30 Posts Not To Miss From ASCO GI24
The ASCO Gastrointestinal Cancer Symposium (GI24) took place from the 18th to the 20th of January in San Francisco, California. Our team at OncoDaily has handpicked 30 posts ASCO GI24 that you shouldn’t miss.
Syed A. Ahmad (USA)
Sobering lecture from Kimmie Ng highlighting the alarming increasing incidence of young GI cancers. Including CRC, pancreas and hepatobiliary.

Joseph McCollom (USA)
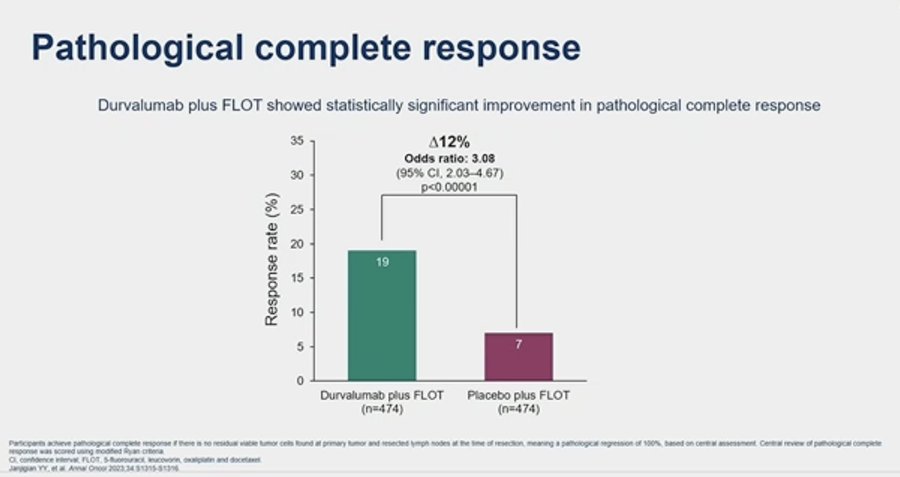
Yelena Janjigian presents the pathological complete response (pCR) 12% improved delta from the MATTERHORN trial with the addition of durvalumab to perioperative FLOT.
Rachna Shroff (USA)
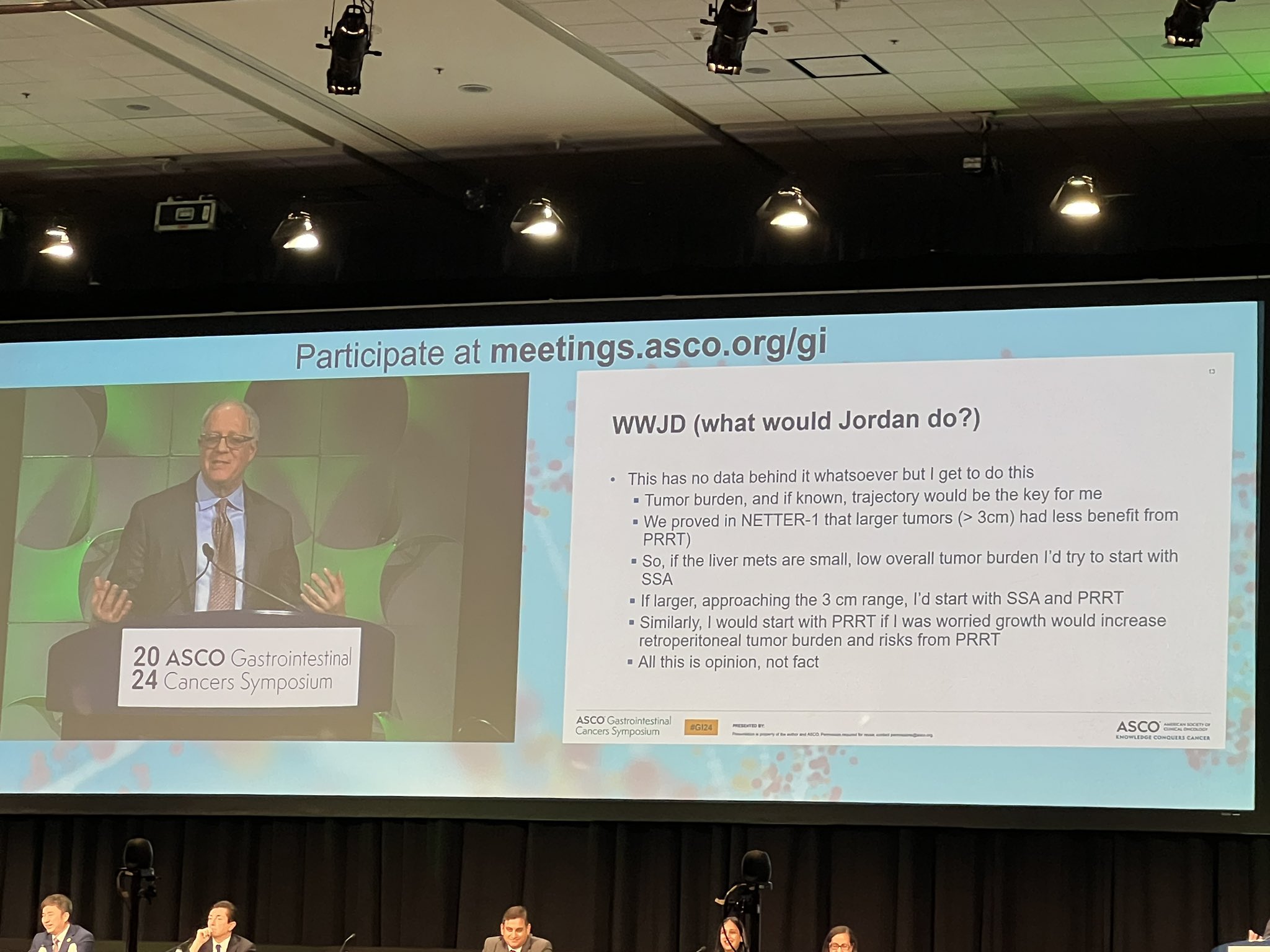
NETTER-2 and KRAS – is it the end game for NET and PDAC?! The inimitable Jordan Berlingives a masterclass discussion!
Mark Lewis (USA)
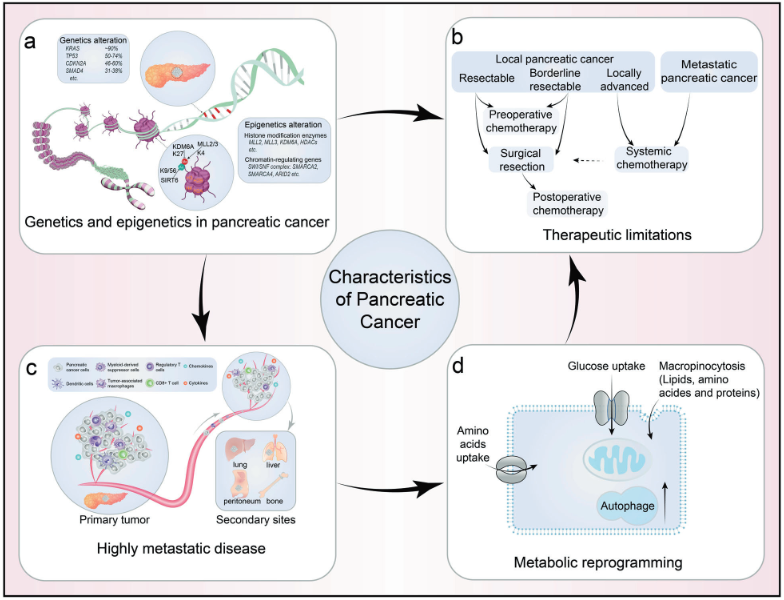
Why is pancreatic adenocarcinoma such a difficult cancer in which to make meaningful progress?
