What is Glucagonoma?
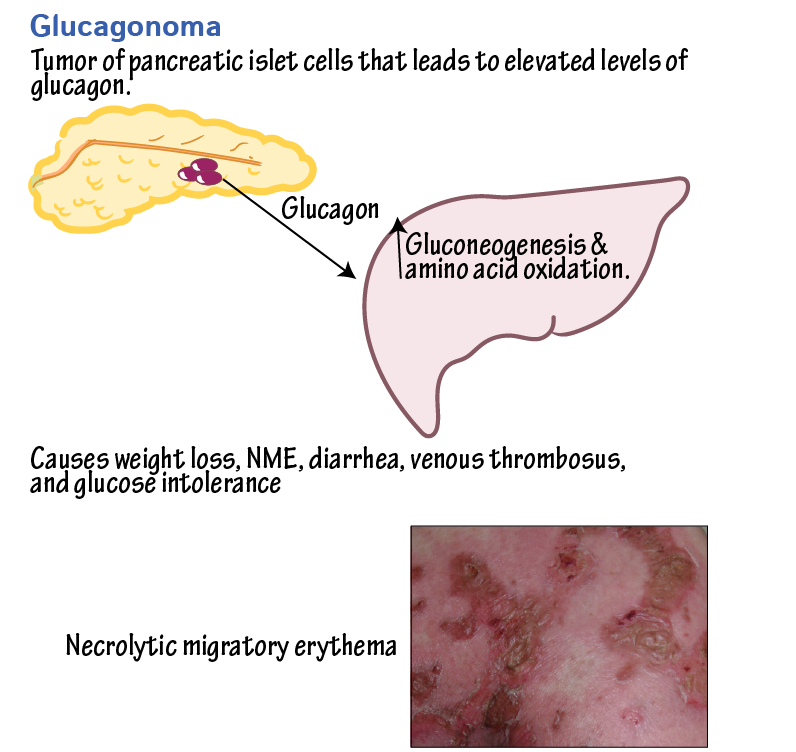
Glucagonoma is a rare neuroendocrine tumor that originates from the pancreatic alpha cells and results in the overproduction of the hormone glucagon. This condition leads to a constellation of symptoms known as glucagonoma syndrome, which includes necrolytic migratory erythema (NME), diabetes mellitus, anemia, weight loss, glossitis, cheilitis, steatorrhea, and diarrhea. Glucagonomas are typically solitary tumors, with less than 10% associated with multiple endocrine neoplasia 1 syndrome (MEN1).
This image is taken from ditki.com
Epidemiology and Risk Factors of Glucagonoma
The exact causes of glucagonoma are currently unknown, but some risk factors have been identified as follows:
Genetic Factors
- Having family members with multiple endocrine neoplasia type 1 (MEN1) syndrome is a risk factor for developing glucagonoma.
- Mutations in the glucagon receptor gene (GCGR), as seen in Mahvash disease, can also increase the risk of glucagonoma.
Demographics
- Women are slightly more likely to develop glucagonoma compared to men.
- The condition is typically diagnosed in patients in their early 50s.
Other Factors
- Glucagonoma is an extremely rare condition, with an estimated annual incidence of 1 case per 20 million population.
- About 60% of diagnosed cases are in women.
In summary, while the exact causes of glucagonoma remain unknown, having a family history of MEN1 syndrome or Mahvash disease, being female, and being in one’s 50s are the main risk factors identified so far. However, the rarity of the condition makes it difficult to establish definitive causal relationships.
Symptoms of Glucagonoma
The most common symptoms include:
Skin Rash
A painful skin rash called necrolytic migratory erythema (NME) is a hallmark symptom of glucagonoma syndrome, affecting about 90% of patients. The rash typically starts with small circles of redness that develop into itchy, painful blisters and can affect various parts of the body, including the buttocks, groin, back passage, genitals, and lower legs.

Necrolytic migratory erythema. This image is taken from researchgate.net
Weight Loss
Weight loss is another common symptom, with more than 90% of patients experiencing significant weight loss despite not dieting. This weight loss can be severe and is often accompanied by other symptoms like diabetes and skin rash.
