At the Global Cardio-Oncology Summit 2025, Dr.Susannah Stanway from the United Kingdom delivered a powerful address titled “Access to Oncology Care: A Global Perspective.” Opening with a reflection on Cape Town’s symbolic message of “solidarity, equality, and sustainability,” she connected these themes to the urgent global challenge of ensuring equitable access to cancer care.
Dr. Stanway reminded attendees that cardiovascular disease remains the leading cause of death worldwide, followed by cancer. Both shareoverlapping risk factors, biological pathways, and, importantly, health system solutions. This overlap underscores the importance of collaboration between oncology and cardiology communities to address the shared global burden of noncommunicable diseases (NCDs).
The rising global burden of cancer and CVD
Citing the Global Burden of Disease study published in The Lancet, Dr. Stanway noted that over 41 million deaths annually are caused by NCDs, accounting for 70% of all global mortality. While communicable disease deaths have declined due to major public health successes, the world now faces a steep rise in cancer and cardiovascular mortality, particularly in low- and middle-income countries (LMICs).
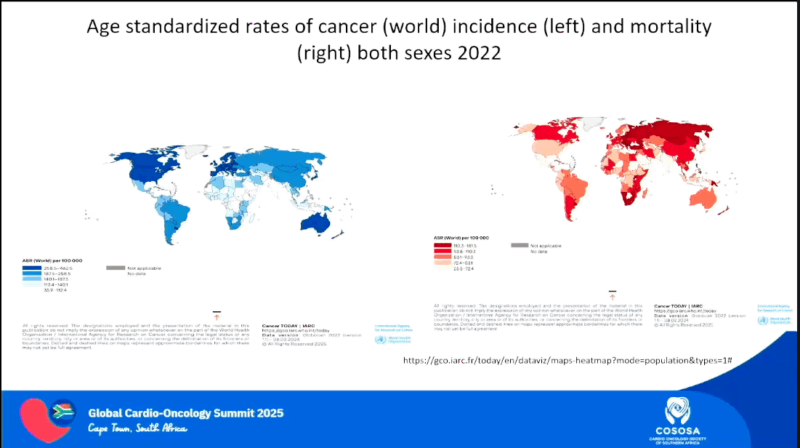
She emphasized that geography continues to dictate survival. Data from the International Agency for Research on Cancer (IARC) demonstrate a stark contrast between high incidence but lower mortality in high-income countries versus the reverse in LMICs, where limited access to diagnostics and treatment drives poor outcomes.
Global inequities and the call for system strengthening
Dr. Stanway referenced recent CONCORD and VENUSCANCER studies led by Claudia Allemaniand Michel Coleman, which revealed wide variations in survival for common cancers such as breast, cervical, and ovarian cancer across continents.In most high-income settings, where the data was collected, in-situ cervical tumours reached over 80%, while in lower-income regions this ranged between 3-55%. Access to oncology care such as targeted therapy, surgery, and radiotherapy remains profoundly unequal, further widening the survival divide.
For bridging the gap in global cancer care there are simple things:
- Strengthen the health system
- Consider economic constrain
- Adress social anc cultural factors
A recent analysis by Lisa Force and colleagues from the Global Burden of Disease Study Group (Washington, USA), published in The Lancet in 2023, examined cancer incidence and mortality across 204 countries between 1990 and 2023. The study reported 18.5 million new cancer cases and 10.4 million deaths in 2023 alone, with 65.8% of cancer deaths occurring in low- and middle-income countries. Importantly, 41.7% of all cancers were attributable to modifiable risk factors, underscoring the urgent need for stronger prevention strategies and policy interventions targeting lifestyle and environmental determinants of cancer.
Access to systemic therapies remains a central challenge in achieving equitable cancer care worldwide. As shown in recent data from the pharmaceutical industry’s global pipeline, most drug development activity has now shifted from cardiovascular disease to oncology—a reflection of the field’s rapid expansion. Yet the growing number of therapies does not necessarily translate into equitable access.
Two key developments illustrate this paradox. The first is the World Health Organization’s Essential Medicines List, which currently includes more than 500 drugs and was most recently updated in September 2025. While inclusion on the list does not guarantee affordability or availability in all countries, it provides crucial guidance to governments on which treatments should be prioritized for public health benefit.
The second is the emerging “Common Sense in Oncology” movement, led by Dr. Christopher Booth and Dr. Bishal Gyawali and others, which challenges the imbalance between innovation and accessibility. The movement highlights a troubling paradox: while some countries overutilize expensive, marginal-benefit drugs, large segments of the world’s population still lack access to essential therapies that can make a life-saving difference. Addressing this inequity, she emphasized, requires a global shift toward value-based, context-appropriate access to oncology care.
