Douglas Flora, Executive Medical Director of Yung Family Cancer Center at St. Elizabeth Healthcare, President-Elect of the Association of Cancer Care Centers, and Editor in Chief of AI in Precision Oncology, shared a post on LinkedIn:
” ‘We choose to go to the moon in this decade and do the other things, not because they are easy, but because they are hard.’
April 13, 1970: When Simulation Saved Lives
Two hundred thousand miles from Earth, an oxygen tank exploded aboard Apollo 13. The spacecraft – meant to be humanity’s third lunar landing – was suddenly a crippled vessel with three astronauts whose survival depended on systems never designed for the crisis they faced.
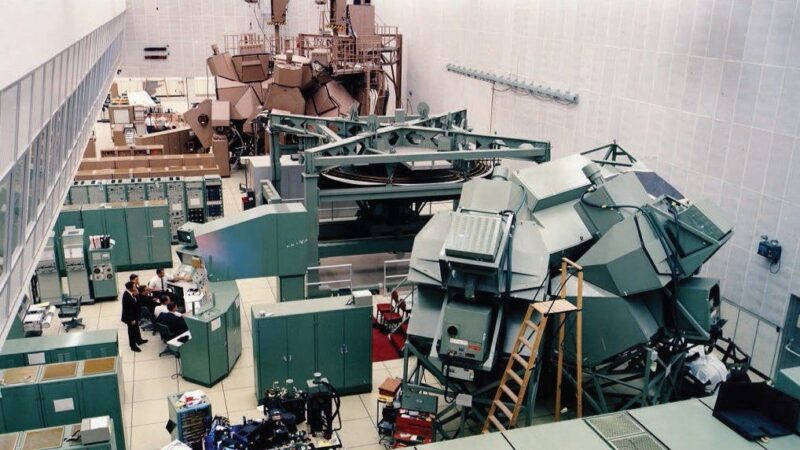
In the hours that followed, while the world watched and prayed, NASA engineers gathered around a perfect replica of Apollo 13 on the ground in Houston. This simulator, an exact duplicate of the spacecraft, became their laboratory. Every proposed solution, every jury-rigged fix, every creative workaround was first tested in this earthbound twin before instructions were radioed to the crew.
When engineers needed to stretch the Command Module’s lithium hydroxide canisters to accommodate three people instead of two, they tested this modification in the simulator. When they had to power down systems to conserve energy, then power them back up in a specific sequence to avoid electrical failure, they rehearsed it first in Houston. When they calculated the precise engine burn needed to correct the trajectory using only the Lunar Module’s thrusters, they verified it on the ground.
The simulator was more than just a training tool. It was a predictive model – a digital twin that allowed NASA to see the future before the astronauts lived it. To test interventions safely before implementing them in a life-or-death situation. To make mistakes on the ground so they wouldn’t make them in space. All three astronauts came home alive.
The Problem We Face Today
In oncology, we’re asking patients to be test pilots without the benefit of simulators. We prescribe chemotherapy regimens knowing they work on average across populations. Still, we are uncertain how they’ll affect this specific patient with their unique genetic makeup, metabolic profile, and constellation of comorbidities. We dose medications based on body surface area and organ function. Still, we’re making educated guesses about how quickly their body will clear the drug, how intensely they’ll experience toxicity, and whether the tumor will respond.
We enroll patients in clinical trials that might take years to show benefit – or harm – without the ability to preview what’s likely to happen to the individual sitting in front of us. We make irreversible treatment decisions, then wait to see if we made the right choice. This isn’t a failure of medicine. It’s a limitation of what’s been technically possible until now.
But what if – like NASA with Apollo 13 – we had a simulator? What if we could test treatments on a digital version of the patient before administering them to the actual person? What if we could preview toxicities, predict responses, and optimize dosing based not on population averages, but on an individualized model that accounts for each patient’s specific biology? This isn’t science fiction. It’s happening now, and it’s called a digital twin.
What Is a Digital Twin?
A digital twin in medicine is a dynamic, computational model of an individual patient that integrates multiple streams of data – genomics, proteomics, metabolomics, medical imaging, electronic health records, wearable device data, even environmental and lifestyle factors – into a living simulation that predicts how that specific patient’s body will respond to interventions.
Think of it as your patient’s doppelgänger existing in silicon instead of flesh. But unlike a static photograph or even a detailed anatomical scan, a digital twin is alive in its own way – constantly updating as new data streams in, running scenarios, predicting outcomes, learning from what actually happens, and refining its predictions accordingly.
In oncology, digital twins are being developed to:
Predict treatment response before the first dose: By modeling tumor biology, immune system interactions, and drug pharmacokinetics specific to the patient, digital twins can estimate which regimens are most likely to work – and which are likely to fail or cause unacceptable toxicity.
Optimize drug dosing using pharmacogenomics: Rather than relying on population-based nomograms, digital twins incorporate genetic variants affecting drug metabolism to calculate personalized dosing that maximizes efficacy while minimizing toxicity.
Reduce complications of therapy: By simulating how treatments affect not just the tumor but the whole patient – cardiac function, bone marrow reserves, nutritional status, wound healing – digital twins can flag patients at high risk for specific complications before they occur.