Diabetes
Glucagonoma syndrome can lead to high blood sugar levels, causing symptoms similar to those of diabetes, such as thirst, frequent urination, weakness, and weight loss. Between 40 and 90% of patients with glucagonoma syndrome develop diabetes.
Mouth Ulcers
Mouth ulcers are a common symptom, affecting between 30 and 40% of patients. These ulcers can cause pain or discomfort and are often accompanied by other symptoms like skin rash and weight loss.
Diarrhea
Diarrhea is another symptom, affecting about 15% of patients. This can lead to dehydration and electrolyte imbalance if left untreated.
Blood Clots
Blood clots, particularly deep vein thrombosis (DVT), are a significant complication of glucagonoma syndrome, affecting about 50% of patients. DVT can lead to pulmonary embolism, which can be fatal if not treated promptly.
Mood Changes
Mood changes, including depression and agitation, are common among patients with glucagonoma syndrome. Depression is the most common mental health issue, affecting about 50% of patients.
Anemia
Anemia, or low levels of red blood cells, is another symptom, affecting up to 80% of patients. Anemia can cause fatigue, weakness, and shortness of breath.
In summary, the symptoms of glucagonoma syndrome are diverse and can affect various aspects of a patient’s health, including the skin, weight, blood sugar levels, digestive system, mental health, and blood clotting.
Diagnosis of Glucagonoma
Glucagonoma syndrome is diagnosed through a combination of clinical evaluation, laboratory tests, and imaging studies. The diagnosis involves satisfying specific criteria, including:
- Demonstration of a tumor mass: Direct visualization or radiographic techniques are used to confirm the presence of a tumor mass
- Proof of glucagon-containing cells: Appropriate staining and proof of increased tissue levels of immunoreactive glucagon are used to confirm that the tumor contains glucagon-producing cells
- Elevation of basal circulating immunoreactive glucagon: Blood tests are used to measure the levels of glucagon in the blood, which are typically elevated in glucagonoma syndrome
- Coincidental findings: At least one of the following coincidental findings must be present: skin rash, glucose intolerance, or hypoaminoacidemia
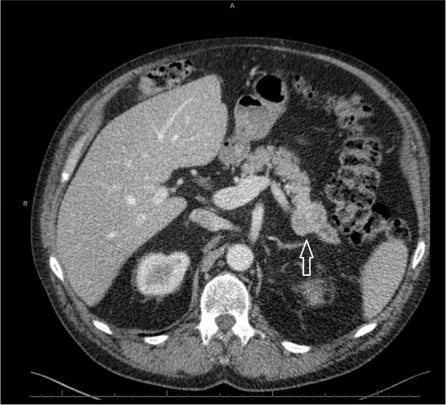
CT scan demonstrating a pancreatic neuroendocrine tumor. This image is taken from sciencedirect.com.
Laboratory Tests
Blood tests are used to check for elevated glucagon levels, as well as other substances that may be raised in neuroendocrine tumors (NETs). These tests can also help rule out other conditions that may cause similar symptoms.
Imaging Studies
Imaging tests such as CT scans, MRI scans, and radioactive scans (e.g., octreotide scans or gallium PET scans) are used to visualize the tumor and determine its size and location. These tests can also help identify if the tumor has spread to other parts of the body.
Endoscopy and Biopsy
Endoscopy and biopsy may be performed to examine the inside of the digestive tract and obtain tissue samples from any abnormal areas. This can help confirm the diagnosis and rule out other conditions.
Clinical Evaluation
A thorough clinical evaluation is essential to identify the symptoms and signs of glucagonoma syndrome, such as necrolytic migratory erythema (NME), diabetes, weight loss, and other associated symptoms.
In summary, the diagnosis of glucagonoma syndrome involves a combination of clinical evaluation, laboratory tests, and imaging studies to confirm the presence of a glucagon-producing tumor and rule out other conditions.
Treatment of Glucagonoma
The treatment of glucagonoma syndrome involves a multidisciplinary approach, including surgical resection, medical therapy, and supportive care. The primary goal of treatment is to manage symptoms, control tumor growth, and improve quality of life.