Radiotherapy is another cornerstone of treatment, contributing to nearly half of all cancer cures and required by over 50% of patients at some point during their disease course. Despite this, access remains highly uneven, with more than 200 million people living in countries with no radiotherapy facilities at all. To address this gap, alliances such as the Global Coalition for Radiotherapy and international efforts led by the International Atomic Energy Agency (IAEA) are driving initiatives to expand capacity.
A recent meeting in Addis Ababa, hosted by the African Union under the “Rays of Hope” initiative, exemplified growing international commitment to improving radiotherapy infrastructure. The personal attendance of IAEA Director General Rafael Grossiunderscored the agency’s leadership in promoting equitable access to radiation treatment.
To further raise awareness, the World Radiotherapy Awareness Day Message was launched this year—a global campaign encouraging collaboration and advocacy across the clinical oncology community. The initiative aims to mobilize oncologists, policymakers, and stakeholders toward actionable progress in radiation access and quality.
Equity in access to oncology care also extends beyond treatment to survivorship. It is estimated that 53 million people worldwide are currently within five years of a cancer diagnosis, with millions more living long-term after treatment. The psychosocial, physical, and spiritual needs of these individuals remain too often overlooked. Dr. Stanway underscored the need for context-specific survivorship programs, emphasizing that rehabilitation, palliative care, and health promotion must be integrated into comprehensive cancer control strategies.
Emerging research, including studies from Latin America, demonstrates that survivorship care tailored to regional realities can improve both quality of life and long-term outcomes. Conferences such as the Global Cardio-Oncology Summit, she noted, play a critical role in fostering this multidimensional approach—linking prevention, treatment, and survivorship through shared learning and collaboration.
Cancer intelligence and data-driven policy
Reliable data remain the cornerstone of effective cancer control. Dr. Stanway highlighted the work of the Global Initiative for Cancer Registry Development (GICR) led by IARC, which supports more than 80 countries in building robust national cancer registries. Yet many nations still lack functioning systems to collect incidence and survival data. Without accurate information, she noted, governments cannot design policies or allocate resources effectively.
Financing and the economics of cancer care
A significant portion of her talk focused on economic barriers. Drawing from the World Bank’s International Debt Report 2024, she noted that LMIC debt reached $8.8 trillion, with servicing costs burdening already fragile economies. The COVID-19 pandemic further strained budgets and exposed the vulnerability of health systems.
Citing the NCD Alliance report Better Data for Better NCD Financing (2024), Dr. Stanway emphasized that 100 million people are pushed into poverty each year due to out-of-pocket payments for NCD care. Between 2011 and 2030, the global economy is expected to lose $47 trillion from premature deaths and reduced productivity linked to chronic diseases. “Health must be reframed as an investment, not a cost,” she urged, calling for innovative financing models, improved data transparency, and engagement of finance ministers in global health discussions.
A comparative analysis from JAMA Health Forum (2022) showed that despite spending three times more on cancer care than Italy, the United States has similar mortality outcomes—illustrating that issues beyond spending volume, determine success.
Health as an ethical and economic imperative
Dr. Stanway underscored findings from the Cancer Epidemiology study examining the BRICS+ countries, which now represent nearly half the world’s population and one-third of global GDP. In 2012 alone, premature cancer-related mortality cost these economies $46 billion, equivalent to 0.33% of combined GDP. These data reinforce the notion that sustainable investment in prevention, screening, and early diagnosis not only saves lives but also strengthens economic productivity.
Political will and social determinants
Beyond economic reforms, political commitment is essential. Dr. Stanway advocated for universal health coverage (UHC) and stronger national cancer control plans. Around 150 countries now have such plans, but implementation varies widely. She called for taxation and regulation of commercial determinants—tobacco, alcohol, and unhealthy foods—to reduce preventable cancers.
She also highlighted social and cultural determinants, including health literacy and gender equity, citing studies such as Women, Power and Cancer and innovative grassroots initiatives in Zambia and India that bring mobile screening and education to rural populations.
“Top-down frameworks are vital, but real change starts in communities,” she said.
Climate change and cancer care
Dr. Stanway closed by connecting environmental and oncologic health through Oncology Advocates United for Climate and Health (OUCH International), an organization addressing how climate change and air pollution exacerbates cancer risk and healthcare inequities. As healthcare contributes significantly to global emissions, the oncology community has both a responsibility and opportunity to lead climate-smart healthcare initiatives.
Conclusion
The session underscored that achieving equity in cancer care is both an ethical duty and an economic necessity. True progress will depend on collective action – strengthening prevention, diagnosis, treatment, and survivorship worldwide. As highlighted in Cape Town, access to oncology care globally is an urgent need, and solidarity and sustainability must guide the future of global oncology.
For more information click here.