Qasim Hussaini, Medical Oncologist at the Sidney Kimmel Comprehensive Cancer Center of the Johns Hopkins Hospital, shared on X/Twitter:
“Proud to present our special multi-institution effort where we investigate barriers and provide solutions impacting oncology physician workforce diversity.
Led by Dr. Curtiland Deville with Kenechukwu Charles-Obi, Trisha Santos, and Malcolm Mattes.
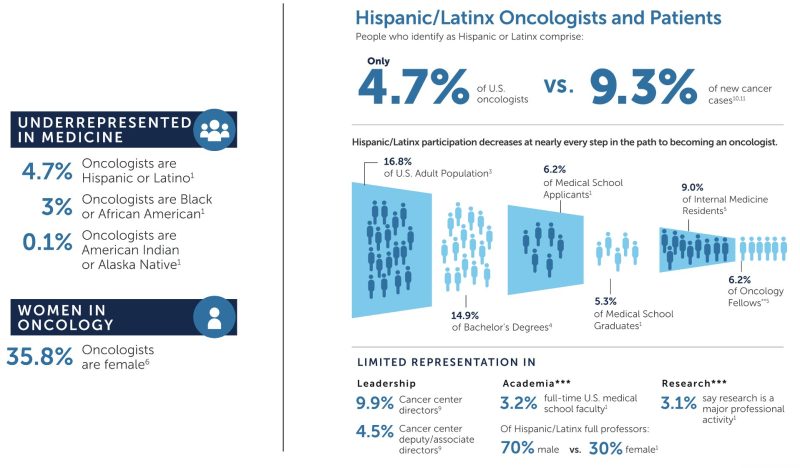
Here are some sobering numbers to begin this discussion: Per 2022
ASCO Snapshot
13.3k practicing oncologists in US
4.7% Hispanic/Latino
3% Black or African American
0.1% American Indian or Alaskan Native
There is attrition at each step along the way for UIM representation
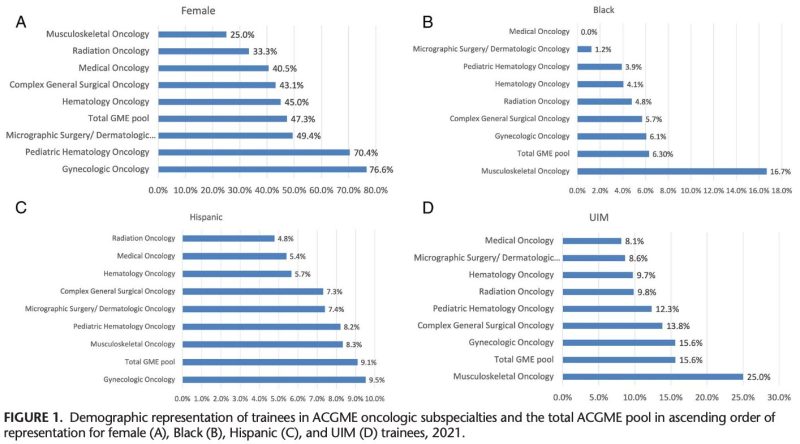
In our study, we noted stark inequities in the representation of women and racial and ethnic minority groups in the ACGME oncologic training specialties. Here are some numbers from 2021.
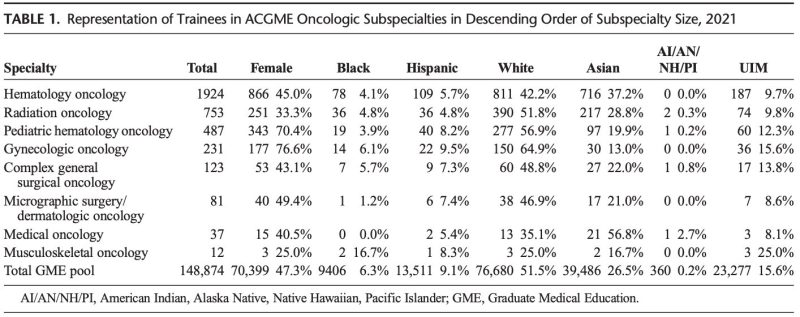
We show Black representation was highest in surgical oncology (5.7%), Hispanic representation highest in gyn onc (9.5%). Women representation was highest in gyn onc (76.6%), but otherwise hovered between 33-45% for rad onc, surg onc and heme onc.
We then studied temporal trends in trainee representation of the last 30 years among hematology-oncology, medical oncology, radiation oncology, and pediatric hematology oncology. For Black, Hispanic/Latino, UIM, and AIAN/NHPI, these numbers have remained static.
