American Society of Hematology (ASH) continues to shape the future of blood disorders research and clinical care worldwide. Each year, the ASH Annual Meeting sets the global agenda in hematology, unveiling breakthrough data, innovative therapies, and practice-changing insights that redefine patient outcomes.
Highlights of ASH in the Mediterranean, Middle East, and North Africa (MENA) brings these transformative discoveries directly to the region, gathering leading experts for two days of high-impact scientific exchange in Istanbul, Türkiye. February 13–14, 2026, Hilton Istanbul Bomonti Hotel & Conference Center.
Designed to bridge global science with regional practice, this meeting explores the most influential and novel research presented at the latest ASH Annual Meeting spanning malignant and benign hematology, hemostasis, thrombosis, and emerging therapies. Participants gain practical insights on how to translate cutting-edge evidence into real-world clinical application.
This year’s discussion is further enriched by expert commentary and key insights from Dr. Heghine Khachatryan, Co-Founder and Chief Editor of Hemostasis Today and MD at Yeolyan Hematology and Oncology Center. Her five key reflections from ASH 2026 highlight the trends, innovations, and paradigm shifts that clinicians across the region need to watch closely.
1. ASH Highlights 2026 | Racial and Ethnic Disparities in the Diagnosis of VTE in Pregnancy
One of the most compelling sessions explored racial and ethnic disparities in the diagnosis and healthcare utilization patterns of venous thromboembolism (VTE) during pregnancy.
The presentation began with a clinical vignette: a 24-year-old pregnant Sudanese woman presenting with dyspnea and restlessness. Beyond the clinical suspicion of VTE, the case highlighted critical real-world barriers—language limitations, communication gaps, and potential diagnostic delay.
Study Overview
Using large population-based administrative and clinical databases (ICES, BORN Ontario, Immigration and Citizenship registries, laboratory and hospital datasets), investigators examined:
• Healthcare encounters preceding confirmed VTE diagnosis
• Resource utilization following VTE diagnosis
• Racial and ethnic differences in diagnostic patterns
The cohort included 442,816 pregnancies (2012–2023) with 1,793 imaging-confirmed VTE events.
Key Findings
• VTE incidence per 1000 pregnancies:
• White: 4.4
• Black: 4.1
• Asian: 2.2
• Prior to confirmed VTE, emergency department visits increased dramatically—up to 18-fold higher in some groups—suggesting missed opportunities for earlier diagnosis.
• Black patients were more likely to experience diagnostic delays influenced by:
• Reduced pulse oximeter accuracy in darker skin tones
• Under-recognition of clinical signs such as erythema
• Implicit bias and systemic inequities
• Communication barriers
Practice Implications
The session emphasized that:
• A “normal” SpO₂ does not guarantee safety in patients with darker skin tones occult hypoxemia must be considered.
• Equity-focused clinical reasoning is essential.
• Awareness of device limitations, implicit bias, and cultural barriers is necessary to prevent delayed diagnosis and adverse outcomes.
Clinical Reflection
This presentation was a powerful reminder that precision medicine must include equity.
Improving VTE outcomes in pregnancy requires not only diagnostic algorithms but also structural awareness and system-level change.
Scientific excellence must go hand in hand with health equity.
2. “ASH Highlights 2026 | Management of Thrombosis in Antiphospholipid Syndrome (APS) with Chronic Kidney Disease (CKD)
One of the most clinically thought-provoking sessions addressed anticoagulation strategies in patients with thrombotic APS complicated by chronic kidney disease — a population in whom therapeutic decision-making is particularly challenging.
⸻
Clinical Case
A 36-year-old woman with APS:
• History of three early pregnancy losses
• Persistent isolated aCL IgG positivity
• Subsequent right tibial vein thrombosis
• Serum creatinine: 3.5 mg/dL (CKD stage 3–5 range)
• Marked INR instability on warfarin (1.1–10)
• Inability to maintain therapeutic anticoagulation
This raised the critical question:
Can a patient with thrombotic APS and CKD be safely switched to a DOAC?
⸻
Current Consensus in Thrombotic APS
• Warfarin remains first-line therapy for thrombotic APS.
• DOACs are not recommended in high-risk APS (triple positivity or arterial events).
• DOACs may be considered in selected low-risk APS patients (single antibody positivity, venous events only).
Prior randomized trials have shaped this caution:
• RAPS (2016): Rivaroxaban non-inferior in VTE-only APS.
• TRAPS (2018): Increased recurrent arterial events with rivaroxaban in triple-positive APS.
• ASTRO-APS (2022): Higher thrombotic stroke rates in the apixaban arm.
Collectively, these studies discouraged DOAC use in high-risk APS.