Accelerate clinical trial conduct: Digital twins can serve as synthetic control arms, reducing the number of patients needed for trials. They can also identify which patients are most likely to benefit from experimental therapies, making trials more efficient and ethical.
Extend healthspan, not just lifespan: By modeling the long-term effects of cancer treatments on organ systems, digital twins enable clinicians to balance tumor control with quality of life, optimizing for health over years rather than just survival.
The Mission Control Moment
Let’s explore a real-world application of digital twins in oncology. Imagine a patient with metastatic colorectal cancer and the UGT1A1*28 variant. Now, envision having a continuously updated digital twin of this patient integrated into their care.
When considering an irinotecan-containing regimen, the digital twin does more than flag the pharmacogenomic variant. It actively simulates the potential outcomes of a standard dosing approach. Based on the UGT1A1 genotype, baseline bone marrow function, nutritional status, concurrent medications, and other critical factors, it probabilistically indicates the likely severity of neutropenia the patient may experience.
Furthermore, the digital twin runs various alternative scenarios. This includes simulations for reduced irinotecan dose levels (e.g., 70% and 50%) and entirely different treatment regimens. For each simulation, it predicts:
- Tumor response probability
- Toxicity risk
- Impact on quality of life
- Overall survival outcomes
The digital twin doesn’t make decisions; instead, it acts as “Mission Control for Cancer Care.” It provides a glimpse into the future under different treatment paths, empowering clinicians to make informed and precise therapeutic choices. The principle is clear: test the intervention on the digital twin first, then implement it on the patient.
The Concerns Worth Addressing
Like any transformative technology, digital twins raise legitimate questions:
Accuracy: How do we validate that digital twins accurately predict individual outcomes? The answer lies in continuous learning – every treatment given, every outcome observed, becomes data that refines the model. Digital twins become increasingly intelligent over time, both for individual patients and across populations.
Privacy: These models require intimate biological data. Protecting patient privacy while enabling the data sharing necessary for model improvement requires robust frameworks – such as encryption, federated learning approaches, and patient control over data use.
Access and equity: Will digital twins be available only to patients at academic medical centers or those with specific insurance? This is the most critical concern. The technology must be designed for broad accessibility; otherwise, it will exacerbate existing disparities.
Clinical integration: How do we present complex probabilistic predictions to clinicians and patients in ways that inform rather than overwhelm decision-making? The user interface matters as much as the underlying algorithms.
These concerns aren’t reasons to avoid digital twins – they’re design requirements for implementing them responsibly.
From Apollo to Oncology
The Apollo 13 mission succeeded because NASA had the wisdom to build a simulator before it was needed in a crisis. They understood that when lives hang in the balance, you don’t experiment on the only copy – you test on the twin.
Medicine is finally catching up to this principle. Digital twins represent the next evolution in AI-driven cancer care – moving beyond reactive alerts (like the co-pilot catching the UGT1A1 variant) to proactive simulation. From “don’t make this mistake” to “here’s what will probably happen if you do this.”
This is what the future of precision medicine looks like: not just matching treatments to tumors based on molecular profiles, but matching treatments to whole human beings based on comprehensive biological models. Not guessing at outcomes, but previewing them. Not hoping for the best, but engineering for it.
The Healthier, Happier Future
The promise of digital twins extends beyond avoiding toxicity or optimizing dosing. It’s about fundamentally changing the patient experience of cancer care.
Imagine patients understanding their treatment plan not through statistics from clinical trials conducted on thousands of other people, but through simulations run on their own digital twin. Seeing, in probabilistic terms, what different treatment paths might mean for their tumor, their quality of life, their ability to work or travel or be present for their grandchildren.
Imagine oncologists freed from the anxiety of decision-making under uncertainty – not because decisions become automatic, but because they’re informed by individualized predictive models that reduce uncertainty. The art of oncology remains, but it’s practiced with better tools.
Imagine clinical trials that answer questions faster, expose fewer patients to ineffective treatments, and identify responders earlier. Research that accelerates because we can test hypotheses on digital cohorts before recruiting actual patients.
This isn’t just about living longer. It’s about living better – with less toxicity, more informed choices, and treatments calibrated to the individual rather than the average.
Houston, We Have a Solution
When Apollo 13’s oxygen tank exploded, the mission seemed doomed. The simulator in Houston – that digital twin of a spacecraft – turned a crisis into a testament to human ingenuity and technological partnership.
In oncology, we face our own impossible challenges every day. Tumors that evolve and adapt. Treatments that work brilliantly for some and catastrophically for others. Patients asking us to predict futures we can only guess at.
Digital twins won’t make cancer easy. But they’ll make our responses smarter, our treatments more precise, and our predictions more accurate. They represent the next chapter in AI-driven cancer care – the evolution from decision support to predictive simulation, from population-based medicine to truly personalized care.
The simulator is being built. The models are getting smarter. The future where every patient has a digital twin helping guide their care is not a distant dream – it’s an emerging reality.
And like those engineers gathered around Apollo 13’s simulator in 1970, we’re learning that the best way to help someone survive an impossible situation isn’t to guess better. It’s to test first, then act. To simulate before we treat. To avoid making mistakes on the twin, we ensure that we don’t make them on the patient.
Mission control is standing by. The digital twin is running. And the future of cancer care is becoming clearer – one simulation at a time.”
More posts featuring Douglas Flora.


