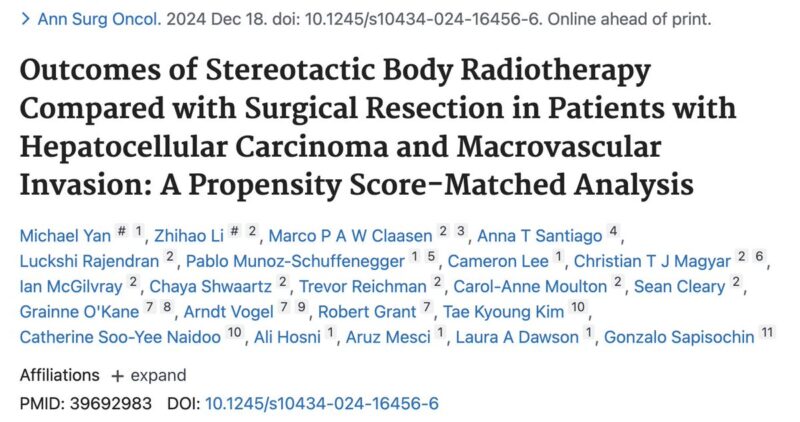
Jeffrey Ryckman, Radiation Oncologist and Assistant Professor at West Virginia University, shared a post on X:
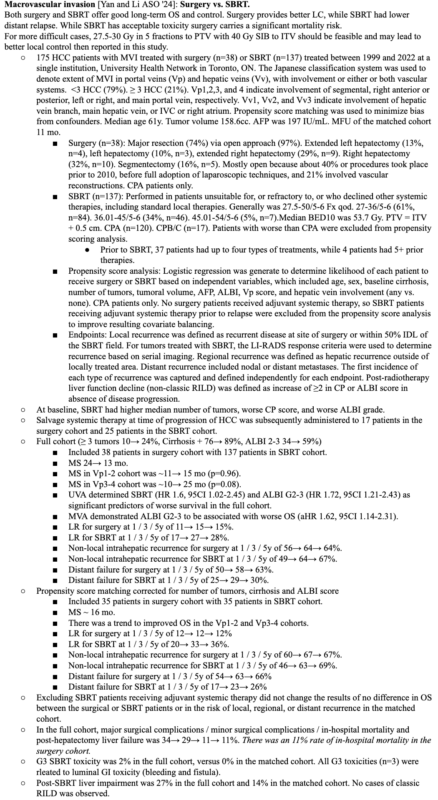
“Treating hepatocellular carcinoma (HCC) with macrovascular invasion (MVI) has always been challenging. New research compares two approaches—surgery and stereotactic body radiotherapy (SBRT)—providing fresh perspectives on how we care for these patients.
Let’s dive in.
This study used propensity score matching to ensure fair comparisons between the two groups. The primary outcome was overall survival (OS), with secondary outcomes including local control and distant recurrence rates.
Here’s what they found:
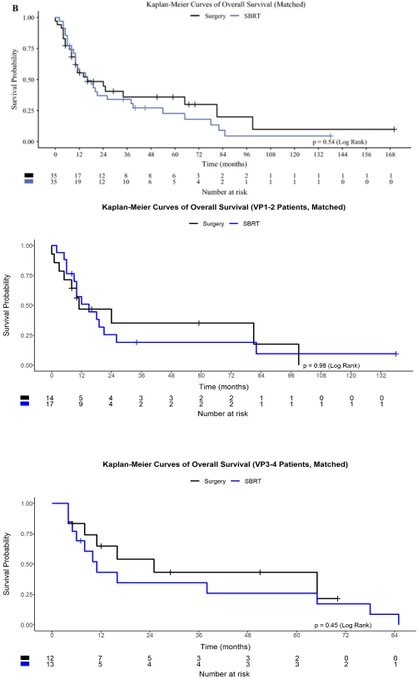
OS was comparable in both groups, with a median of ~16 months. But each approach has distinct advantages:
Surgery: Stronger local control (failure rate: 12% vs. 20% with SBRT).
SBRT: Fewer distant failures (17% vs. 54% with surgery).
Why the difference?
Surgery directly removes visible disease but might inadvertently contribute to distant spread by disrupting the environment.
SBRT precisely targets tumors, sparing surrounding tissue and possibly enhancing immune system activity.
Let’s talk safety:
Surgery carried a 9% in-hospital mortality rate and significant complications.
SBRT was less invasive, with minimal severe toxicity but a 14% chance of post-treatment liver function decline.
These factors are crucial when choosing a treatment plan.
Interestingly, the findings echo Bernard Fisher’s theory that surgical interventions might temporarily suppress the immune system, potentially leading to distant failures. Meanwhile, SBRT’s immune-modulating effects could offer a protective benefit.
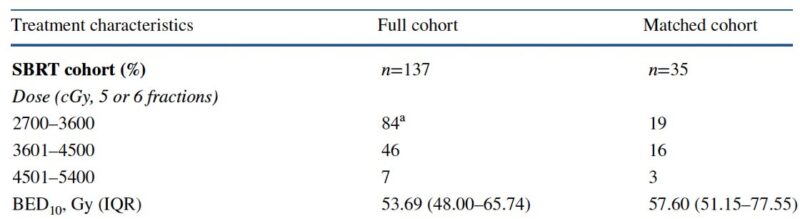
And what about progress in radiotherapy?
In this study, the median biologically effective dose (BED10) for SBRT was 53.7 Gy. With modern techniques (e.g., 27.5 to PTV, 40+ to ITV), doses could bring local failure rates well below 20%. Exciting potential for the future!
The takeaway?
Both SBRT and surgery are valuable tools:
Surgery excels in controlling disease at its source.
SBRT is less invasive and may reduce the risk of distant recurrence.
Each patient’s needs and priorities will guide the best choice.
What’s next? Combined strategies could further improve outcomes.
Trials integrating SBRT with systemic therapies or using SBRT as a bridge to surgery show promising early results. A new chapter in care for HCC with MVI may be on the horizon.
TL;DR: Surgery and SBRT both offer meaningful options for advanced HCC with MVI, each with unique strengths.
Personalizing treatment through multidisciplinary discussions is key to supporting patients in their journey.”