- Until recently KRAS mutations were considered undruggable
- A microenvironment inhospitable to immunotherapy
- Location, location, location
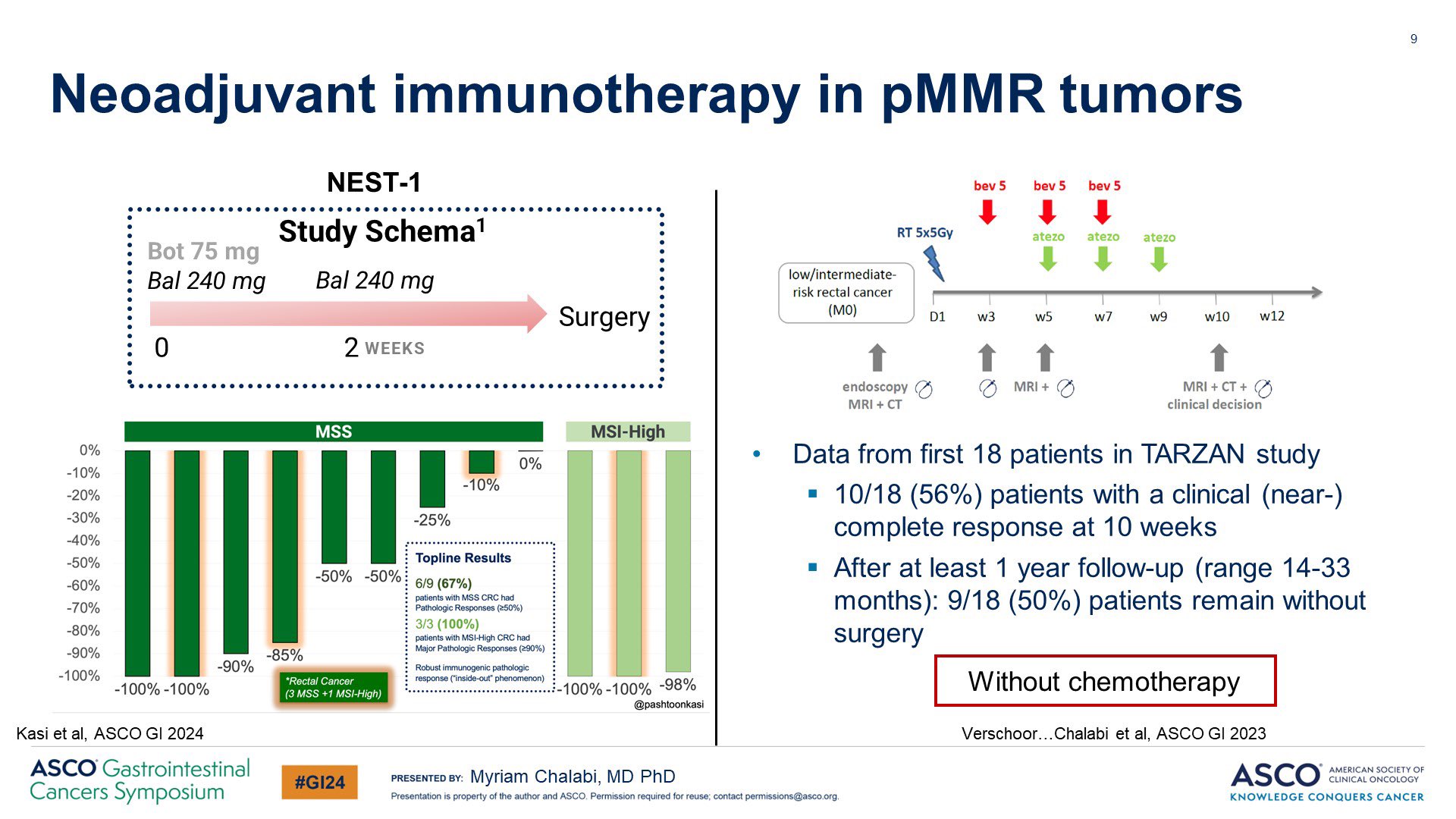
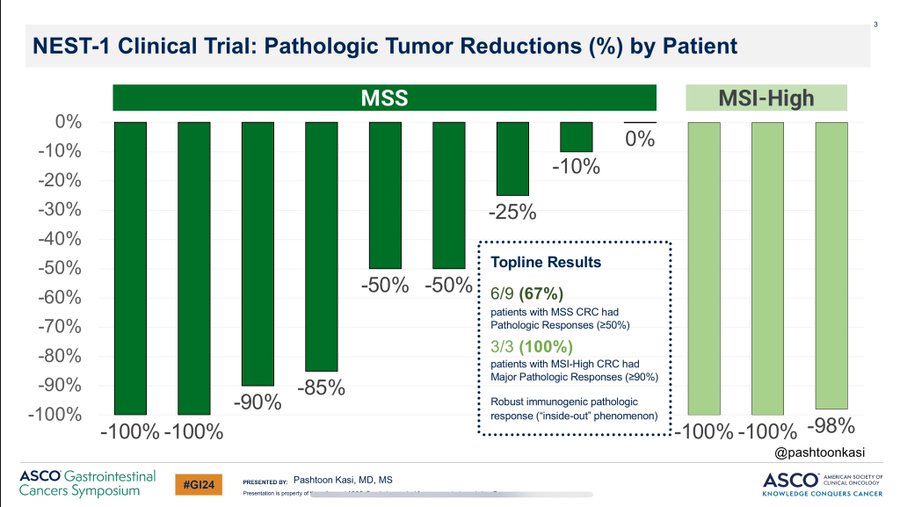
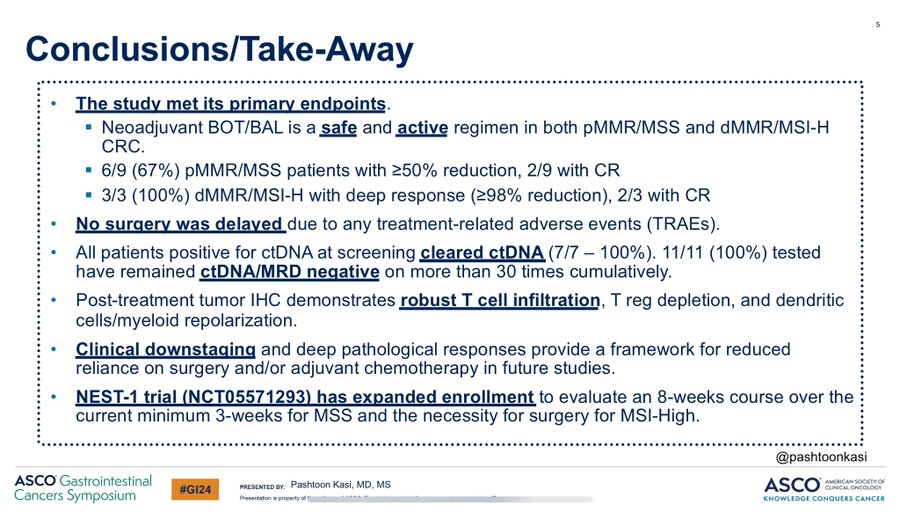
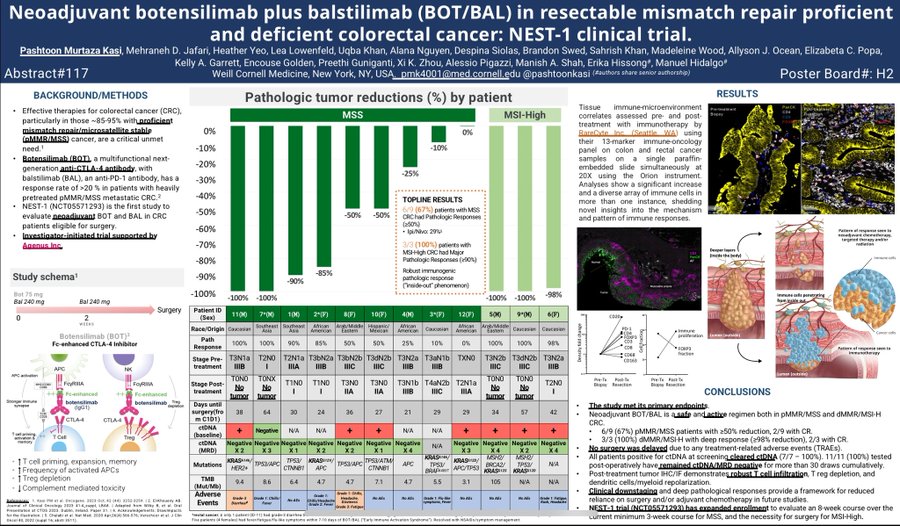
Pashtoon Kasi (USA)
Our NEST-1 study highlighted by Myriam Chalabi. 4 of our 12 patients treated on the clinical trial had rectal cancers as highlighted. Similar downstaging as in colon. Place for interrogating this more.
MSS:
- 100%
- 85%
- 10%
MSI-High
- 100%
Bishal Gyawali (Canada)
We had a fantastic session today morning at GI24 on the art and science of clinical trial design. Thank you ASCO and session chairs Nina Niu Sanford and William A Hall for arranging such an exciting session with an engaged and large audience. Was a big pleasure to speak about trial design issues in oncology and introduce the Common Sense Oncology movement to the audience!

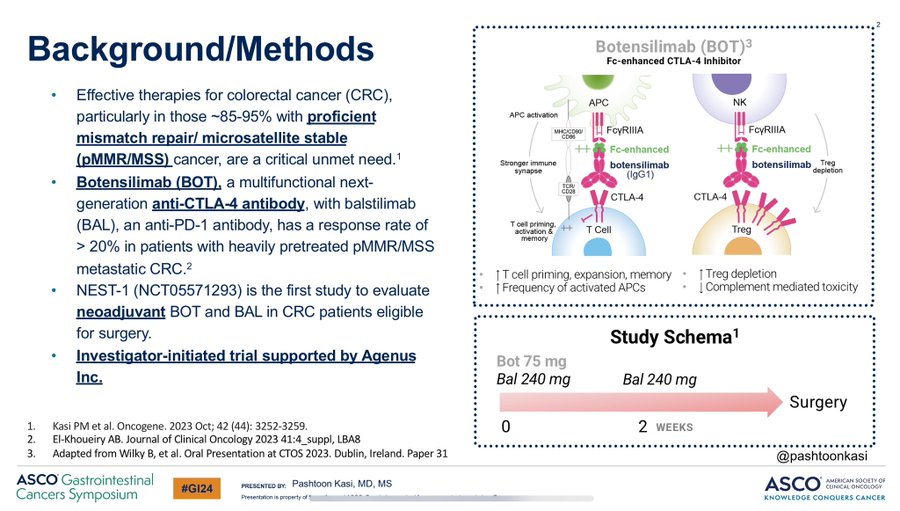
Pashtoon Kasi (USA)
Just out: NEST-1 trial results: Are we on the verge of a new drug combo for colon or rectal cancer? Substantial and brisk responses to just one dose of BOT (botensilimab) plus BAL (balstilimab) and immunotherapy. Abstract 117 at Poster Board H2.
Thank you, OncLive.com, for doing a comprehensive piece on our NEST-1 clinical trial with BOT/BAL. This tells such a nice story with all the relevant details. Link for details. Sharing the waterfall plot:
Here’s a 2 minute poster presentation of our NEST-1 clinical trial. Thank you to Colorectal Cancer Alliance for showing up at 6:30 PST! Patient advocacy and education you do is much appreciated.
