
Immunotherapy for Pancreatic Cancer
About Pancreatic Cancer
Pancreatic cancer is one of the most lethal and aggressive forms of cancer. It is the 12th most common cancer worldwide, with over 495,000 new cases diagnosed in 2020. The disease is characterized by its propensity for early metastatic dissemination, aggressive local invasion, and resistance to conventional chemotherapy and radiotherapy. The high mortality rate is also attributed to the late diagnosis of the disease, as pancreatic cancer often remains asymptomatic until it reaches an advanced stage.
Pancreatic cancer is projected to become the second leading cause of cancer-related deaths in the United States by 2030, surpassed only by lung cancer. This grim statistic underscores the urgent need for developing more effective treatment strategies and improving early detection methods for this devastating disease. The most common type of pancreatic cancer is pancreatic ductal adenocarcinoma, which accounts for about 85% of cases. Risk factors for pancreatic cancer include smoking, obesity, chronic pancreatitis, diabetes, and certain genetic mutations.
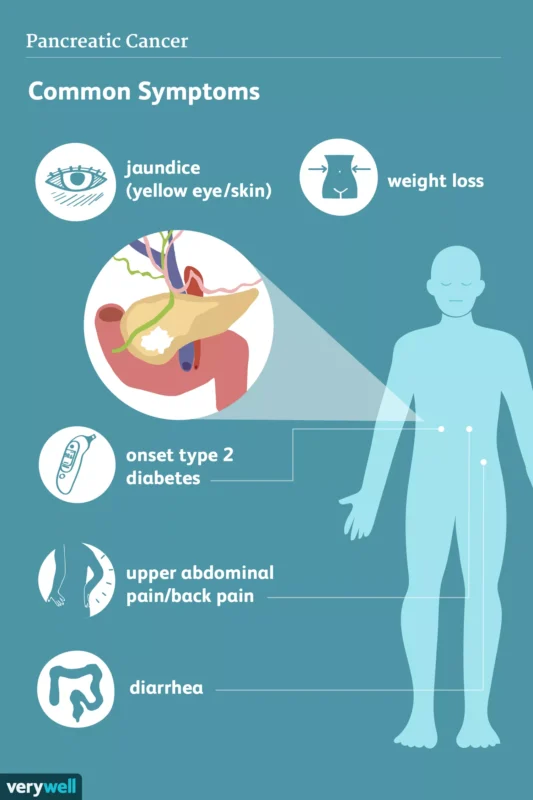
The image is taken from verywellhealth.com.
Cancer and the Immune System
The immune system plays a crucial role in protecting the body against illness and infection, including cancer. It comprises various cells and responses that identify and eliminate abnormal cells, including cancer cells. The immune system can recognize cancer cells as abnormal and kill them, but this response is often insufficient to eradicate cancer. Cancer cells can evade the immune system by exploiting mechanisms that suppress immune responses or by hiding from immune cells.
The immune system consists of two main components: the innate immune system, which provides immediate but non-specific defense, and the adaptive immune system, which offers a targeted and long-lasting response. The innate immune system includes cells like macrophages and natural killer (NK) cells that can recognize and destroy abnormal cells without prior sensitization. The adaptive immune system, comprising T and B cells, can recognize and remember specific antigens, allowing for a more efficient response upon subsequent exposures.
Cancer cells, however, have developed various mechanisms to evade the immune system. They can reduce the expression of antigens and major histocompatibility complex molecules, which are essential for immune recognition. Additionally, cancer cells can upregulate immune checkpoint proteins like PD-L1, which bind to receptors on T cells and inhibit their activity, effectively “turning off” the immune response. The tumor microenvironment can also become immunosuppressive, with the accumulation of regulatory T cells, myeloid-derived suppressor cells, and immunosuppressive cytokines, further hindering the immune system’s ability to attack the tumor.
Despite these evasion tactics, the immune system continues to play a critical role in controlling cancer. NK cells can recognize and destroy cancer cells without prior sensitization, providing a first line of defense. The adaptive immune system’s T cells can be activated to target and kill cancer cells that present specific antigens, contributing to a more targeted immune response. The ongoing interaction between cancer cells and the immune system is a dynamic process, with the immune system constantly adapting to recognize and combat cancer cells, even as they evolve to evade detection.
How Does Immunotherapy Work for Pancreatic Cancer?
Immunotherapy is a treatment approach that aims to harness and enhance the body’s natural immune defenses against cancer cells. In the context of pancreatic cancer, immunotherapy works by helping the immune system recognize and attack the cancer cells more effectively.
The immune system can detect and eliminate abnormal cells, including cancer cells. However, pancreatic cancer cells like other cancer cells can employ various mechanisms to evade the immune system’s defenses, creating an immunosuppressive tumor microenvironment. Immunotherapy drugs work by disrupting these evasion mechanisms, allowing the immune cells to identify and target the cancer cells for destruction.
One of the most successful immunotherapy approaches for pancreatic cancer is the use of immune checkpoint inhibitors. These drugs target proteins like PD-1 and CTLA-4, which act as brakes on the immune system. By blocking these proteins, checkpoint inhibitors can enhance the immune response against cancer cells. Pembrolizumab is an FDA-approved checkpoint inhibitor for pancreatic cancer patients with high microsatellite instability (MSI) or mismatch repair deficiency (dMMR). These genetic alterations are present in a small percentage of pancreatic cancer cases, but they can significantly improve the effectiveness of immunotherapy in these patients.
Types of Immunotherapy Drugs for Pancreatic Cancer
Immunotherapy for pancreatic cancer is an active area of research, with various types of immunotherapeutic agents being investigated in clinical trials.
