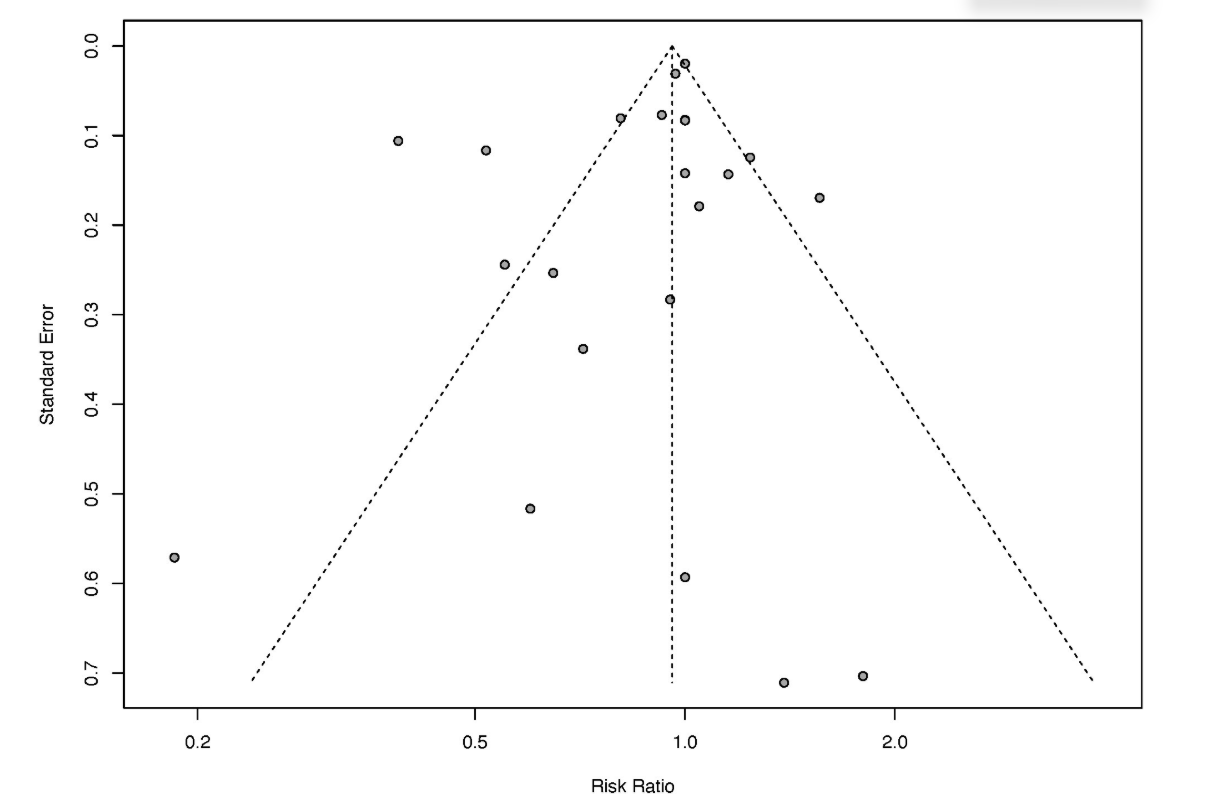
The meta-analysis revealed that the RR of developing dysphagia in patients who developed oral mucositis was 0.96 (95% CI: 0.93–0.99, p < 0.01). While the effect size is modest, it is statistically significant. The analysis showed considerable heterogeneity (I² = 85%, τ² = 0.1074), reflecting variability in OM grading systems, patient populations, and treatment regimens.
A subgroup analysis focused on grade 3 or higher mucositis confirmed the findings, with an RR of 0.96 (95% CI: 0.93–0.99), and even higher heterogeneity (I² = 92%, τ² = 0.1674). These consistent results strengthen the hypothesis that OM may contribute directly or indirectly to the risk of dysphagia.
Comparative Effectiveness Research: Cisplatin vs. Docetaxel
One of the key findings from the CER was that docetaxel plus radiotherapy (RT) was less likely to result in concurrent OM and dysphagia compared to the more widely used cisplatin plus RT regimen. This was supported by a P-score of 0.75, indicating a favorable safety profile in terms of mucosal and swallowing toxicities. These insights may have important clinical implications for optimizing CRT regimens in HNC.
Interpretation and Implications
The data presented suggest that while mucositis management remains a priority in HNC care, clinicians must also consider its broader systemic and functional consequences, particularly its impact on swallowing. The findings also highlight a major research gap: despite OM being widely studied, dysphagia has been the only downstream toxicity consistently reported in RCTs, leaving the full spectrum of mucositis-associated complications unexplored.
Given the potential involvement of inflammatory, neural, and anatomical mechanisms, further studies are needed to explore the neurophysiological pathways linking OM and DYS, including the role of sensory nerves and cytokine signaling.
Conclusion: A Call for Integrated Toxicity Management
Dr. Sankaran and colleagues emphasized that this analysis represents a preliminary yet foundational step in understanding the causal links between treatment-related toxicities in oncology. As mucositis continues to be a major challenge in HNC, its association with swallowing dysfunction deserves more focused investigation and clinical attention. Future trials should adopt a multidimensional toxicity assessment framework, integrating oral, pharyngeal, and neurologic endpoints.