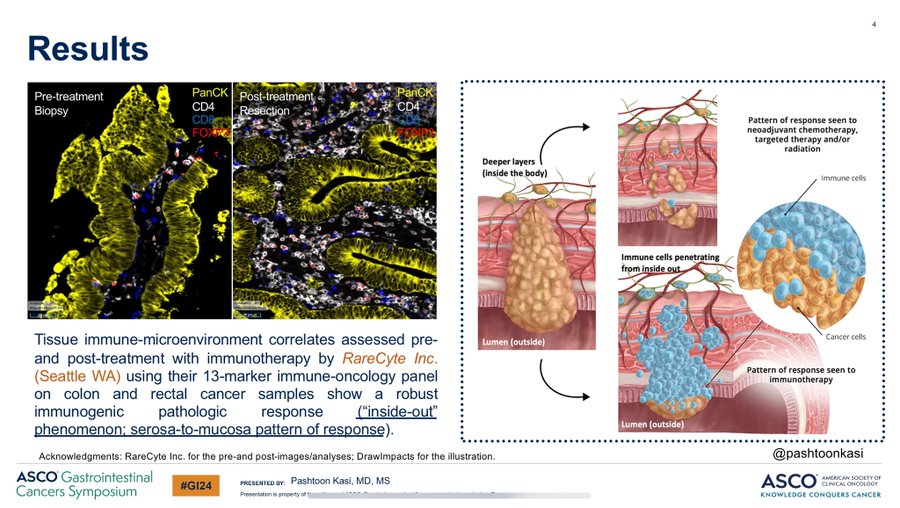
What’s very intriguing is the pattern of response:
- “Inside-out”
- “Root-up”
- “Serosa-to-mucosa” pattern of response
Cancer cells even when present were all near the luminal surface. Has very distinct implications in the adjuvant setting, potentially high rates of cure.
A little bit about the design of the NEST-1 trial and the drug Botensilimab (BOT).
The study has expanded to a cohort of patients with MSS who would have the chance to have a longer duration of exposure to immunotherapy (~8 weeks), and an additional cohort of patients with MSI-High for watch-and-wait.
Great questions by Filip Van Herpe. Answering them on the thread here.
Q. Delay in surgery? A. No surgery delayed
Q. Severity of toxicity? A. Only 1 Grade-3 diarrhea – managed with infliximab – surgery 6 days later
Q. cTNM staging of all patients? A. Correlation cTNM VS pTNM difficult. The cTNM and pTNM shown below – see the significant DOWNSTAGING – colonic staging will always be challenging but we had 4 MRIs for rectal cancer. CT can understage MSS & overstage MSI-High
Q. How did you Assess tumor regression? A. Standard methods of regression as per NICHE-1
Q. NGS of patients? A. NGS/DNA/RNA – regular run of the mill colon and rectal cancer. See poster below. Illumina TSO-500 on all Patient’s samples plus we will have RareCyte on all pre and post in the next few days.
See the 2 minute take of Myriam Chalabi on our NEST-1 trial. Our trial did allow patients with rectal cancer to enroll if after multi-disciplinary tumor board discussion, the plan was for surgery. If that was the case, they were allowed to get BOT/BAL.
Aparna Raj Parikh (USA)
GI24 my favorite. Congrats to Rachna Shroff and team for another great year. Hearts and brains full plus got training in. Most compelling for me, Colon Cancer and Colorectal Cancer (CRCSM) ipi/nivo vs chemo curves and 2 year Disease-free survival (DFS) (await nivo data but a soc option). Also, look forward to more MSS localized bot/bal data.

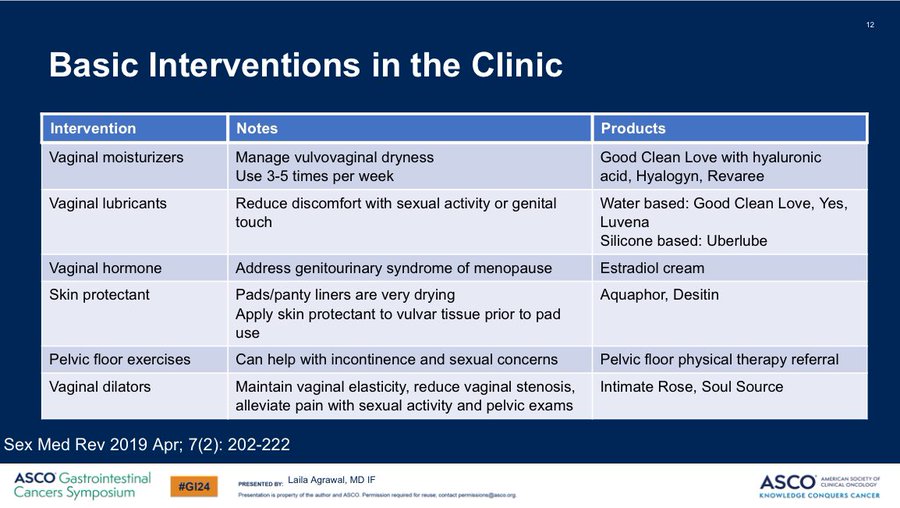
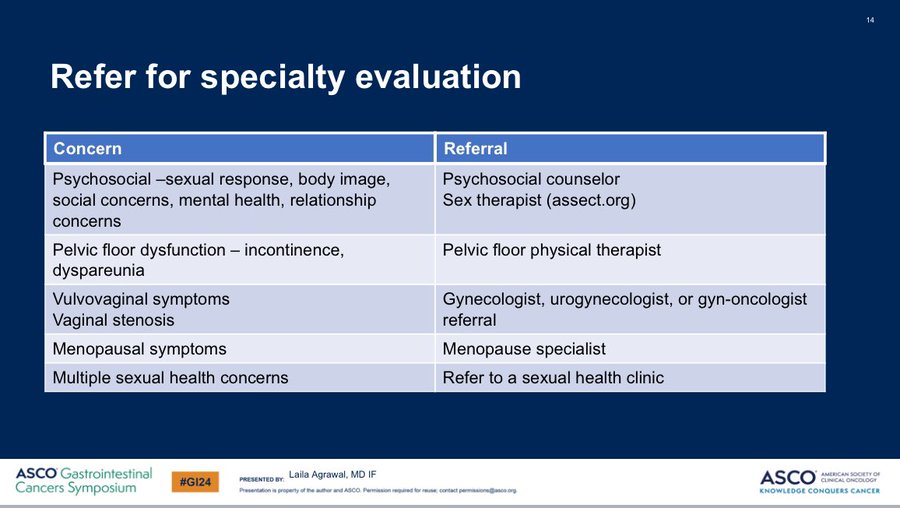
Laila Agrawal (USA)
It was an honor to speak at ASCO GI24 supportive care session on fertility and sexual health after colorectal cancer (CRC). Here are pearls that oncology professionals can take back to their clinics Monday morning.
75% of patients with CRC have sexual health concerns after treatment, yet most patients do not recall any discussions about sexual health. Maybe because medical training teaches the value of a women’s role in reproduction, but does not value female sexuality.
- Assess sexual health concerns throughout cancer treatment and follow up. Use a ubiquity statement. “It is really common for patients with CRC to experience changes to sexual health. Do you have any concerns?” Start this conversation early, don’t wait for problems to develop!
- Offer basic interventions in the clinic Vaginal moisturizers, lubricants (silicone based), vaginal hormones, skin protectants if using pads, instruction on vaginal dilators. Vaginal dilators should be recommended to patients receiving pelvic radiation. Discuss use prior to radiation. Start within 4 weeks (may vary). Use a few times a week for 5-10 minutes (may vary).
- Referrals to specialists. Sex therapists, counselors, pelvic floor PT, menopause specialists, gynecology specialists. Early onset CRC is rising and patients are not going to accept our neglect of this important aspect of quality of life. It is critical that ALL oncology professionals address sexual health and fertility concerns for patients. How do we get there? Let me know your thoughts!
Nina Niu Sanford (USA)
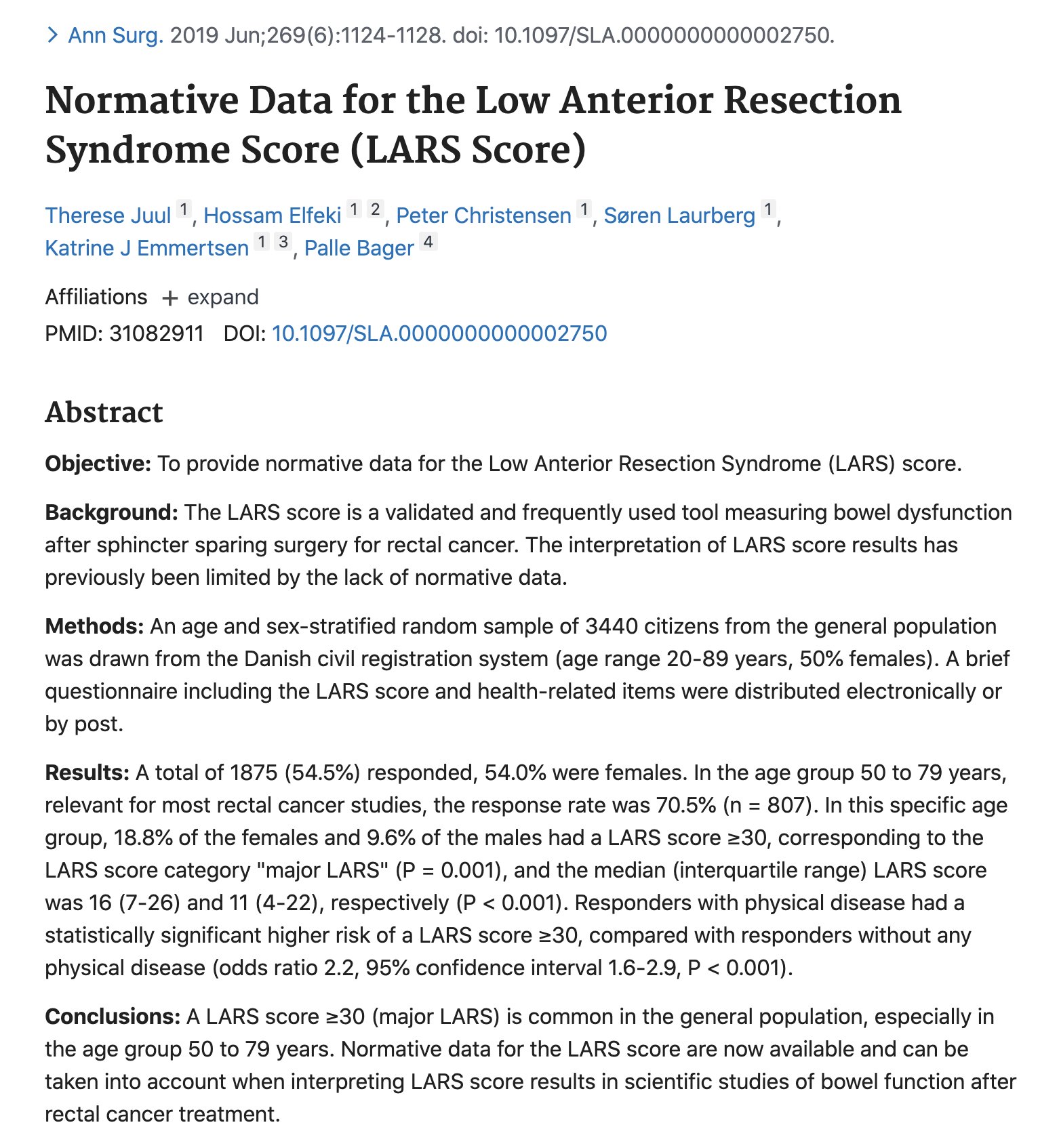
Lots of discussion on risk factors for Low Anterior Resection Syndrome Score (LARS). Something to keep in mind is % of individuals without rectal cancer (no surgery, RT) who endorse LARS. In this study of n=1,875 (general population, age 50-79), 19% of women and 10% of men had major LARS.
