George J. Li, Chief Resident at the Department of Radiation Oncology, University of Toronto (UTDRO), shared a post on X:
“Excited to share our new systematic review looking at risks and outcomes of definitive radiotherapy for patients with comorbid ILD and early-stage NSCLC!
In our analysis of 24 studies including 705 patients with purely stage I-II NSCLC (no oligomets), we found the risk of radiation-related mortality was ~8% and severe respiratory toxicity was ~16%, lower than reported in prior reviews.
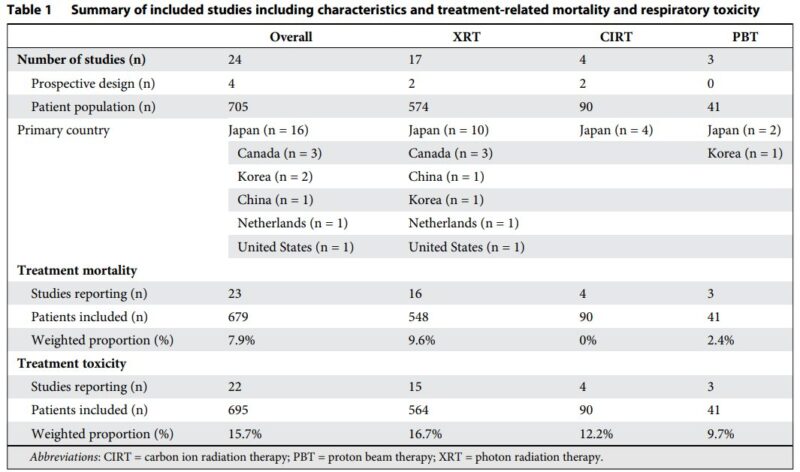
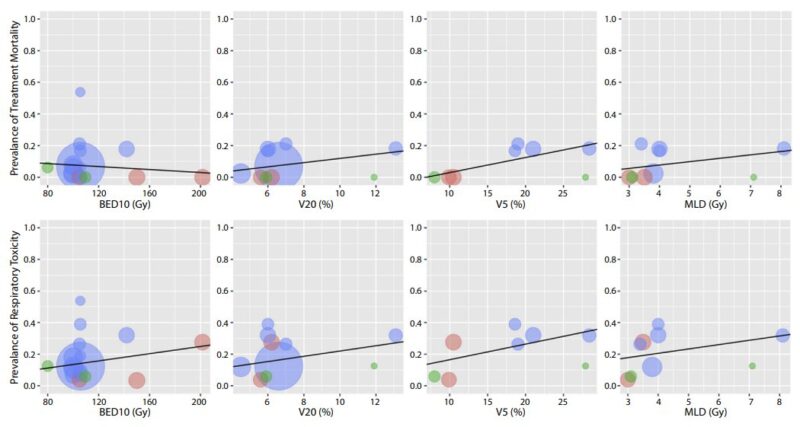
A key finding:
Higher volume of lung receiving low-dose radiation (V5) was significantly correlated with mortality.
IMRT (or protons?) may be preferrable over VMAT in this population to reduce low dose wash.
How well does radiotherapy work?
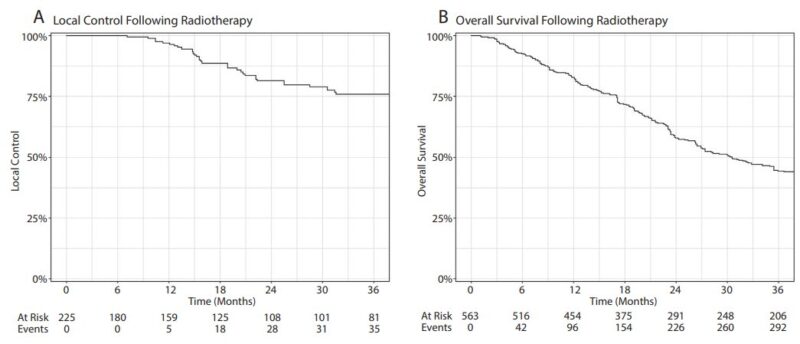
We found an aggregate 3-year local control rate of 76% and median OS of 2.5 years – the decision to treat must carefully balance this benefit against the risks of toxicity.
Multidisciplinary assessment is key!
We found a gap in Radiation Oncology literature, where ILD subtype/severity was not reported in 50% of studies.
Just as staging is critical in treating cancer, ‘staging’ ILD with a respirologist is equally important.
Our work builds on previous studies, like the 2017 systematic review by Dr. Hanbo Chen, which first quantified the high radiotherapy toxicity risks for ILD patients, while also providing a comparison to RFA and surgery.
For an overview of ILD in the context of thoracic radiation, this 2020 primer by Chris Goodman remains an essential read for thoracic oncologists.
Highlighting prospective data, the ASPIRE-ILD trial (included in our review) enrolled 39 patients with ES-NSCLC and ILD, treated with 50Gy/5fx SBRT, resulting in a 2-year LC of 92%, mOS of 25 months, and 7.7% grade 5 toxicity rate.
Next steps are to refine our approach to treatment and patient selection. The ongoing RESPIRE-ILD trial by Houda Bahig and David Palma is testing if medications like NAC and steroids can reduce dyspnea after RT, which could be practice-changing.
Returning back to our present systematic review, it again highlights a critical need for consistent reporting of ILD characteristics in future Radiation Oncology studies.
Better data will lead to better risk stratification and outcomes for our patients.”
Title: Treatment Toxicity and Outcomes Following Definitive Radiation Therapy for Patients With Early-Stage Non-Small Cell Lung Cancers and Pre-Existing Interstitial Lung Disease – A Systematic Review and Dosimetric Analysis
Journal: The International Journal of Radiation Oncology
Authors: George J. Li, Melissa Sam Soon, Hanbo Chen, Gabriel Boldt, Houda Bahig, Patrick Cheung, David A. Palma, Christopher J. Ryerson, Suresh Senan, Alexander V. Louie

Title: Treatment-Related Toxicity in Patients With Early-Stage Non-Small Cell Lung Cancer and Coexisting Interstitial Lung Disease: A Systematic Review
Journal: The International Journal of Radiation Oncology
Authors: Hanbo Chen, Suresh Senan, Esther J. Nossent, R. Gabriel Boldt, Andrew Warner, David A. Palma, Alexander V. Louie
Title: Primer on Interstitial Lung Disease and Thoracic Radiation
Journal: Journal of Thoracic Oncology
Authors: Christopher D. Goodman, Suzan F.M. Nijman, Suresh Senan, Esther J. Nossent, Christopher J. Ryerson, Inderdeep Dhaliwal, X. Melody Qu, Joanna Laba, George B. Rodrigues, David A. Palma
Title: Stereotactic Radiation Therapy in Early Non–Small Cell Lung Cancer and Interstitial Lung Disease: A Nonrandomized Clinical Trial
Journal: JAMA
Authors: David A. Palma, Houda Bahig, Andrew Hope, Stephen Harrow, Brock J. Debenham, Alexander V. Louie, Thi Trinh Thuc (Toni) Vu, Edith Filion, Andrea Bezjak, Marie-Pierre Campeau, Adele Duimering, Meredith E. Giuliani, Joanna M. Laba, Pencilla Lang, Benjamin H. Lok, X. Melody Qu, Srinivas Raman, George B. Rodrigues, Christopher D. Goodman, Stewart Gaede, Julie Morisset, Andrew Warner, Inderdeep Dhaliwal, Christopher J. Ryerson
More posts featuring radiotherapy on OncoDaily.