Surgical Resection
Surgical resection is the definitive treatment for glucagonoma syndrome, offering the only chance for a cure. The surgical approach typically involves distal pancreatectomy, peripancreatic lymphadenectomy, and splenectomy. Resection of metastases and the primary tumor is recommended if complete resection is possible.
Medical Therapy
Medical therapy plays a crucial role in managing symptoms and controlling tumor growth. Somatostatin analogs (SSAs), such as octreotide and lanreotide, are the mainstay of medical treatment. These medications can help control symptoms, reduce glucagon levels, and improve the rash associated with glucagonoma syndrome. Chemotherapeutic agents, such as streptozotocin and doxorubicin, may be used in combination with SSAs to treat advanced disease.
Supportive Care
Supportive care is essential to manage the various symptoms associated with glucagonoma syndrome. This includes providing a supplemental protein supply to furnish amino acids, which can be administered intravenously in severe cases. Ingestion of essential fatty acids, zinc, vitamins, and minerals is also helpful. Antibiotics, corticosteroids, amino acids, and zinc supplementation may improve severe skin rash. Prophylaxis for venous thrombosis, including the subcutaneous administration of low-dose heparin, is mandatory for all patients during the perioperative period.
Other Therapies
Other therapies, such as peptide receptor radionuclide therapy (PRRT) with lutetium Lu 177-dota-tate (177Lu-DOTATATE; Lutheran), have been proposed as a first-line therapy in patients with glucagonoma and secreting metastasis. Hepatic artery catheterization for infusion of doxorubicin, cisplatin, and mitomycin-C may be considered in patients with widespread metastases. Embolization of liver metastases may also be beneficial in selected patients
Follow-up and Consultations
Given the risk of recurrence, even patients with completely resected glucagonomas require close follow-up, especially in the first 3 years after resection. Guidelines suggest maintaining follow-up for at least 10 years in most cases. Consultations with dermatologists, neurologists, endocrinologists, and ophthalmologists may be very helpful for differential diagnosis and therapy.
In summary, the treatment of glucagonoma syndrome involves a multidisciplinary approach, including surgical resection, medical therapy, and supportive care. The primary goal of treatment is to manage symptoms, control tumor growth, and improve quality of life.
Prognosis and Survival
The prognosis and survival rates for glucagonoma depend on several factors, including the stage and grade of the tumor at diagnosis, whether it has spread to other parts of the body, and the overall health of the patient.
Survival Rates
- For people with glucagonomas that have not spread and can be surgically removed, the 10-year survival rate is almost 100%.
- People with cancers from glucagonomas that have spread to other body parts have about a 50% chance of living 10 years after diagnosis.
- An international study that looked at 407 people diagnosed with glucagonoma found that around 65 out of 100 people (around 65%) with glucagonoma and diabetic-teratogenic syndrome (DDS) survive their disease for 10 years or more.
- For those with glucagonoma and DDS that have not spread to other parts of the body, about 100 out of every 100 people (100%) survive.
- For those with glucagonoma and DDS that have spread to other parts of the body, more than 50 out of every 100 people (more than 50%) survive.
Factors Affecting Survival
- The stage of the tumor at diagnosis is a key factor, with earlier-stage tumors having a better prognosis.
- Tumors that are contained within the pancreas and can be surgically removed typically have a good outlook, but this represents only about 20% of glucagonoma cases.
- Metastatic disease, where the cancer has spread to other organs like the liver, is associated with a poorer prognosis. Overall health and response to treatment also impact survival.
In summary, while glucagonomas are slow-growing tumors, their prognosis depends on the stage at diagnosis and whether they have spread to other organs. Early diagnosis and treatment, particularly surgical removal of localized tumors, offer the best chance for long-term survival.
Challenges and Considerations
The main challenges and considerations in managing glucagonoma include:
Rarity and Lack of Data
Glucagonomas are extremely rare, with an estimated annual incidence of only 1 case per 20 million population. Due to the rarity of the condition, there is limited data available to accurately predict survival rates and outcomes, especially for metastatic disease.
Nonspecific Symptoms
The symptoms of glucagonoma syndrome, such as weight loss, diabetes, and skin rash, can be nonspecific and similar to other more common conditions. This can lead to delayed diagnosis, as the condition may not be suspected initially.