Joseph McCollom (USA)
I shouldn’t be here”. It’s not that I don’t feel like I belong here at GI24. These are my people. It’s more of a recognition of my personal statistics. A thread:
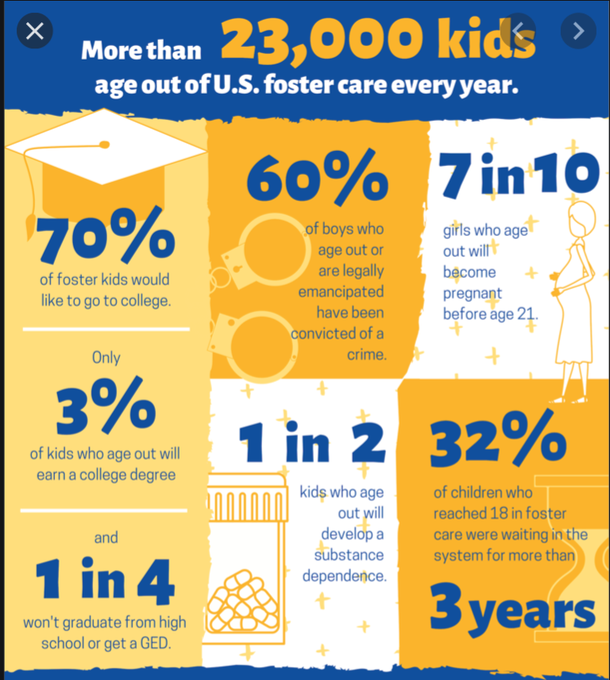
“I shouldn’t be here”, Because the orphanage I spent my 12th birthday in isn’t here. The foster agency that handled my case until 18 isn’t here.
“I honestly should be dead”, like that 9 year old boy at the bottom of the lake. Like hundreds of foster children, I grew up alongside, left neglected, abused and forgotten. Like the hundreds of thousands of foster kids still in the system and wondering if hope should be abandoned.
“I honestly should be dead” Or incarcerated (40-60%) Or on substances (50%) Or no high school diploma (75%) Or jobless (48%).
“I shouldn’t be here”. I know she’s saying it in her head too, downcast eyes on wringing hands as we review her pathology together. “I honestly should be dead”, It bursts forth in the tears of the pancreatic cancer survivor when the scans he’s been dreading for weeks come back NED (No evidence of disease).
But we are here, alive and together As long as there are compassionate providers, empowered patient voices, innovative researchers, faithful allies and quality conferences, there is hope. As long as there is fellow sufferers offering sincere support, hope remains.
Thanks to Don Dizon for telling my story and The Oncologist Journal for publishing. Thanks for the honor of being a featured voice for GI24 and for every wonderful connection made and every story shared.
Nina Niu Sanford (USA)
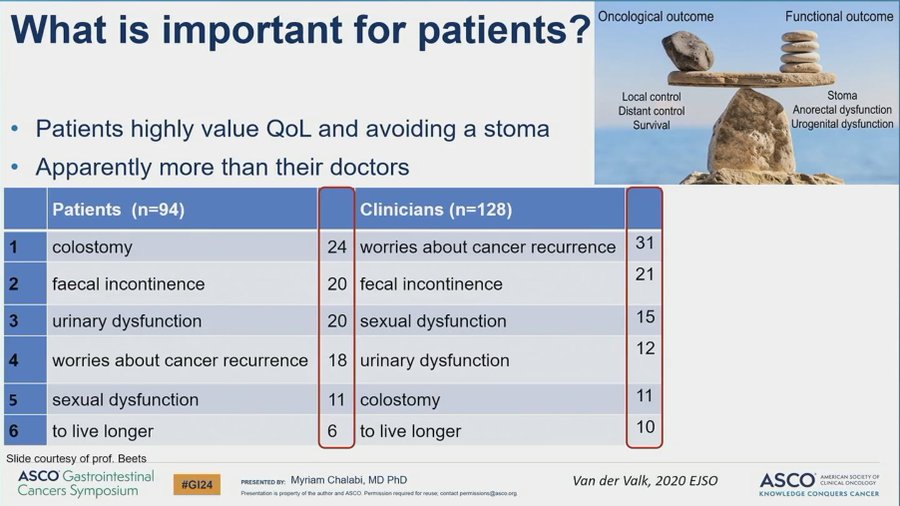
Patient vs. clinician values in rectal cancer. Cancer recurrence and colostomy were pretty much flipped between patients and clinicians. But both groups valued living longer last? Does anyone know the reference for this study? Great talk, Myriam Chalabi!
Melissa Lumish (USA)
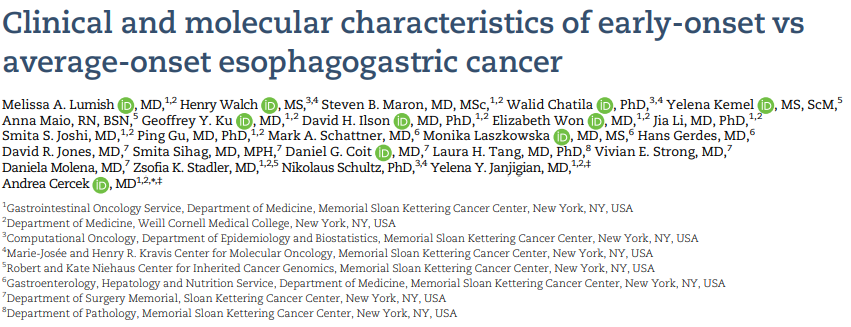
Early onset GI cancers will be highlighted at ASCO GI24. EO-EGC is rising along with colorectal cancer. Our results in Journal of the National Cancer Institute (JNCI) show EO-EGC is: increase of gastric diffuse type influences stage/survival. Much still unknown. Fantastic collaboration.
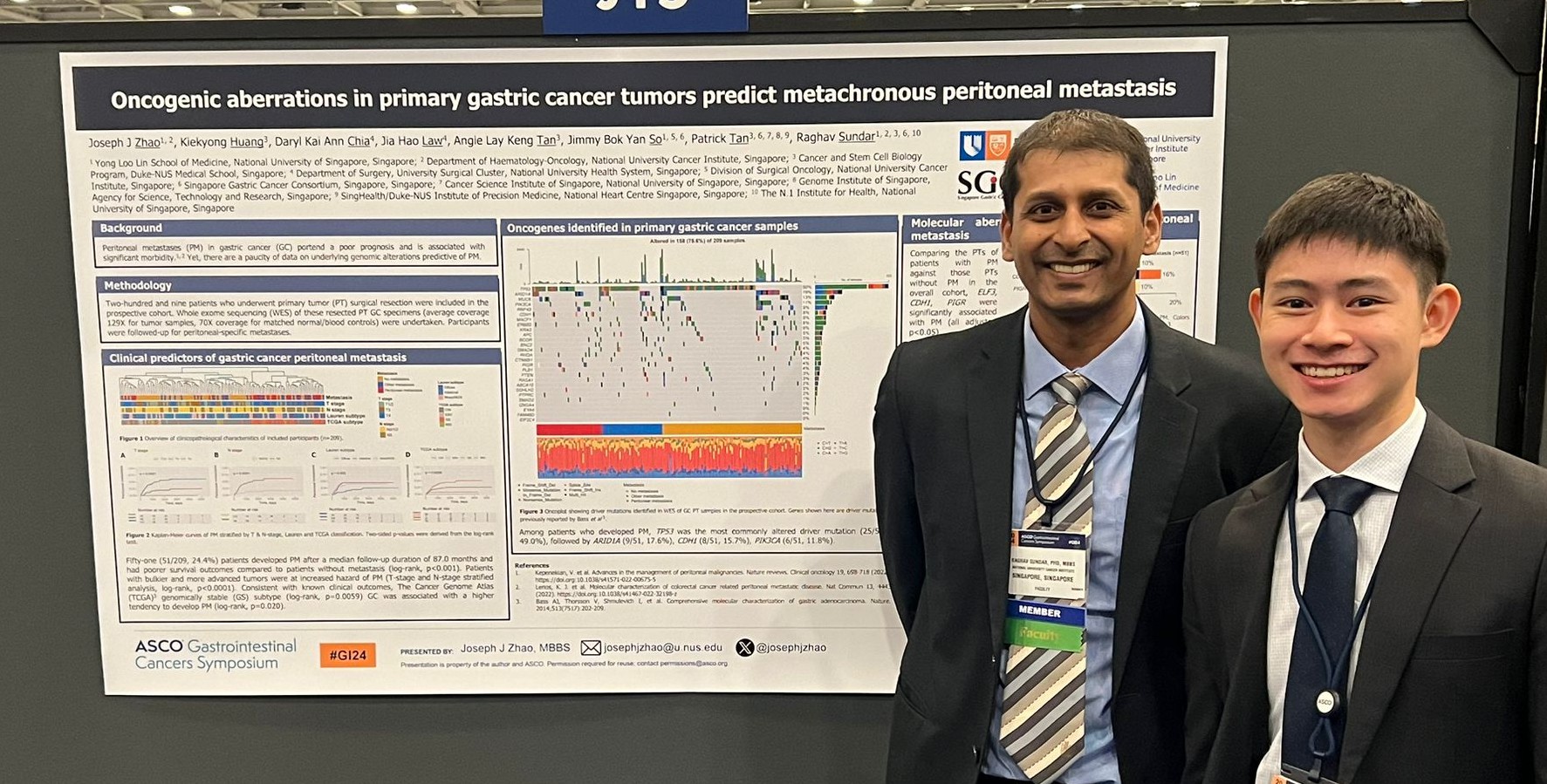
Raghav Sundar (Singapore)
Cancers don’t metastasize to distant sites equally. Tumors have varied affinities to different organs, termed organotropism. We share insights from our study to factors that lead to stomach cancer spreading to the peritoneum at GI24 in this poster by Joseph J Zhao.
