The Human Expertise of Medical Physics: Beyond the Radiotherapy Machine
Medical physics is an applied science that utilizes the principles, methods, and techniques of physics to enhance human health through the prevention, diagnosis, and treatment of diseases. From the initial discovery of X-rays and radioactivity in the 1890s, physicists have been instrumental in developing crucial diagnostic tools like MRI and CT scans, as well as pioneering life-saving treatments such as radiation therapy. This field continues to evolve, with medical physicists playing a vital role in ensuring the precision, safety, and effectiveness of cutting-edge medical technologies and patient care.
Who Are Medical Physicists?
Medical physicists are highly skilled healthcare professionals uniquely trained to bridge the gap between physics and medicine. They possess specialized education in applying the fundamental principles and intricate physics techniques directly to patient care. Their expertise is crucial in various medical applications, including high-energy radiation (like X-rays), ultrasound, magnetic and electric fields, and even infrared and ultraviolet light for both diagnostic imaging and therapeutic interventions.
These professionals work within hospitals, dedicated cancer treatment facilities, and hospital-based research establishments. However, their skills are also sought in universities, government bodies, and the medical industry. As integral members of the healthcare team, medical physicists collaborate closely with physicians, nurses, and technologists to ensure that advanced medical equipment and radiation treatments are not only precisely calibrated and operating safely but also effectively tailored to each patient’s specific needs, ultimately enhancing the quality and safety of healthcare delivery.
Historical Overview of Medical Physics
As we understand it today, medical physics traces its origins back to the late 19th century with pivotal scientific discoveries. The field started to form after Wilhelm Conrad Roentgen, a physicist, made the monumental discovery of X-rays in the 1890s, an accomplishment for which he was awarded the first Nobel Prize in Physics in 1901.
From its inception, physics was intimately involved in diagnostic and therapeutic applications. Physics was central to developing early radiotherapy treatments and protocols, with titles like “radiation physicist” highlighting their significance. These pioneering physicists included the Canadian physicist Harold Johns, who developed the first Cobalt Therapy Unit in the late 1940s and treated the first patient with the Cobalt Machine in 1951.
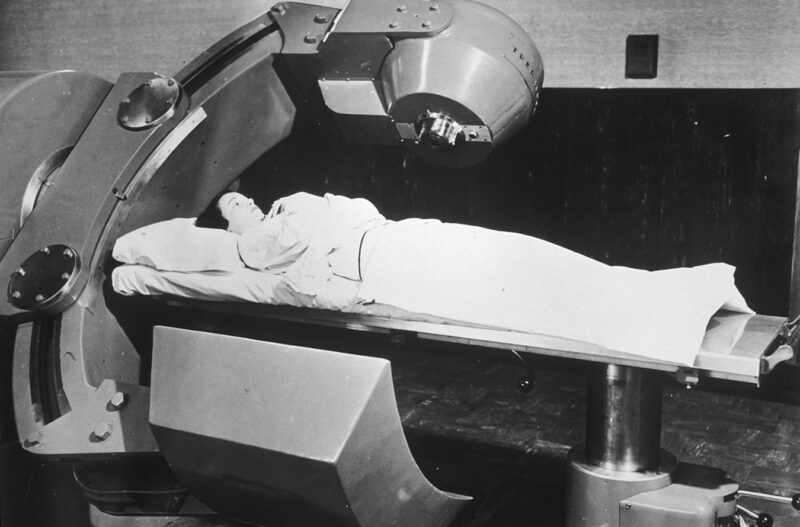
Patient Recieving Co-60 Radiation Therapy (1951)
source: www.visualsonline.cancer.org
Initially, physicists were comprehensively involved in all aspects of treatment planning, often performing manual calculations to configure beams and determine doses. This hands-on approach, though time-consuming and challenging given the era’s technological limitations, fostered a deep understanding of radiation interaction with body tissues and the limitations of early dose calculation algorithms. As technology advanced, particularly with the advent of computerized planning systems, the methods evolved, yet the foundational role of physicists in ensuring the precision and safety of medical radiation applications remained integral to the progress of healthcare.
