World Ovarian Cancer Coalition shared a LinkedIn post about recent article published on Journal of Cancer Policy:
“The June issue of the Journal of Cancer Policy features our latest study:
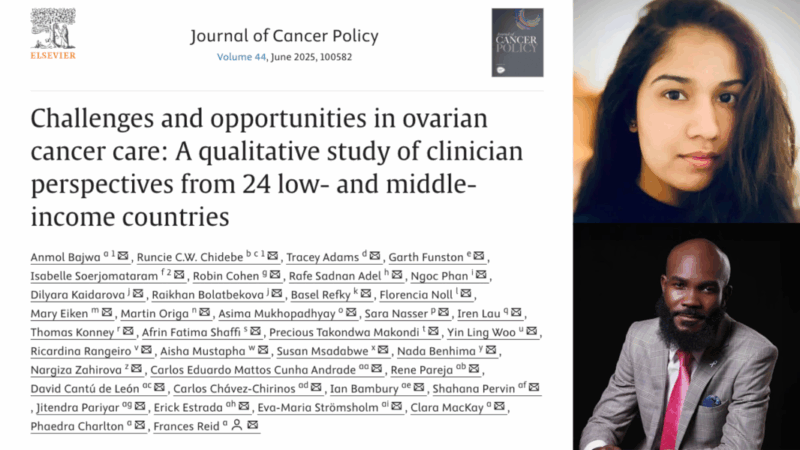
‘Challenges and opportunities in ovarian cancer care: A qualitative study of clinician perspectives from 24 low- and middle-income countries.’
To learn more, read our blog post, where the Coalition’s CEO, Clara MacKay, chats with co-lead authors Anmol Bajwa and Runcie C.W. Chidebe. Together, they dive deeper into the key themes of the report and considerations for improving access to diagnostics and therapies.
Clinician insights on the opportunities and challenges in ovarian cancer in LMIC
The June issue of the Journal of Cancer Policy includes the recent qualitative study with clinicians conducted as part of the multi-country observational Every Woman Study (EWS). Semi-structured interviews were conducted with clinicians between June 2022 and June 2023. The interview guide was developed by the EWS LMIC Oversight Committee, including patients, clinicians and data specialists. 24 clinicians participated representing Africa, Asia and Latin America.
This study reveals the complexity of ovarian cancer treatment and care in LMICs and the need to mitigate disparities in these regions, underscoring the need for patient-centred, context specific and intersectoral strategies to be considered in cancer planning to improve ovarian cancer care quality and equity in LMICs.
The study, titled, Challenges and opportunities in ovarian cancer care: A qualitative study of clinician perspectives from 24 low- and middle-income countries, can be found here.
The Coalition’s CEO, Clara MacKay, sat down with co-lead authors, Anmol Bajwa and Runcie C.W. Chidebe to dive deeper into the key themes of the report and considerations for improving access to diagnostics and therapies.
Clara: You spoke to clinicians from 24 countries, each with unique health systems and cultural contexts. Was there a common thread you noticed across these very different settings?
Anmol: Even though each country has its own health system, cultural backdrop, and set of challenges, a common thread that ran through almost every conversation was that women were often reaching care too late. The reasons why were far more complex than they appeared on the surface.
Whether in low-, lower-middle-, or upper-middle-income countries, clinicians described how financial barriers, gaps in infrastructure, cultural beliefs, and fear of treatment side effects all intertwined to impact diagnosis and care. It made me realize that, while the nature and weight of the barriers varied from country to country, the experience of facing layers of obstacles was something women shared almost everywhere.
What also stood out was how personal these barriers were. These weren’t just about access to a hospital, but about trust, about healthcare autonomy, about hope. It challenged me to think differently about how we talk about “access” in global health – not as a single issue to solve, but as a journey full of moments where support or failure can profoundly shape outcomes.
Clara: What conversations or moments during the interviews with these clinicians have stayed with you the most – and why?
Anmol: There are so many moments that have stayed with me, but one in particular continues to echo in my mind. A clinician from a lower-middle-income country shared how women often arrived at the hospital only when their disease had advanced to the point where the pain was unbearable.
I remember the clinician pausing for a moment before saying, almost quietly, “It’s not that they don’t want treatment. It’s that the road to treatment is filled with barriers we don’t always see.”
That moment stayed with me because it captured something so important – that the obstacles women face aren’t always visible from the outside. Additionally, there was also a deep and painful honesty in how clinicians spoke about the limitations they faced. It wasn’t just frustration about not having enough resources. It was a real sense of responsibility, and sometimes heartbreak, knowing exactly what their patients needed but being unable to provide it.
However, despite the barriers faced by the women with ovarian cancer as well as clinicians, what stood out most was a sense of resilience and hope that has stayed with me and continues to shape how I think about health systems.
Clara: How did hearing these stories from clinicians – often on the frontlines – change how you see the barriers women face when seeking ovarian cancer care?