Richard Dunne (USA)
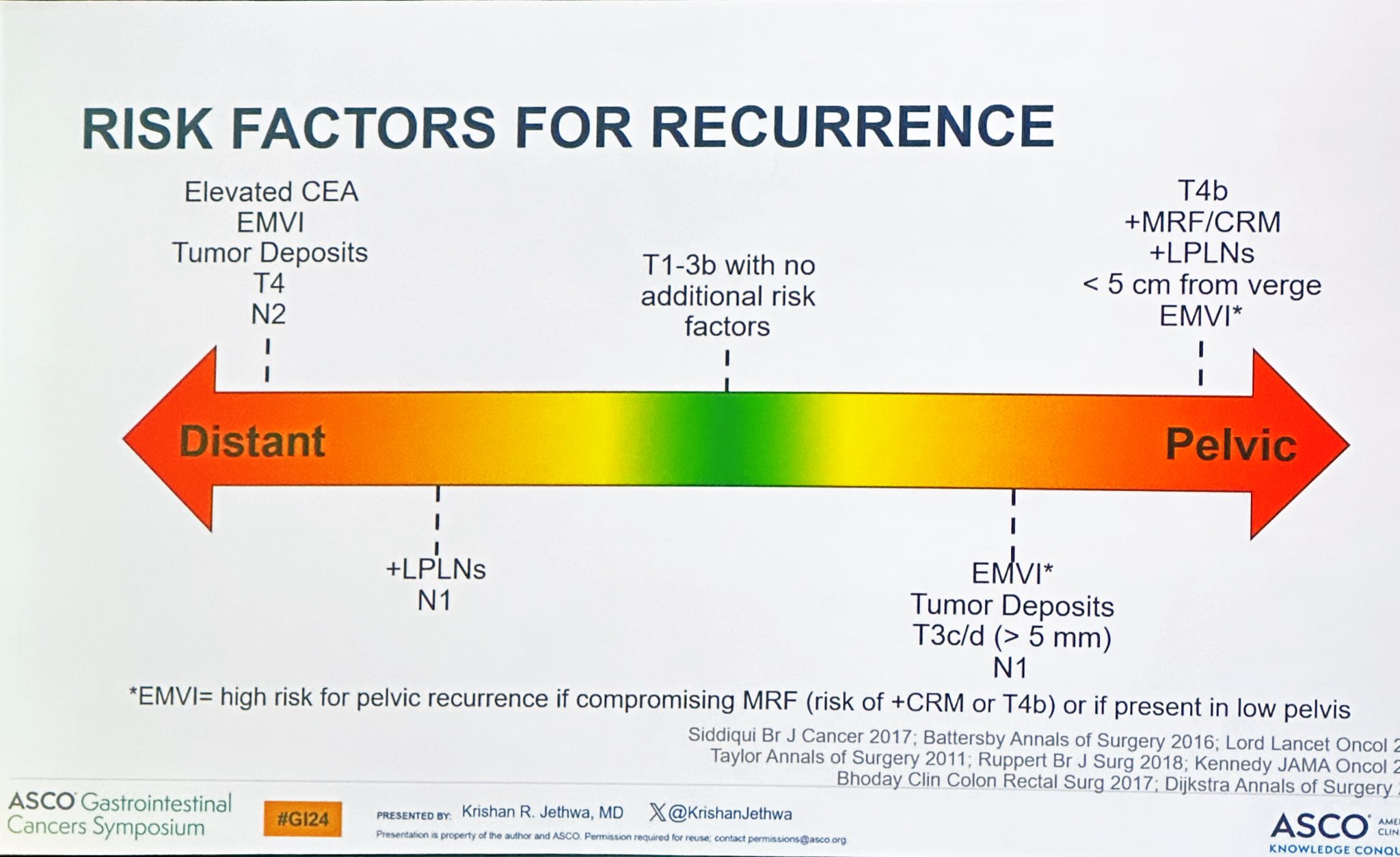
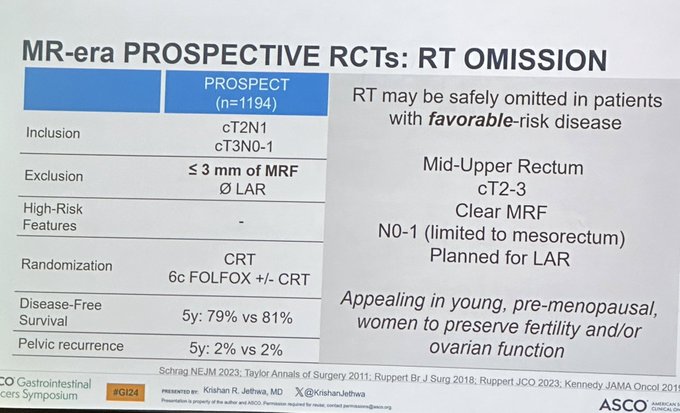
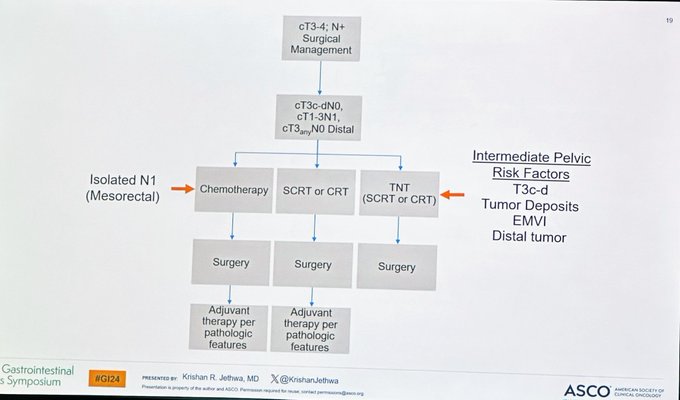
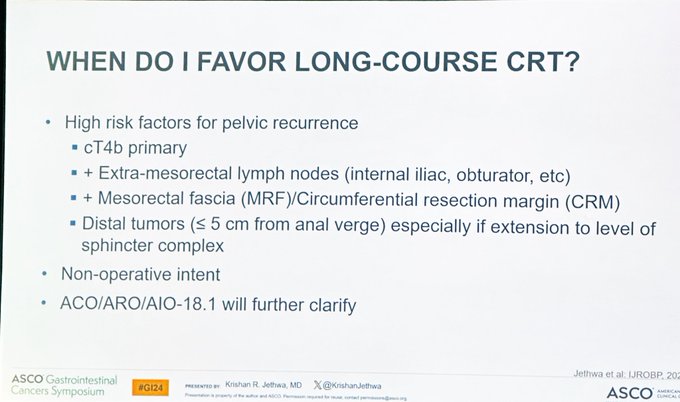
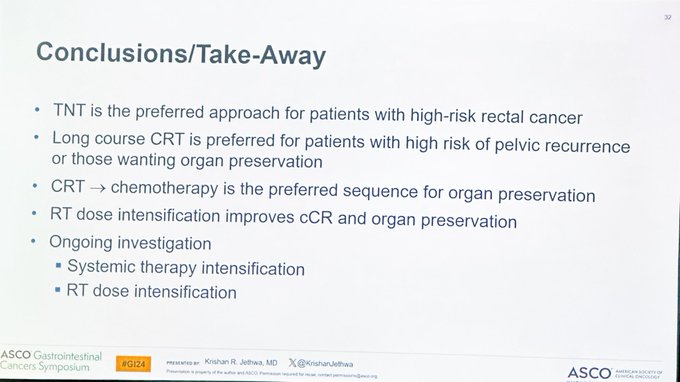
My favorited educational talk of GI24 was given by Krishan Jethwa who offered a well-balanced, well-informed but decisive view on Neoadjuvant treatment in rectal cancer. Trying to summarize his talk.
Radiotherapy maybe omitted for:
- cT2-3
- mid to high tumors with planned low anterior resection (LAR)
- clear effects of mesorectal fascia (MRF)
Choose Total neoadjuvant therapy for:
- high risk cancers
- intermediate risk rectal cancers (T3c-d, tumor deposits, distal tumors with Extramural vascular invasion (EMVI))
Use long course over short course if:
- High risk for pelvic recurrence (cT4b, extramesorectal lymph nodes, Circumferential resection margin (CRM), distal tumors)
- Those seeking organ preservation
Use Chemo-radiotherapy before chemotherapy if seeking organ preservation. Congrats Krishan Jethwa on an excellent talk.