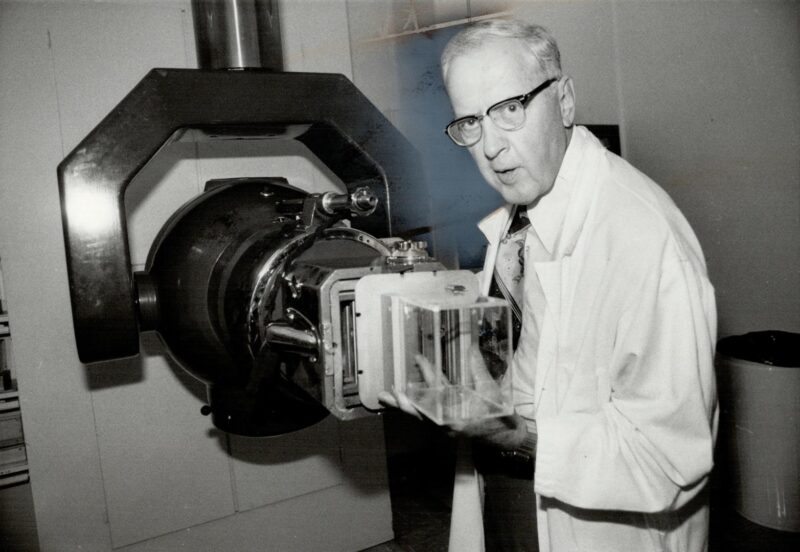
source: www. digitalarchive.tpl.ca
What Are The Core Activities Of Medical Physicists?
Medical physicists undertake a wide range of essential duties, fundamentally applying the principles of physics to healthcare. Their responsibilities generally fall into three key domains: clinical service and consultation, research and development, and teaching.
In their clinical service and consultation role, medical physicists are integral to the direct care of patients. A primary responsibility in radiotherapy involves designing individualized radiation treatment plans for cancer patients. They meticulously use advanced computer calculations and imaging techniques, such as CT and MRI scans, to precisely outline tumor volumes and plan radiation beams. The goal is always to deliver the most effective dose to the cancer while meticulously minimizing exposure to healthy surrounding tissues, a process that applies to both external radiation treatments and internal brachytherapy.
Beyond planning, they are crucial for managing all radiotherapy and diagnostic imaging equipment, including linear accelerators, CT scanners, and MRI machines. This comprehensive management involves calibrating equipment for accurate dose delivery, performing rigorous daily, monthly, and yearly quality assurance (QA) checks, implementing preventative maintenance programs, and overseeing the acceptance testing and commissioning of new technologies. They are also the go-to experts for troubleshooting and diagnosing faults in complex medical devices.
Furthermore, medical physicists provide vital radiation safety and protection services for both patients and staff, developing new safety procedures, ensuring the secure handling and disposal of radioactive materials, and planning facility shielding. In diagnostics, they analyze nuclear medicine image data to derive important physiological information, such as metabolic rates or blood flow. Crucially, they collaborate closely within multidisciplinary teams, including radiation oncologists, radiation therapists, and nurses, offering their specialized scientific and technical advice to enhance treatment outcomes.
Within research and development, medical physicists are at the forefront of innovation. They conduct foundational theoretical studies to explore new diagnostic and treatment concepts. A significant part of their work involves the integration of new technologies: they develop, test, and implement novel medical equipment, creating standard operating procedures and providing essential training to staff on its safe and effective use. They actively participate in and often lead clinical trials for new imaging and treatment techniques. Additionally, a specialized subgroup focuses on developing and refining complex algorithms that power the advanced computerized planning systems.
