Linvoseltamab-gcpt is a newly approved cancer treatment for adults with relapsed or refractory multiple myeloma. This innovative drug was approved by the FDA in July 2025 and offers hope for patients who have already tried multiple other therapies without success. It represents an exciting advancement in targeted immunotherapy for difficult-to-treat blood cancers.
Lynozyfic was developed by Regeneron Pharmaceuticals, Inc., a U.S.-based biotechnology company known for pioneering work in immunotherapy and genetic research. Regeneron is also the developer of several other successful biologic treatments and continues to invest heavily in cancer research.
What Is Linvoseltamab and How Does It Work?
Linvoseltamab is a bispecific antibody, meaning it is designed to connect two different types of cells. It targets a protein called BCMA found on multiple myeloma cells and CD3 on T cells, a key part of the immune system. By binding to both, linvoseltamab brings T cells into direct contact with cancer cells. This triggers the immune system to attack and destroy the cancer, even when the cancer has become resistant to earlier treatments. This approach allows the immune system to refocus its efforts on eliminating myeloma cells in a precise and controlled way.
What Cancers Does Linvoseltamab Treat?
Linvoseltamab is approved for the treatment of relapsed or refractory multiple myeloma in adults who have previously received at least four different types of treatment. These include a proteasome inhibitor, an immunomodulatory drug, and an anti-CD38 antibody. It specifically targets the BCMA protein, which is commonly found on malignant plasma cells in multiple myeloma.
You can read more about Multiple Myeloma: Symptoms, Causes, Stages, Diagnosis and Treatment on OncoDaily.
Efficacy and Results from Clinical Trials
The approval of Linvoseltamab was based on promising results from the phase 1/2 LINKER-MM1 trial. This study included patients with heavily pretreated multiple myeloma who had not received BCMA-targeted therapy before. Among those treated with the 200 mg dose, 71% responded to the drug, and 50% achieved a complete response or better. Impressively, 72% of responders maintained their benefit at 12 months, and the median duration of response reached 29.4 months.
A lower 50 mg dose was also tested in 104 patients, with a 48% response rate and 21% achieving a complete response. These findings, published in the Journal of Clinical Oncology in June 2024, supported the 200 mg dose as the optimal choice for long-term effectiveness.
What Is a Clinical Trial and Why Does It Matter?
A clinical trial is a research study designed to test new drugs and treatments in patients to determine their safety and effectiveness. Before Linvoseltamab was approved, it went through multiple phases of clinical trials to assess how well it worked, what side effects it caused, and whether it was better than existing treatments. Clinical trials are essential because they provide scientific evidence that a drug can help patients while ensuring it is safe for widespread use.
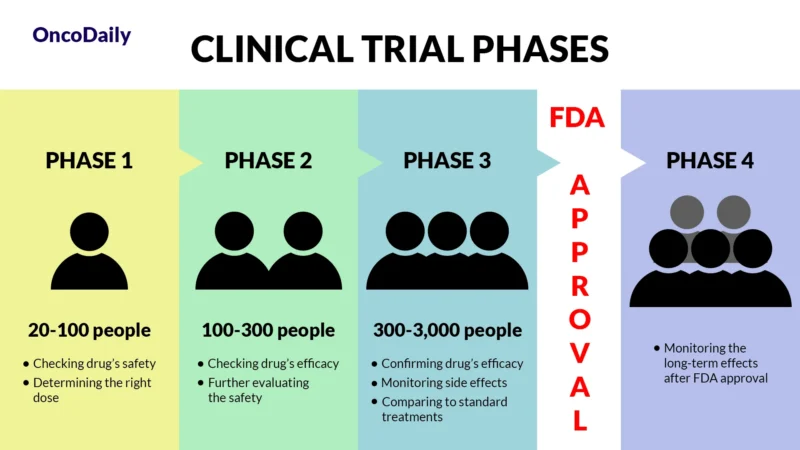
What Does FDA Approval Mean?
When a drug receives FDA approval, it means that after rigorous testing in clinical trials, it has been shown to be both safe and effective for treating a specific condition. The FDA granted accelerated approval to Linvoseltamab based on the LINKER-MM1 trial’s strong early results. This approval makes the drug widely available for doctors to prescribe and helps patients access new, cutting-edge treatments sooner.
Side Effects and Management
Linvoseltamab is a type of immunotherapy designed to help the immune system fight multiple myeloma. While it can be very effective, it may also cause side effects. Some are mild and go away on their own, while others are more serious and need medical attention. Knowing what to expect can help patients feel more prepared and safer during treatment.