American Society of Clinical Oncology (ASCO)
A recording of Kimmie Ng‘s GI24 keynote lecture is now available, “The Growing Problem of Early-Onset Gastrointestinal Cancers.” Watch here.
Arndt Vogel (Germany)
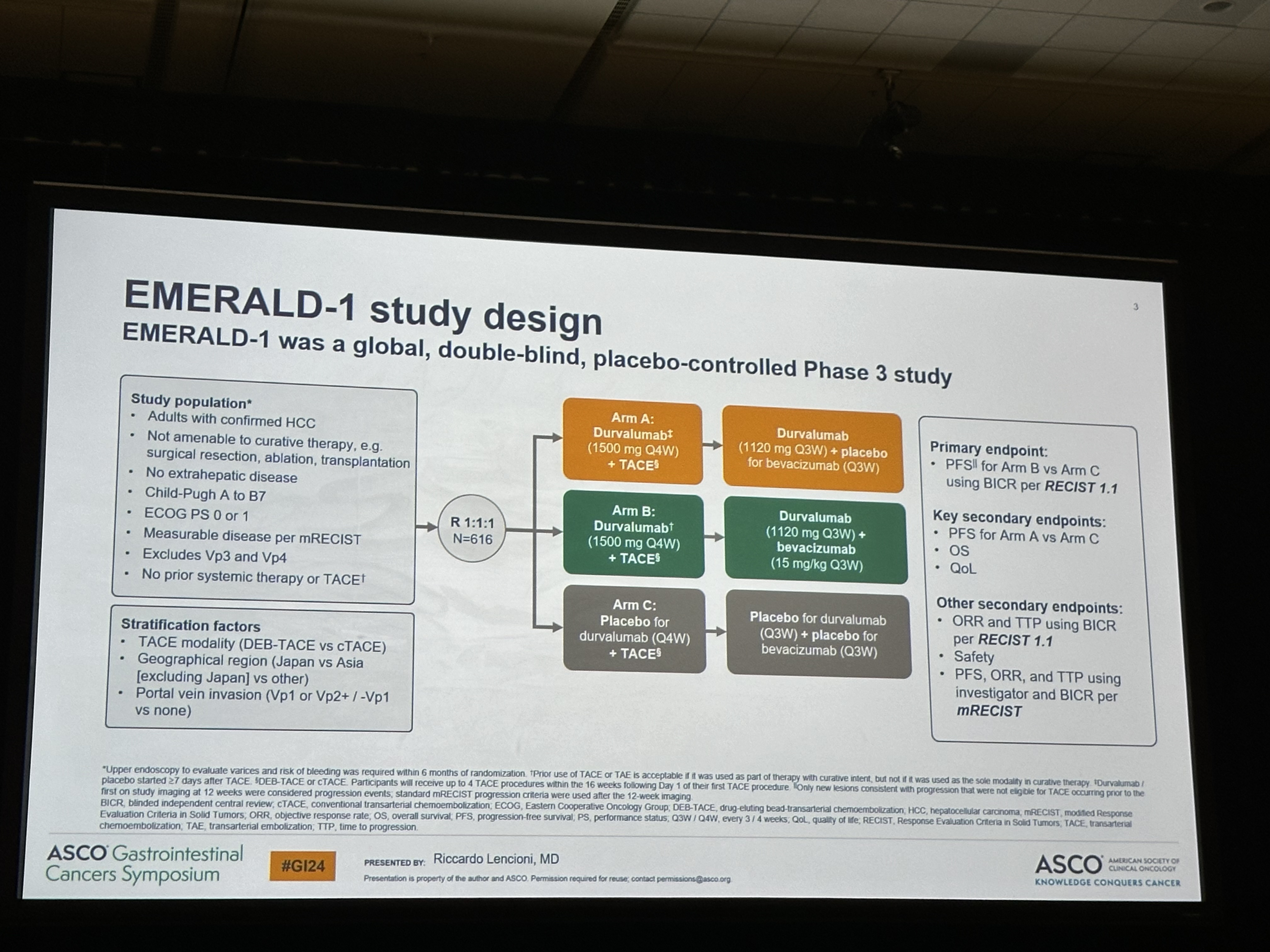
Transarterial Chemoembolization (TACE) plus durvalumab with or without bevacizumab in hepatocellular carcinoma (HCC). EMERALD-1, 616 patients.
- Objective response rate: 41 vs 43 vs 29%
- median Progression Free Survival: 15 vs 10 vs 8.2 months
- median Overall Survival: too early
Interesting data, no Durva mono benefit? Bev adds efficacy (again). Practice changing?
Josh Smith (USA)
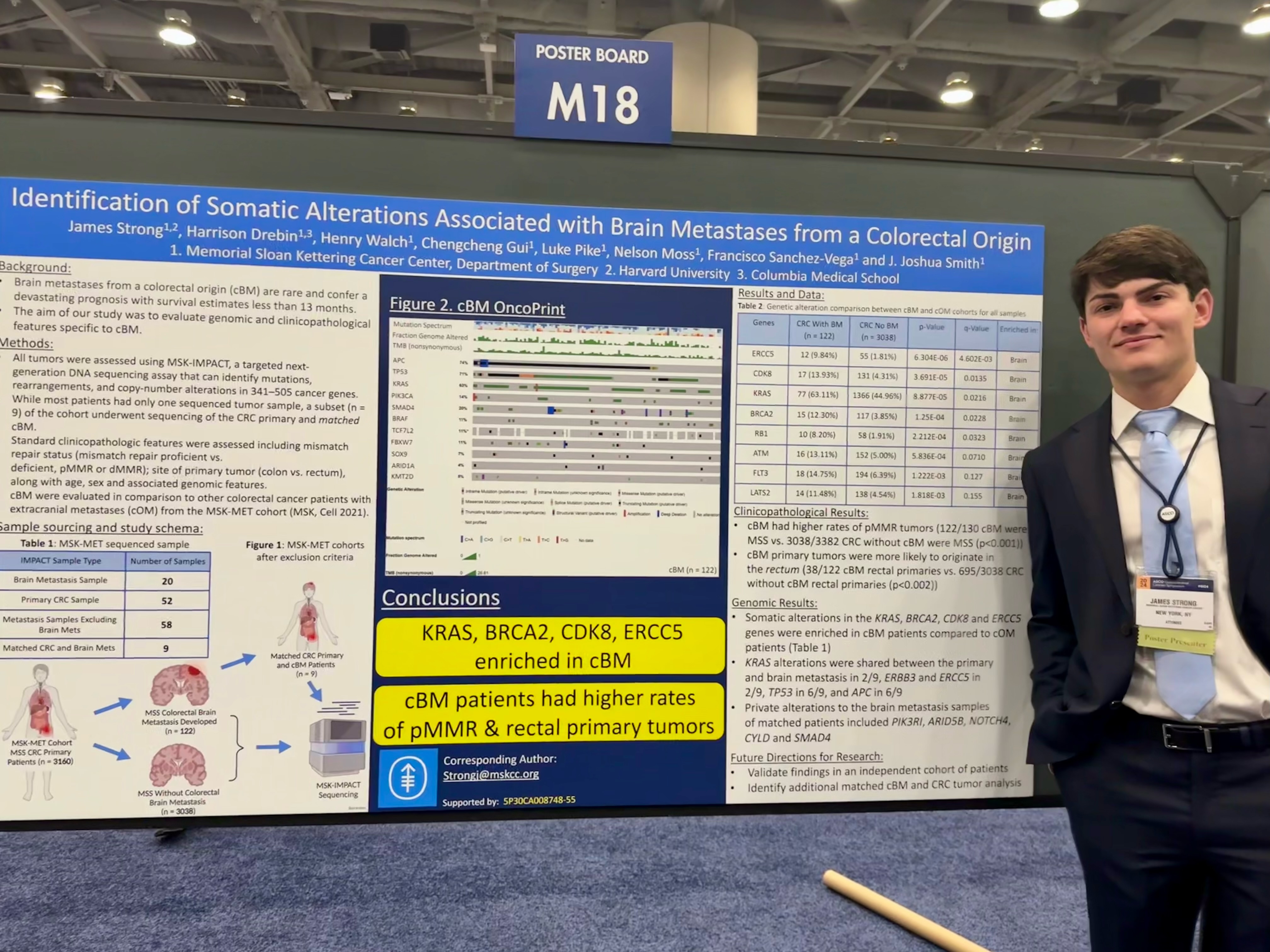
Busy morning at GI24 poster session with outstanding SmithLab and GarciaLab members representing Memorial Sloan Kettering Cancer Centre at GI24. Topics include: accuracy of endoscopy/MRI post-TNT, Local excision/ESD post-TNT, Rectal Cancer Tumoroid Biorepository and brain metastasis genomics from colorectal origin.