Immune Checkpoint Inhibitors
- Pembrolizumab: Pembrolizumab is a PD-1 inhibitor that blocks the PD-1 protein on T cells, preventing cancer cells from evading the immune response. It is FDA-approved for pancreatic cancer patients with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR). These genetic alterations make the cancer cells more recognizable to the immune system.
- Nivolumab: Nivolumab is another PD-1 inhibitor used in various cancers. While not specifically approved for pancreatic cancer, it is being studied in combination with other therapies to enhance its efficacy against this disease.
- Dostarlimab: Dostarlimab targets PD-1 and is being investigated for its potential in treating pancreatic cancer, particularly in patients with specific genetic profiles similar to those treated with pembrolizumab.
Experimental and Combination Therapies
- BXCL701: BXCL701 is an oral immune activator that inflames the tumor microenvironment, enhancing the activity of immunotherapies like pembrolizumab. Preliminary findings from a phase 2 clinical trial showed promising results, with some patients experiencing stable disease and significant reductions in cancer markers.
- Botensilimab: Botensilimab is an immunostimulator designed to optimize interactions between T cells and antigens, promoting a stronger immune response. It is currently in a phase 2 clinical trial to assess its efficacy in combination with standard chemotherapy for metastatic pancreatic cancer.
- Chimeric Antigen Receptor (CAR) T-Cell Therapy: CAR T-cell therapy involves reprogramming a patient’s T cells to target specific antigens on cancer cells. Potential targets for pancreatic cancer include CEA, mesothelin, ROR1, EpCAM, HER2, and MUC1 ( genes that encode proteins involved in cell adhesion, signaling, and growth). This approach is still in the experimental stage for pancreatic cancer.
- Cancer Vaccines: Cancer vaccines like GVAX and GV1001 aim to stimulate the immune system to recognize and attack pancreatic cancer cells. These vaccines are designed to present tumor-specific antigens to the immune system, thereby enhancing the anti-tumor response. They are currently being tested in clinical trials.
- Oncolytic Virus Therapy: Oncolytic viruses are engineered to selectively infect and kill cancer cells while stimulating an immune response. This approach is being explored in combination with other immunotherapies to enhance their efficacy against pancreatic cancer.
More information about completed and ongoing clinical trials for colorectal cancer can be found here – clinicaltrials.gov
The video created by The New England Journal of Medicine presented the use of adoptive immunotherapy with T-cell receptor (TCR) – -engineered T cells in a patient with pancreatic cancer.
Side Effects of Immunotherapy
While immunotherapy has shown promising results in the treatment of various cancers, it can also cause a range of side effects. These side effects are often different from those associated with traditional cancer therapies and can affect various organ systems. Some common side effects of immunotherapy include:
- Fatigue: The most common side effect, which can range from mild to severe. Management includes balancing rest and activity, maintaining a nutritious diet, and consulting a mental health expert if needed.
- Skin Reactions: Includes rash, itchiness, redness, blistering, and sensitivity to sunlight. Management involves using moisturizers, avoiding sun exposure, and consulting a dermatologist for severe cases.
- Flu-like Symptoms: Fever, chills, weakness, dizziness, muscle or joint aches, and headache. Management includes staying hydrated, using cold compresses for fever, and seeking medical advice for persistent symptoms.
- Gastrointestinal Issues: Diarrhea, nausea, vomiting, and colitis (inflammation of the colon). Management involves staying hydrated, following a bland diet, and using medications as prescribed for nausea and diarrhea.
- Endocrine Disorders: Thyroid dysfunction, adrenal insufficiency, and hypophysitis (inflammation of the pituitary gland). Management may include hormone replacement therapy for conditions like hypothyroidism and adrenal insufficiency.
- Respiratory Issues: Pneumonitis (inflammation of the lungs), which can cause cough and shortness of breath. Immediate medical attention is required for symptoms of pneumonitis, and treatment may include corticosteroids.
- Hepatitis: Inflammation of the liver, which can lead to elevated liver enzymes and jaundice.
- Cardiac Issues: Myocarditis (inflammation of the heart muscle) and arrhythmias.
- Neurological Issues: Encephalitis (inflammation of the brain), neuropathy, and myasthenia gravis.
- Renal Issues: Nephritis (inflammation of the kidneys), which can lead to kidney dysfunction.
It is crucial for patients receiving immunotherapy to be closely monitored for these side effects, and prompt management by healthcare professionals is essential to mitigate the risks and ensure patient safety.
FAQs
Who is eligible for pancreatic cancer immunotherapy?
Eligibility for pancreatic cancer immunotherapy typically depends on specific genetic markers and the stage of the disease. Patients whose tumors exhibit high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR) are more likely to benefit from immunotherapy.
Additionally, patients with certain genetic mutations, such as BRCA or RAD51C, may also respond well to immunotherapy. Immunotherapy is generally considered for patients with unresectable pancreatic cancer, those whose cancer has recurred after treatment, or those who cannot tolerate chemotherapy. Molecular profiling of the tumor is often recommended to determine eligibility for immunotherapy.
How long does immunotherapy work for pancreatic cancer?
The duration of effectiveness of immunotherapy for pancreatic cancer can vary. In a study involving patients with refractory pancreatic cancer, immunotherapy resulted in improved overall survival. Another study reported improved survival for stage IV pancreatic cancer patients treated with immunotherapy, compared to those receiving standard care. However, findings in those studies suggest that while immunotherapy can extend survival in some patients, the overall duration of effectiveness remains limited, particularly in advanced stages of the disease.
Sources
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- American Society of Clinical Oncology – asco.org
- Cancer Research UK – canceresearchuk.org
- Immunotherapy for Pancreatic Cancer – Pancreatic Cancer Action Network
- Immunotherapy for pancreatic cancer – World Journal of Clinical Cases
- The Role of Immunotherapy in Pancreatic Cancer – Current Oncology
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