Common Side Effects
Some side effects are more common, especially early in treatment. One of the main ones is called cytokine release syndrome (CRS), which is the body’s strong immune reaction to the drug. CRS can cause fever, chills, tiredness, low blood pressure, or difficulty breathing. These symptoms usually happen soon after receiving the medicine and often go away with supportive care. Another common reaction is called an infusion-related reaction, which might include feeling dizzy, getting a rash, or feeling sick to your stomach during or after the infusion.
Linvoseltamab can also affect your blood cells. You might have fewer white blood cells, which help fight infections, or fewer red blood cells, which can make you feel tired. A low platelet count can lead to easy bruising or bleeding. Some people also report body aches, headaches, cough, diarrhea, or infections like colds or pneumonia.
Less Common but Serious Side Effects
In some cases, more serious side effects may occur. One rare issue is called ICANS, a condition that affects the brain and nervous system. This may cause confusion, trouble speaking, or even seizures. It usually happens early in treatment and needs immediate care. Severe infections can also happen, especially when white blood cells are low. These infections might be caused by bacteria, viruses, or fungi and can become dangerous if not treated right away.
Some people may also have problems with their liver, which are usually seen in blood tests as increased liver enzyme levels. A very rare but serious immune reaction called HLH-like syndrome can cause extreme inflammation and needs emergency care.
How Side Effects Are Managed?
Before each dose, patients receive medications such as corticosteroids, antihistamines, and fever reducers to help prevent CRS or infusion reactions. If a serious reaction occurs, the infusion may be paused and restarted at a slower rate. CRS can be treated with medications like tocilizumab, and ICANS usually responds to corticosteroids. Blood count problems are managed with temporary dose interruptions or medications that boost blood cell production. Preventive antibiotics and regular monitoring help reduce infection risks. Liver problems are monitored through regular blood tests and may require dose adjustments.
Recommended Dosage of Linvoseltamab
Linvoseltamab comes in two strengths: a 5 mg vial and a 200 mg vial. Treatment starts with smaller “step-up” doses to help your body adjust and reduce the risk of side effects. You’ll receive 5 mg on Day 1, 25 mg on Day 8, and the full dose of 200 mg on Day 15. After this, 200 mg is given once a week for 10 weeks. If your cancer responds well and you’re doing okay, the schedule may shift to every two weeks, and later every four weeks starting after Week 24. This flexible approach helps balance effectiveness and safety.
How Is Linvoseltamab Given?
Linvoseltamab is given as an intravenous (IV) infusion, meaning the medication is slowly delivered into your bloodstream through a vein, usually in your arm. The medicine is prepared by mixing it with a sterile saline solution and checked carefully for clarity and safety before use.
The first few infusions are longer. For example, the initial step-up doses (5 mg, 25 mg, and the first 200 mg dose) are usually given over about four hours to monitor for any early reactions. After that, the second 200 mg dose is typically infused over one hour, and later doses take about 30 minutes—unless your doctor needs to slow the infusion to manage side effects.
How is Lynozyfic processed and removed from the body?
After it’s given, Linvoseltamab is slowly broken down by the body into smaller, natural protein pieces. It stays in the body for a long time, which helps it keep working over time. Even after the last dose, most of the drug takes about 11 weeks (77 days) to clear from the bloodstream. This slow removal supports the extended dosing schedule used during treatment.
What to Avoid During Treatment?
While on linvoseltamab, patients should avoid live vaccines, alcohol, herbal supplements, and any medications not approved by their healthcare provider. Since the drug can weaken the immune system, it’s important to avoid crowds and limit exposure to infections. Patients should also avoid skipping or delaying doses, and all infusions must be done under medical supervision.
Real-Life Effectiveness and Future Outlook
Early real-world results suggest that linvoseltamab is effective and well-tolerated when given as part of clinical practice. New data from the phase 1b LINKER-MM2 trial show that combining linvoseltamab with bortezomib, another myeloma drug, leads to even better outcomes. In that trial, 79% of patients responded, and 90% of them maintained their response for at least six months. These results suggest linvoseltamab could be used earlier in treatment or in combination with other therapies in the future.
Ongoing Trials and Future Potential
Research is continuing in other diseases, including systemic light chain (AL) amyloidosis. In the LINKER-AL2 trial (NCT06292780), linvoseltamab is being tested in people with relapsed or refractory AL amyloidosis. The study is exploring how well the drug reduces harmful proteins that affect the heart and kidneys and whether these improvements last over time.
Linvoseltamab represents a new approach in the treatment of relapsed or refractory multiple myeloma. By engaging the immune system in a highly targeted way, it offers new hope for patients who have exhausted other treatments. With strong results from clinical trials and more research underway, this drug may play an even bigger role in the future of cancer therapy.
If you’re a healthcare provider, access the professional version here.