Duilio Rocha (Brasil)
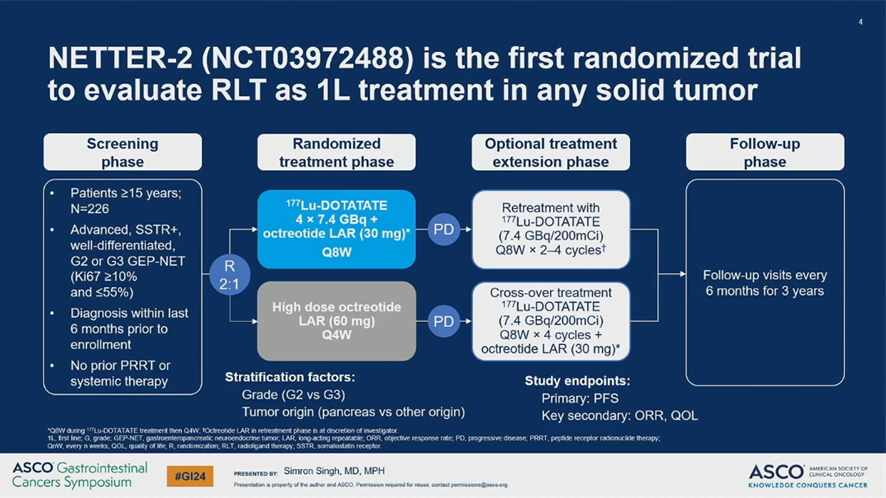
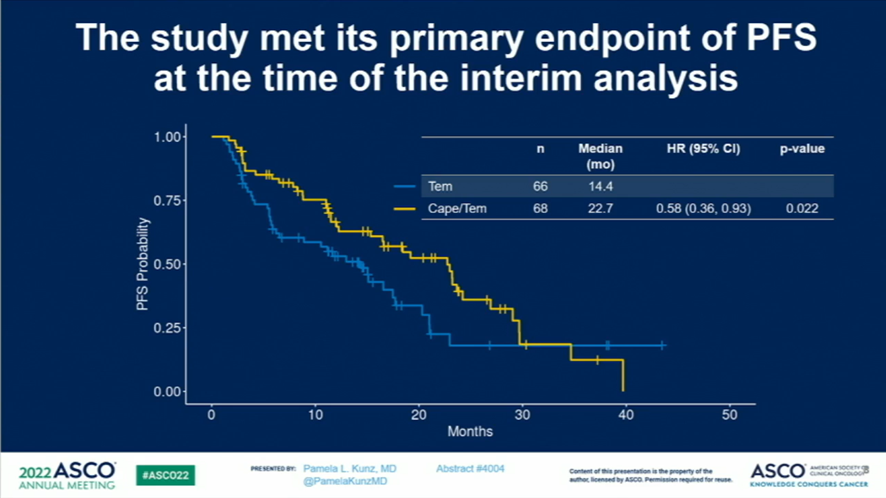
Comments on my personal top 4 GI24 abstracts (1/4): 1. NETTER-2
177Lu-DOTATATE vs high dose octreotide as 1L treatment of G2 or G3 GEP-NET (Ki67 between 10% and 55%): Increase of PFS (22.5 vs 8.5 mo, HR 0.27) and increase of ORR (43% vs 9%). I did not expect such good numbers.
Is octreotide the ideal control group?
- CAPTEM preferred over Somatostatin Analogs (SSA) in many NETTER-2 patients
- CAPTEM results (mPFS 22 mo, ORR 40%) similar to 177Lu
- Early PRRT may decrease tolerance to subsequent chemo
CAPTEM still option, especially for higher grade/higher volume PNET
- Patients on octreotide had a decent mPFS of 8.5 months
- Early Peptide Receptor Radionuclide Therapy (PRRT)? will induce 2% myeloid neoplasms (median time ~40 mo).
- No OS or QoL benefit with initial PRRT so far
- 177Lu may be considered as a subsequent therapy after SSA In lower grade, lower tumor burden G2-3 patients
NETTER-2 establishes PRRT as 1L for many G2-3 NET pts (with low to moderate tumor burden?). Over time, those patients may have less SSTR expression/less efficacy of PRRT. PRRT in late scenarium may not reproduce NETTER-2 results. NETTER-2 is my personal GI22 star.
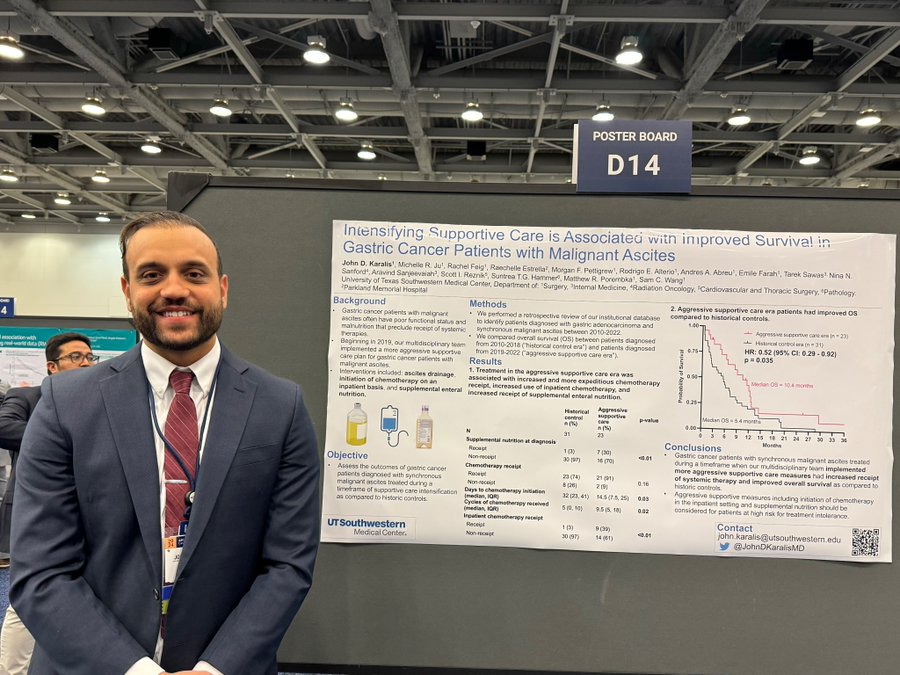
Sam C. Wang (USA)
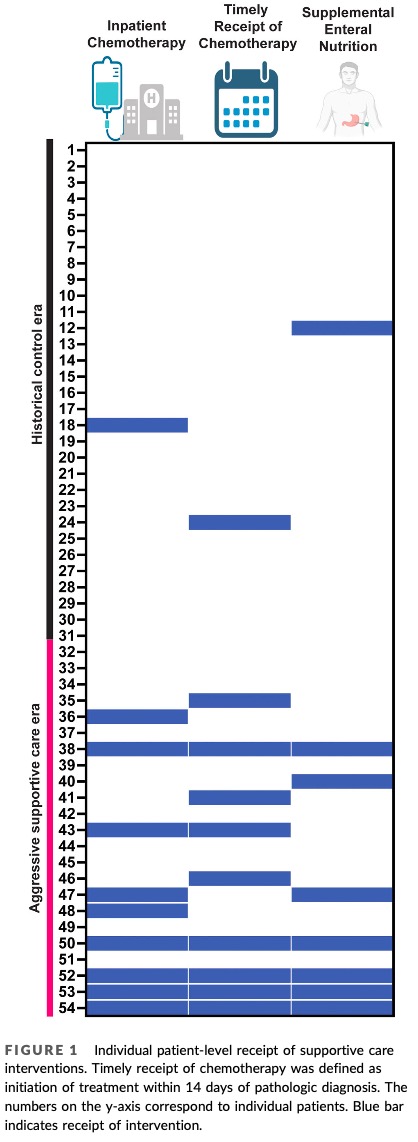
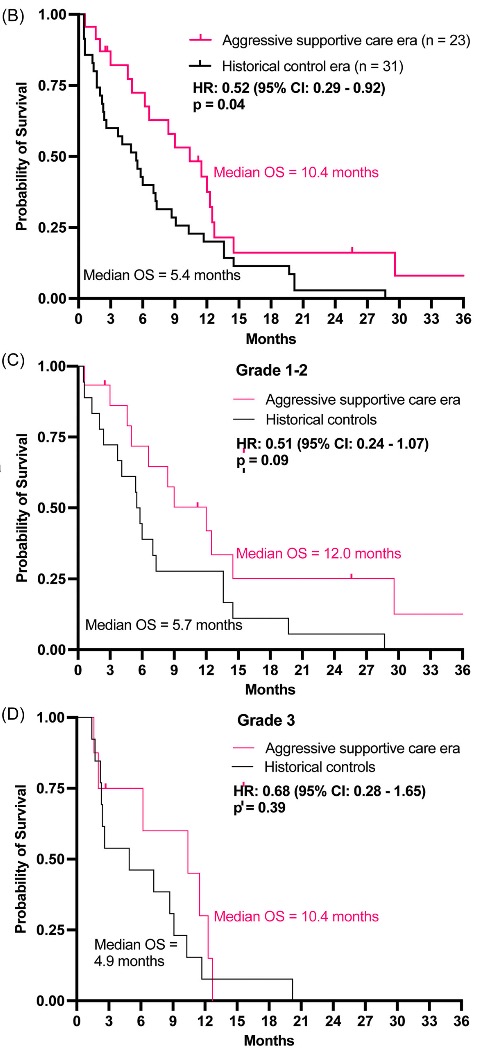
Here is John D. Karalis at ASCO GI24: “Intensifying supportive care is associated with improved survival in gastric cancer patients with malignant ascites” recently published in Journal of Surgical Oncology.
Gastric cancer patients who present with synchronous malignant ascites have median overall survival of 2-8 months. Significant contributors to their poor prognosis are poor functional and nutritional status due to the sequelae of ascites.
n 2019, our multi-D team became much more aggressive to admit these patients to the inpatient service to control symptoms, improve nutrition and functional status, and initiate therapy. We compared our institutional outcomes in the timeframe before and after 2019.
In the “aggressive care” era, patients had higher rate of receiving supplemental enteral nutrition, often via NJ tubes, and starting chemo as inpatients. Median time from diagnosis to chemo went from 32 days to 14.5 days and median cycles of chemo received went from 5 to 9.5.
We found that the median OS increased from 5.4 months to 10.4 months; and this was true in patients both mild to moderate ascites (grades 1-2) and severe ascites (grade 3).
While most patients still had very poor outcomes, aggressive supportive care may allow for the minority of patients with otherwise favorable underlying tumor biology to improve their functional status enough to receive treatment, (eg EBV+ or MSI-H tumors and IO).