⸻
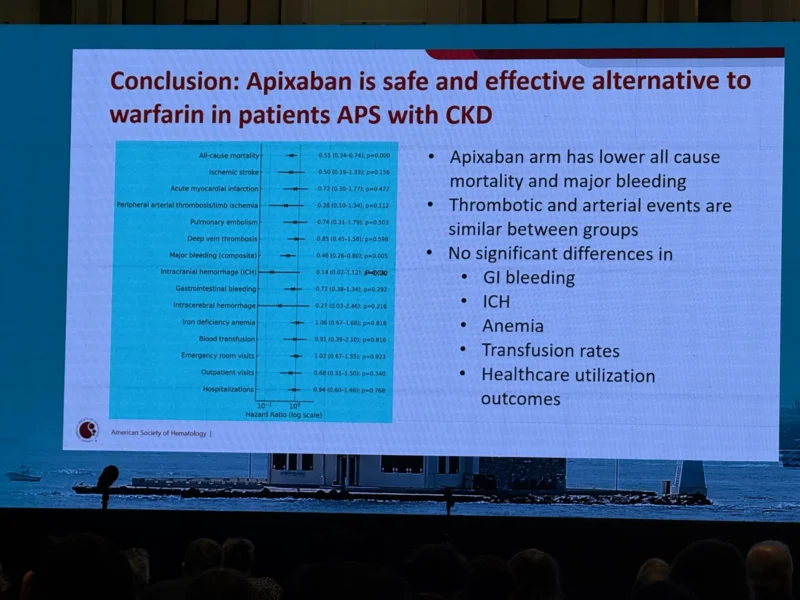
New Real-World Evidence: APS with CKD
A retrospective propensity-matched cohort study (TriNetX database) evaluated:
• Adult patients with APS and stage 3–5 CKD
• Newly initiated on apixaban vs warfarin
• 523 patients in each cohort
Key Findings:
• Lower all-cause mortality in the apixaban arm
• Reduced major bleeding
• Comparable rates of thrombotic and arterial events
• No significant differences in:
• Gastrointestinal bleeding
• Intracranial hemorrhage
• Anemia
• Transfusion requirements
• Healthcare utilization outcomes
Conclusion
In this real-world cohort, apixaban appeared to be a safe and effective alternative to warfarin in selected patients with APS and CKD.
⸻
Clinical Reflection
While warfarin remains the standard of care in high-risk APS, these findings suggest that in carefully selected patients — particularly those with CKD and unstable INR control — apixaban may represent a reasonable therapeutic option.
Management of APS is not uniform; it requires individualized risk stratification, careful evaluation of antibody profile, thrombotic phenotype, renal function, and bleeding risk.
This session highlighted the evolving complexity of anticoagulation in APS — where evidence, clinical judgment, and patient-specific factors must intersect.”
3. “ASH Highlights – Day 3 | Dual Antithrombotic Therapy in Acute VTE
One of the most thought-provoking sessions of the third day focused on the role of dual antithrombotic therapy (DAT) in patients with acute venous thromboembolism (VTE), based on large RIETE registry data and propensity-matched analysis.
Study population:
132,679 patients with confirmed acute VTE (2001–2025)
4,248 received dual therapy with concomitant antiplatelet treatment
Mean age of the matched cohort: 71 years
Key Findings
Primary Outcomes (2-year follow-up):
• All-cause mortality: 8.1% vs. 23.3%
HR 0.40 (95% CI 0.34–0.47), P<0.001
• Net adverse clinical events (NACE): 21.7% vs. 39.2%
HR 0.57 (95% CI 0.52–0.62), P<0.001
These results suggest a substantial reduction in mortality and overall adverse events among patients receiving DAT compared with anticoagulation alone.
Secondary Outcomes:
• Recurrent VTE: no statistically significant difference
• Increased bleeding risk observed with DAT
(Any bleeding HR 1.36; Major bleeding HR 1.28)
Importantly, DOAC-based dual therapy appeared to demonstrate a more favorable risk–benefit profile, without a significant increase in bleeding compared with anticoagulation monotherapy.
