Olubukola Ayodele, Consultant Medical Oncologist at the University Hospitals of Leicester NHS Trust, shared a post on LinkedIn:
“It’s Day 1 of ASCO 2025 and the session on financial toxicity has left me deeply reflective.
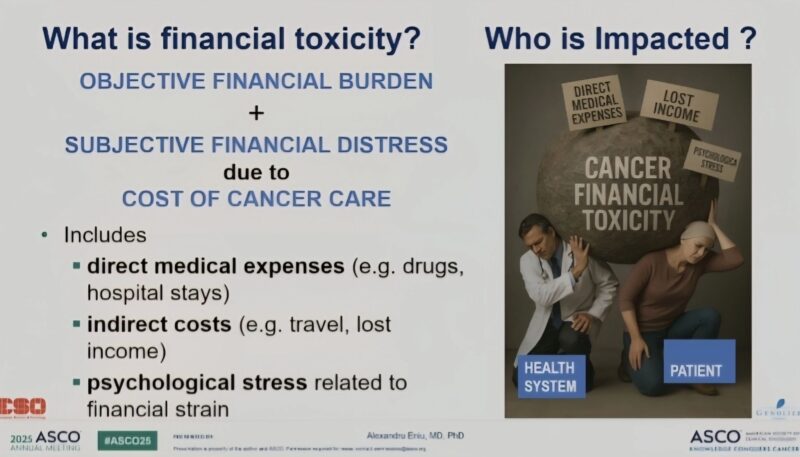
As oncologists, we frequently discuss side effects like fatigue, nausea, alopecia, and neutropenia. However, we talk far less about the invisible burden that gradually erodes dignity and security: Financial Toxicity (FT).
Coined in 2013, FT refers to the negative financial and psychological impact of cancer-related expenses. I’ve witnessed its toll in every health system I’ve worked in, which manifests in various ways:
– Loss of income due to time off work
– Cost of travel for treatment
– Paying for childcare during appointments
– Out-of-pocket costs for wigs, bras, and prescriptions
– Parking fees at hospitals—yes, patients still have to pay to park while fighting for their lives.
The emotional toll can also be significant, leading to guilt, anxiety, treatment delays, and even non-adherence.
Breast cancer patients are especially vulnerable due to:
– Higher caregiver burdens
– Lower average income
– Multimodal, prolonged treatments
– Often experiencing abandonment or divorce after their diagnosis
Recently, one of my patients returned to work mid-treatment, not because she was ready but because she couldn’t afford to miss rent. Patients are forced to choose between health vs survival, treatment vs food, life vs living.
In Europe, the UK has the second-lowest paid sick leave period. Our systems need urgent reform.
I must also raise an uncomfortable question: Are we, as healthcare professionals, contributing to financial toxicity?
– When we ignore costs of supportive meds
– When we prescribe beyond third-line treatments without questioning their real-world value
– When we fail to ask, “Can this patient afford this choice?”
Doctors are trained to heal, not to discuss finances.
I regularly refer patients with brain metastases for stereotactic radiosurgery (SRS) in Sheffield. However, we need to consider the additional costs for the patients and their caregivers (accommodation, meals, transportation, and logistics) that they wouldn’t incur if they were local to Leicester. We risk adding unseen burdens to already heavy shoulders.
I’ve had patients unable to pick up their medications due to work commitments or because they couldn’t afford transportation.
What can we do?
– Start the conversation: “Is cost a concern for you?”
– Eliminate avoidable costs: No one should pay for parking during cancer treatment.
– Arrange for pharmacies to deliver medications when possible.
– Evaluate treatments beyond third line for meaningful benefits.
– Provide financial navigators to help patients access support.
– Advocate for affordable and accessible treatments.
– Push for systemic change.
– Incorporate economic burden into the medical curriculum.
We must be proactive, not reactive. A cancer diagnosis should never lead to financial ruin.”
More posts featuring ASCO25.