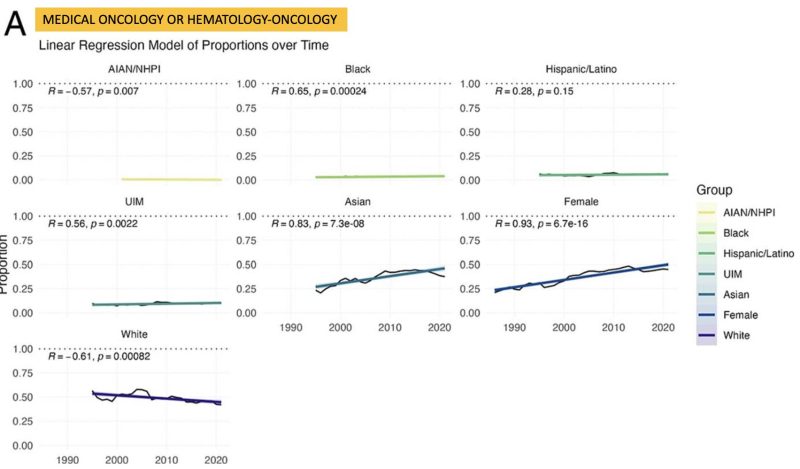
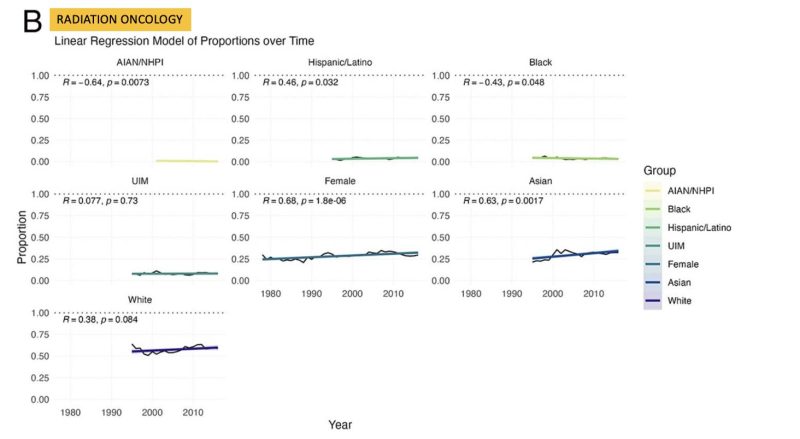
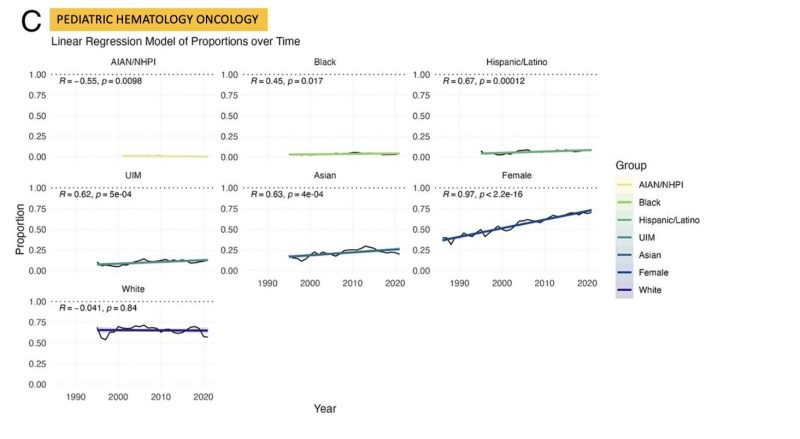
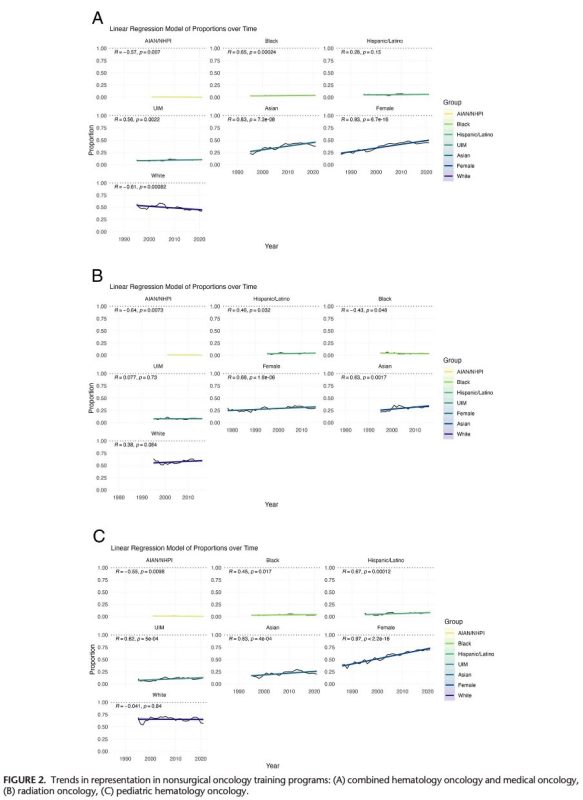
Of note, while female and Asian representation increased above, White representation remained static or decreased over time.