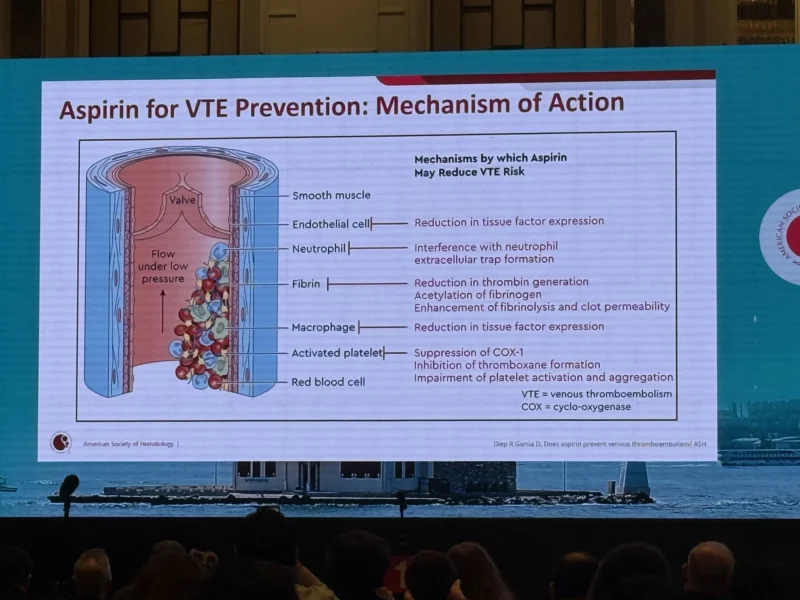
Mechanistic Insights
The session also revisited aspirin’s role in VTE prevention, highlighting pleiotropic mechanisms beyond platelet COX-1 inhibition, including:
• Modulation of tissue factor expression
• Effects on thrombin generation
• Interference with neutrophil extracellular trap formation
• Enhancement of fibrinolysis
Clinical Reflection
This analysis challenges us to reconsider how we individualize therapy in older, high-risk VTE populations—particularly those with concomitant cardiovascular disease requiring antiplatelet therapy.
Balancing thrombotic protection against hemorrhagic risk remains central to precision hemostasis.
Grateful to be part of these stimulating scientific discussions that continue to refine our understanding of thrombosis management.”
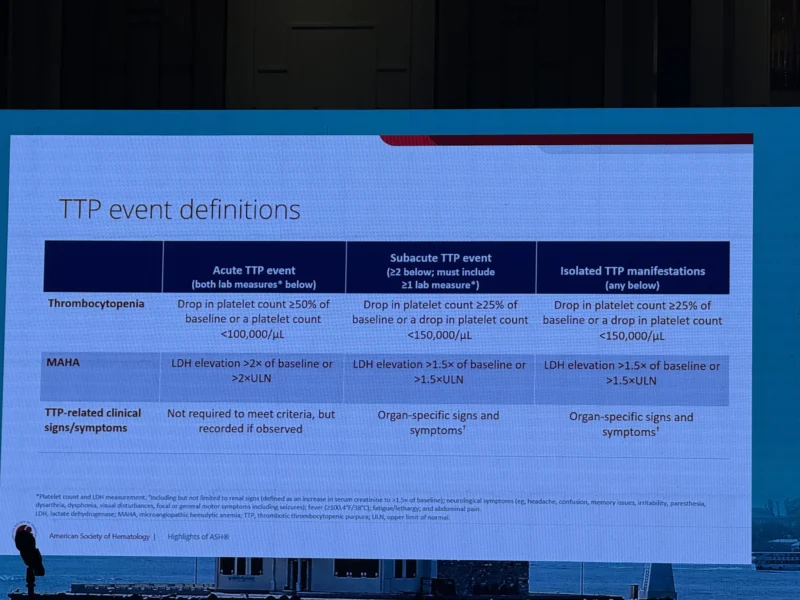
4. “ASH Highlights 2026 – Advances in Thrombotic Thrombocytopenic Purpura (TTP)
One of the most impactful sessions today focused on emerging therapeutic strategies in immune TTP (iTTP) and congenital TTP (cTTP), particularly CD38-targeted therapy and recombinant ADAMTS13 replacement.
-Daratumumab in Immune TTP (iTTP)
Data from the international, multicenter DarTTP study demonstrated:
▪️ Rapid ADAMTS13 remission in 75% of patients with iTTP who were refractory or intolerant to rituximab and other immunosuppressive therapies
▪️ Sustained remission (>6 months) in approximately two-thirds of responders
▪️ Targeting CD38+ plasma cells offers a promising strategy in cases where B-cell depletion alone is insufficient
These findings represent an important advancement in the management of refractory iTTP and provide renewed hope for patients at high risk of relapse.
-Congenital TTP (cTTP)
The session also highlighted a clinical case discussion and phase 3 data on recombinant ADAMTS13 (rADAMTS13) replacement therapy:
▪️ Demonstrated favorable efficacy and safety profile
▪️ Approved in the US, EU, and Japan for both prophylactic and on-demand use
▪️ Represents a paradigm shift in long-term cTTP management, reducing dependence on plasma infusions
This lecture clearly underscored that TTP treatment is entering a new era of mechanism-based and targeted therapy.
Integrating these advances into national practice remains crucial, particularly with regard to laboratory capacity, ADAMTS13 monitoring, and access to innovative therapeutics in our region.”