As a signal, 3 of 23 patients in the aggressive supportive care cohort were alive 30 months after diagnosis (vs 0 of 31 historical controls). For me, the most striking part of our data is the median age of presentation: 46 years old. The “median” patient from our cohort is one who is working, married, and with young kids.
They come to the ED with months of abdominal discomfort and while in ED, receive news that they have widely metastatic cancer with only months to live. We can imagine that they may be deemed not candidate for systemics due to rapidly declining functional and nutritional status.
Our findings suggest that if we overcome nihilism that may sink in when caring for these patients with really challenging clinical problems, we can give them a bit more time with their families and maybe even help a small handful achieve longer-term survival.
While we did not formally gather QoL data for patients in this analysis, from our anecdotal experience, we found that for a number of patients, they felt a lot better after getting on therapy. This study has headed by John D. Karalis of UTSW Surgery. Look for him in the current CGSO fellowship application cycle.
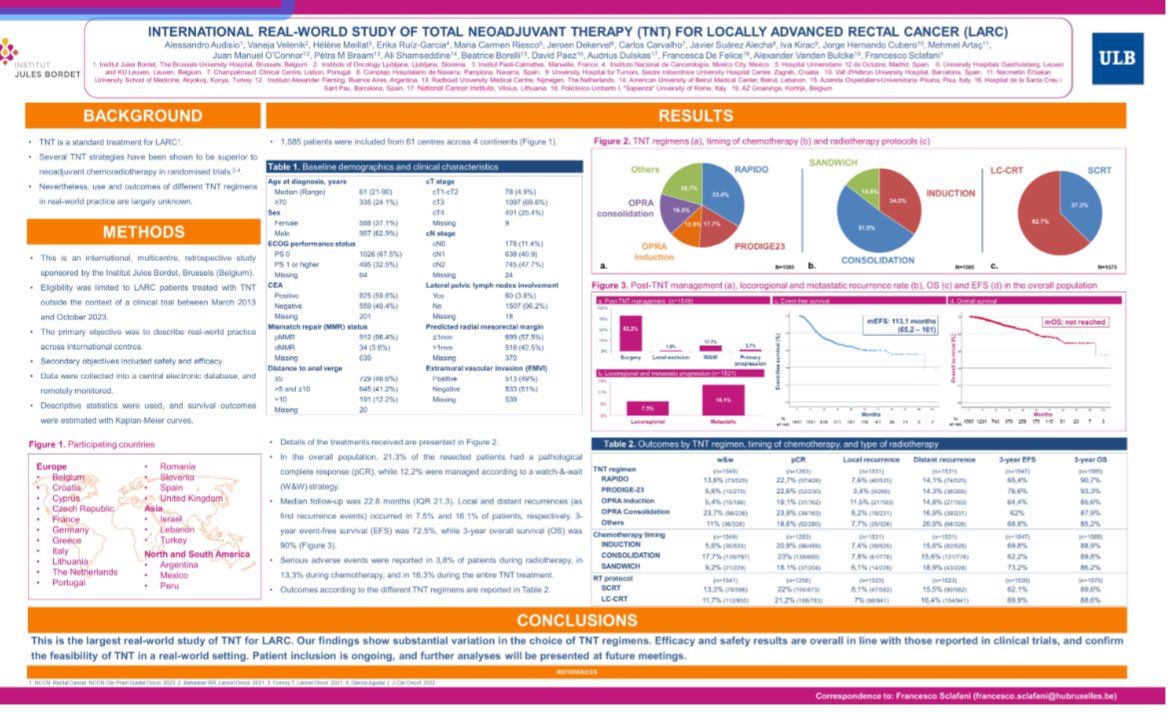
Juan O’Connor (Argentina)
Great international cooperative real world study, Total Neoadjuvant Therapy (TNT) in rectal cancer!! 1585 pts, variable TNT regimen and 12 % watch and wait. Great job Alessandro Audisio, Erika Ruiz-Garcia and team.
Jordan Berlin (USA)
Taking advantage of the fact that my GI24 talk resulted in about 100 new followers to repeat my usual mantra: Reject Hate. Avoid Anger. Be Kind to Animals and People. Forgive Always. Respect Others. Most of All, Care.
Mark Lewis (USA)
Having an NG tube removed after 5 weeks was, without exaggeration, one of the greatest moments of my life. Please do not underestimate the misery of delayed gastric emptying after gastroenteropancreatic surgery!

Vivek Subbiah (USA)
So nice catching up with the amazing Timil Patel from the US FDA about simple/pragmatic trial designs in oncology at ASCO GI24 meeting.
Since clinical trials in oncology that are submitted for regulatory review are becoming more and more complex – Dr. Patel and colleagues from the FDA Oncology, US FDA recently in a commentary called upon the drug development community to find ways to make clinical trials simpler.
When less is more – reducing complexity in cancer trials.
Cathy Eng (USA)
Fantastic Women in GI networking event last night! Thank you, Pfizer Oncology Medical for supporting us! Kristen Ciombor, Smitha Krishnamurthi, Pamela Kunz, Efrat Dotan, Nataliya Uboha, Carolina Bernabe, Shruti Patel and so many others!

Dana-Farber’s Breast Oncology Center
Congratulations to Rachel Freedman, recipient of the George P. Canellos Award for Excellence in Clinical Investigation and Patient Care! Dr. Freedman is recognized for her leadership, creativity, and productivity in advancing the field of oncology.
Rachna Shroff (USA)
No words to describe the feeling I have in a post GI24 glow! Thanks to ASCO, the committee, the speakers and the over 4500 attendees! I am so honored to have played a small role in a memorable event! With my heart full, I’m back with my babies!

At GI24? Stop by the ASCO booth to meet with Pamela Kunz, the Editor of our newest journal, JCO Oncology Advances! Learn more about JCO OA.

American Society of Clinical Oncology (ASCO)
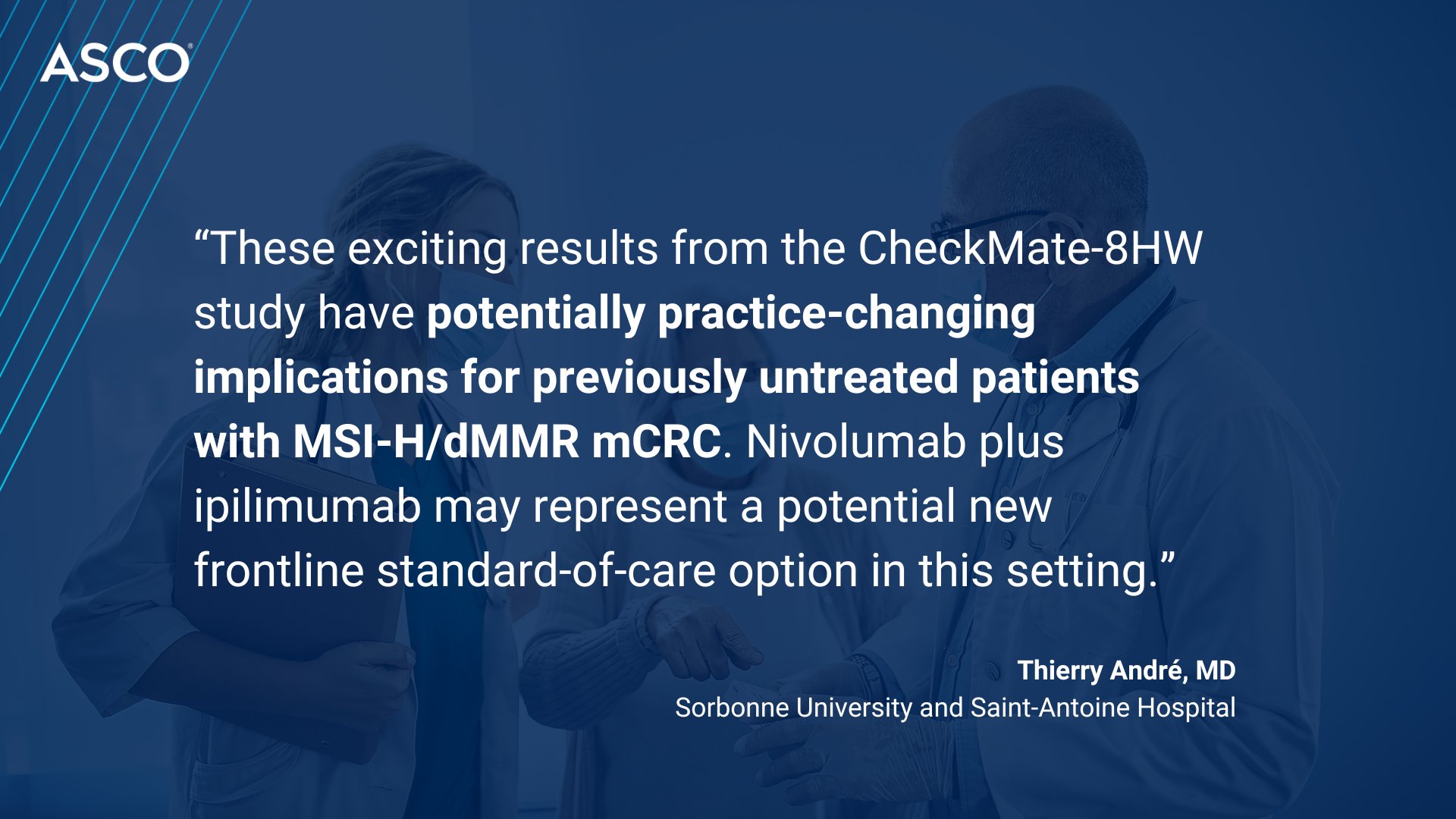
Breaking news from GI24: CheckMate-8HW shows that 1L nivolumab + Ipilimumab improves progression free survival vs chemo in MSI-H/Deficient mismatch repair (dMMR) Metastatic Colorectal Cancer (mCRC), reinforcing the regimen as a potential treatment option in 1L mCRC.