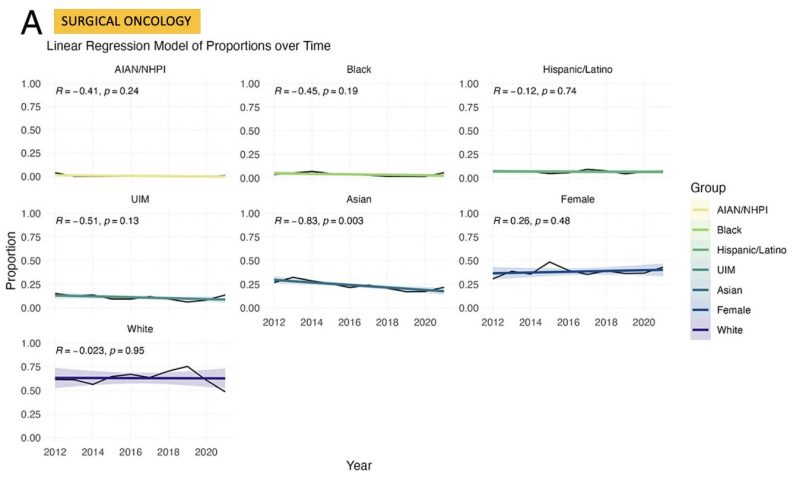
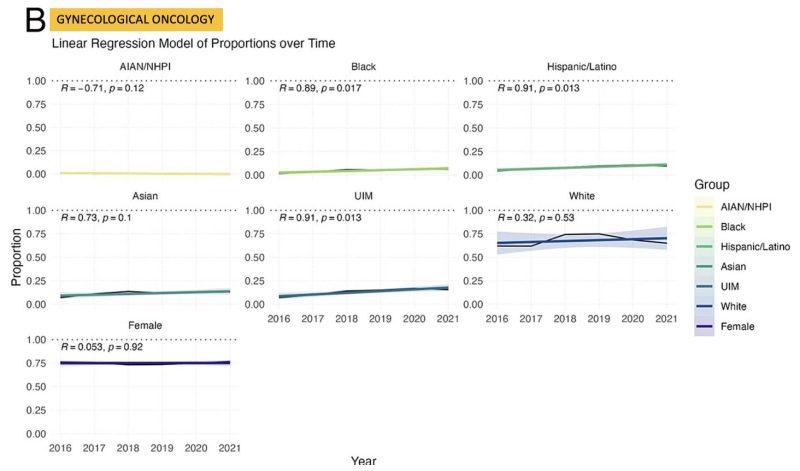
Below are some numbers for surgical onc & gyn onc with different findings. Female representation saw no change. Gyn onc did better with representation.
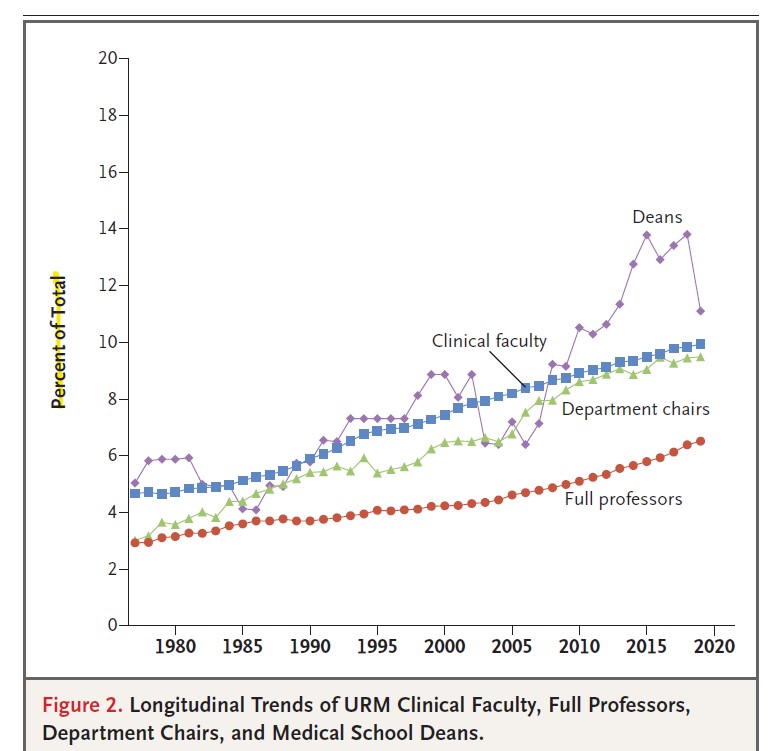
Further, we know few URM make it to academic onc faculty, and those that do are underrepresented at EVERY level. Beyond oncology, Drs Sophia Kamran, Karen Winkfield, Neha Vapiwala and Reede’s recent work noted a concerning widening URM gap over a 40yr analysis.