Anmol: Hearing directly from clinicians on the frontlines was incredibly eye-opening. When I conducted these interviews, I was a Master’s student in Health Policy, and I came into the work expecting to hear primarily about resource shortages. But speaking with clinicians made me realize how much deeper and more layered the barriers really are.
It’s not just about infrastructure or funding. It’s about women living hours away from the nearest specialist, needing permission to travel, or placing their trust first in traditional healers because that’s what feels familiar. Fear, stigma, and financial strain quietly shape every step of the journey to care. These barriers are structural, cultural, and emotional.
They also do not exist in isolation; they stack up, making it harder and harder for women to reach care in time. As a health policy student, I had often thought about barriers in terms of infrastructure or financing, words we often use because they fit neatly into policy frameworks. But these conversations made it clear that for the women seeking care, and for the clinicians trying to care for them, health systems aren’t abstract. They are lived experiences.
Clara: There’s a lot of talk about ‘health systems strengthening’ – but this study puts real, personal stories behind that concept. How can this kind of qualitative research help move policy forward?
Runcie: As a patient advocate for better cancer care across Africa, every day I see how systems fail patients, their family caregivers, and professional care teams, not just because of a lack of resources, but because policies are often disconnected from the frontline reality. We must stop blaming the patients for every poor outcome and start blaming the health system that provided poor cancer services to the patients.
Health systems have a greater role to play in mitigating the burden of ovarian cancer in almost every setting. This study not only explored the challenges but also described possible sustainable solutions in line with the World Health Organization’s (WHO) building blocks of health systems. The opportunities identified in this study may be valuable for many low- and middle-income countries (LMICs).
We hope that policymakers can use the evidence from this study to inform their decisions on what is more useful and needed for clinicians to improve ovarian care in their countries, rather than assuming what is necessary.
Clara: How do you think this study could shift the global conversation about equity in cancer care -and what role can advocates play in keeping these voices at the centre of it?
Runcie: This research shows that equity isn’t just about funding – it’s about recognizing the need for more global collaboration and partnership for ovarian cancer among organizations such as the World Health Organization, the Union for International Cancer Control (UICC), the International Gynecologic Cancer Society, and the World Ovarian Cancer Coalition.
These global oncology communities have undertaken remarkable work in global campaigns and national policy engagement, utilizing the Global Strategy for Cervical Cancer Elimination and the Global Breast Cancer Initiative. This study explores the need to rethink and consider integration into existing strategies or developing new initiatives. On the other hand, patient advocates can use the results of this study to advocate for policy changes that improve ovarian cancer care in their respective countries.
For instance, (i.) advocate for a budget line to pilot access to targeted therapies in a public facility, (ii.) advocate for engagement of more men in ovarian cancer control, (iii.) use the examples of countries with success stories to convince policymakers, (iv.) advocate for quicker payment for cancer medicines by hospitals and many others as published in the study.
Clara: You have a particular interest in the important role of patient, family, and community engagement in driving improvements- what does this research tell us about that?
Runcie: The research reminds us that cancer care doesn’t happen in isolation – it’s deeply embedded in families and communities.
Clinicians often step far beyond their roles to provide emotional, social, and even financial support. That suggests that improving outcomes is partly about trust and engagement with community connections. As a patient advocate, I believe we must invest in the cancer health system if we want to see better outcomes for people with cancer. None of us is immune to cancer; hence, protecting and supporting women with ovarian cancer may be that opportunity to protect and support ourselves or those related to us in the future.”
Title: Challenges and opportunities in ovarian cancer care: A qualitative study of clinician perspectives from 24 low- and middle-income countries
Journal: Journal of Cancer Policy
Authors: Anmol Bajwa, Runcie C.W. Chidebe, Tracey Adams, Garth Funston, Isabelle Soerjomataram, Robin Cohen, Rafe Sadnan Adel, Ngoc Phan, Dilyara Kaidarova, Raikhan Bolatbekova, Basel Refky, Florencia Noll, Mary Eiken, Martin Origa, Asima Mukhopadhyay, Sara Nasser, Iren Lau, Thomas Konney, Afrin Fatima Shaffi, Precious Takondwa Makondi, Yin Ling Woo, Ricardina Rangeiro, Aisha Mustapha, Susan Msadabwe, Nada Benhima, Nargiza Zahirova, Carlos Eduardo Mattos Cunha Andrade, Rene Pareja, David Cantú de León, Carlos Chávez-Chirinos, Ian Bambury, Shahana Pervin, Jitendra Pariyar, Erick Estrada, Eva-Maria Strömsholm, Clara MacKay, Phaedra Charlton, Frances Reid

The study highlights insights from 24 clinicians across Africa, Asia, and Latin America as part of the Every Woman Study. It identifies key barriers such as late presentation, financial hardship, cultural stigma, and limited infrastructure, emphasizing the importance of patient-centered and context-specific strategies.
Read more articles about Ovarian Cancer on OncoDaily:
Bianca Balti: The Supermodel’s Brave Battle with Ovarian Cancer
Ovarian Cancer: Symptoms, Causes, Stages, Diagnosis and Treatment