Metastatic Disease
Around 50% of glucagonomas have metastasized by the time of diagnosis. Metastatic disease, particularly in the liver, is associated with a poorer prognosis compared to localized tumors that can be surgically removed.
Genetic Factors
Having a family history of multiple endocrine neoplasia type 1 (MEN1) syndrome is a risk factor for developing glucagonoma. Genetic testing can help identify individuals at risk, but the rarity of the condition makes it challenging to implement widespread screening programs.
Treatment Challenges
While surgical resection is the definitive treatment for localized glucagonomas, many patients present with metastatic disease that is not amenable to complete resection. In these cases, treatment often involves a combination of medical therapies, such as somatostatin analogs and chemotherapy, which have limited efficacy.
Psychological Impact
The diverse symptoms of glucagonoma syndrome, including skin rash, weight loss, and mental health issues like depression, can have a significant impact on a patient’s quality of life. Providing comprehensive support and access to mental health resources is crucial for managing the psychological burden of this rare condition.
During Treatment
Common side effects include:
During treatment for glucagonoma, some common side effects may include:
- Injection Site Reactions – Injection site reactions can occur at the site where medications like octreotide are administered. These reactions may include redness, swelling, pain, or itching at the injection site.
- Nausea and Vomiting – Nausea and vomiting are common side effects that may occur after treatment with medications like GlucaGen. These side effects usually ease quickly.
- Headache – Headache is another common side effect reported with GlucaGen treatment.
- Dizziness, Drowsiness, and Lack of Energy – Mild side effects like dizziness, drowsiness, and lack of energy have been reported with GlucaGen.
- Temporary Changes in Blood Pressure or Heart Rate – GlucaGen may cause a temporary increase or decrease in blood pressure or heart rate in some patients.
- Diarrhea – Chronic diarrhea can occur in about 15% of patients with glucagonoma syndrome.
It’s important to note that not everyone will experience these side effects, and the severity can vary. If side effects persist, worsen, or become bothersome, patients should consult with their healthcare provider. Prompt management of side effects is crucial to ensure the best possible outcome during glucagonoma treatment.
After Treatment
Follow-up Care
After treatment for glucagonoma, patients require close follow-up care to monitor for recurrence and manage any ongoing symptoms or complications. Here are some key points about follow-up care:
Monitoring for Recurrence
- Even patients with completely resected glucagonomas require close follow-up, especially in the first 3 years after resection․
- Guidelines suggest maintaining follow-up for at least 10 years in most cases
- Regular imaging tests like CT scans, MRI scans, and octreotide scans are used to check for tumor recurrence or metastases․
Managing Symptoms and Complications
- Patients may require ongoing treatment with somatostatin analogs like octreotide or lanreotide to control symptoms and slow tumor growth
- Blood sugar levels need to be closely monitored and managed with medications if needed
- Skin rashes may require treatment with amino acid infusions, corticosteroids, antibiotics, and zinc supplementation
- Prophylaxis for venous thrombosis with low-dose heparin is mandatory during the perioperative period
Supportive Care
- Patients may require supplemental protein, essential fatty acids, vitamins, and minerals to address nutritional deficiencies
- Consultations with dermatologists, neurologists, endocrinologists, and ophthalmologists may be helpful for managing various aspects of glucagonoma syndrome
Psychological Support
- The diverse symptoms and impact of glucagonoma syndrome can take a toll on mental health
- Access to counseling and support resources is important for helping patients cope with the condition.
In summary, the recommendations for patients with glucagonoma syndrome include managing symptoms, considering surgical resection, utilizing medical therapies like somatostatin analogs, ensuring close follow-up care, providing supportive care, and seeking consultations with various specialists for comprehensive management.
References
- Journal of Medical Case Reports – jmedicalcasereports.biomedcentral.com
- Cancer Research UK – cancerresearchuk.org
- The glucagonoma syndrome. Clinical and pathologic features in 21 patients – PubMed
- National Cancer Institute – cancer.gov
- Canadian Cancer Society – cancer.ca
- Johns Hopkins Medicine – hopkinsmedicine.org
- American Society of Clinical Oncology (ASCO) – Cancer.net
- American Cancer Society – cancer.org
- Oncodaily.com