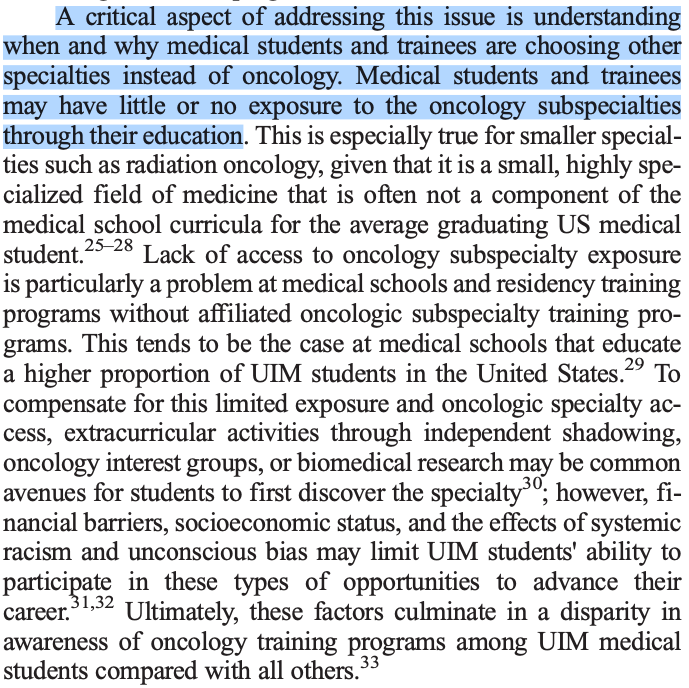
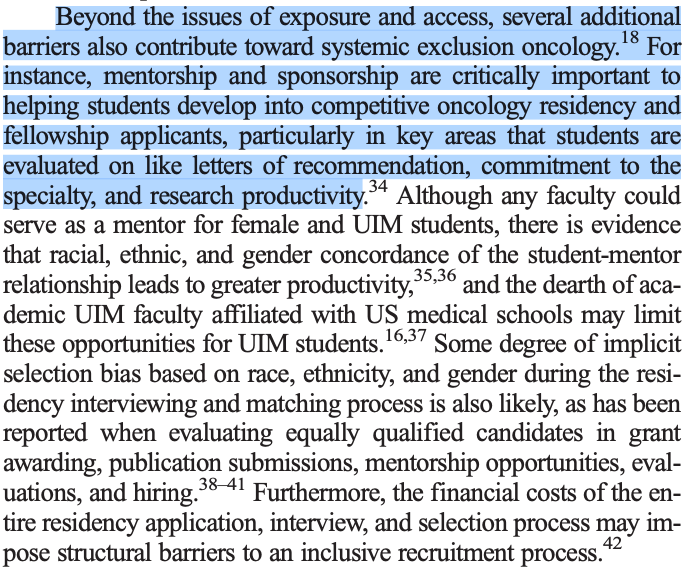
Barriers to choosing a career in oncology and completing oncologic training occur across the career trajectory from initial exposure and specialty access. A few expert thoughts from our piece below.
A systemic approach with structured leadership and administrative support will be necessary for individual departments, as well as national specialty societies, to overcome these multifaceted barriers to a diverse workforce in oncology. We present several examples in our article.
At the societal level, some key DEI initiatives from
ASCO:
Medical Student Rotation for URM
Annual Meeting Research Award for URM
Oncology Summer Internship
ASTRO:
Leadership Pipeline Program
Aspiring Scientist & Physician Program
Med Student Fellowship Program
Efforts, however, must also be undertaken by training programs to rise to the challenge. It begins with addressing the pipeline problem & investing in professional development. Read about the unique program we built at The Hopkins Hem Onc Fellowship.
Ultimately, there is real world impact of missing the mark on improving oncologic physician diversity. See this recent work led by Vishal Patel where we noted high levels of delayed or foregone care by patients due to patient-clinician identity differences.
Ultimately, tailored approaches are needed to address the largest demographic gaps per oncologic subspecialty to ensure our workforce is representative of the increasingly diverse patient population it serves and that health disparities and inequities are effectively addressed.”
For the article click here.
Source: Qasim Hussaini/Twitter