Finally, in their teaching capacity, medical physicists are instrumental in shaping the future of the field. Many are affiliated with universities, where they instruct students in graduate and undergraduate medical physics programs. They provide hands-on clinical supervision and training for aspiring medical physicists, dosimetrists, and radiotherapy technologists. They also play a key role in educating other medical staff, including radiology and oncology residents and medical students, on critical medical physics principles and radiation safety.
In essence, medical physicists serve as the indispensable scientific and technical foundation within departments utilizing radiation and advanced imaging. Their expertise ensures that every diagnostic procedure and treatment is executed with the highest degree of precision, safety, and effectiveness, directly benefiting patient care.
Education and Training of Medical Physicists
Historically, individuals pursuing a career as a medical physicist typically graduated from university programs, often five-year degrees, in pure physics. These programs sometimes included an emphasis on medical applications or radiation physics, equipping graduates with extensive theoretical physics knowledge before they joined a medical physics team for specialized training.
However, the educational landscape has evolved significantly. In Europe, the implementation of the Bologna Agreement restructured higher education into Bachelor’s and Master’s degrees, which can impact the foundational physics training. While it theoretically allows students with a Bachelor’s degree in a related field (like engineering) to pursue a Master’s in Physics or Medical Physics, it raises questions about the consistency of their physics background compared to earlier generations who completed longer, integrated physics degrees. Recognizing this, organizations like the European Federation of Organizations for Medical Physics (EFOMP) have issued clear guidelines recommending a three-step pathway: a Bachelor’s degree in foundational sciences, followed by a Master’s degree specifically in medical physics, and then a postgraduate residency program in a hospital.
In the United States, the pathway to becoming a clinical medical physicist is also rigorously defined, with a strong emphasis on accreditation. The typical route involves:
- Undergraduate Degree: A Bachelor’s degree, usually in physics or a related natural science, physical science, mathematics, or engineering, with a strong physics background.
- Graduate Degree: Completion of a Master’s (MS) or Doctoral (PhD/DMP – Doctor of Medical Physics) degree in medical physics from a program accredited by the Commission on Accreditation of Medical Physics Education Programs (CAMPEP). CAMPEP accreditation is a crucial standard ensuring high-quality courses, instructors, and facilities
- Graduate Degree: Completion of a Master’s (MS) or Doctoral (PhD/DMP – Doctor of Medical Physics) degree in medical physics from a program accredited by the Commission on Accreditation of Medical Physics Education Programs (CAMPEP). CAMPEP accreditation is a crucial standard ensuring high-quality courses, instructors, and facilities.
- Clinical Residency: Following the graduate degree (or integrated into a DMP program), a CAMPEP-accredited residency program, typically two years, is required. This hands-on training under the supervision of experienced medical physicists is essential for gaining practical clinical competency.
- Board Certification: After completing the accredited graduate program and residency, aspiring medical physicists seek board certification, commonly through the American Board of Radiology (ABR) or the American Board of Medical Physics (ABMP). This certification involves a series of rigorous examinations (written and oral) to validate expertise in a chosen specialty (e.g., therapeutic, diagnostic, or nuclear medical physics). While most US states register rather than license medical physicists, ABR or ABMP certification is widely recognized and often a prerequisite for clinical practice.
Both European and US systems stress the importance of a strong physics foundation and extensive clinical postgraduate training. Documents from bodies like the European Commission (EC) define key competencies for a Medical Physics Expert (MPE), particularly highlighting safety-related aspects. However, some variation in specific requirements across countries still exists, and the ongoing need for continuing professional development is universally recognized to keep pace with rapidly evolving technologies and maintain expertise throughout a medical physicist’s career.
Read OncoDaily’s Special Article About Radiation Oncologists
Research In Medical Physics
Medical physics applies physics principles to enhance human health through diagnosis, prevention, and treatment of diseases. Originating with X-rays in the 1890s and evolving through pioneers like Harold Johns, medical physicists are specialized healthcare professionals, primarily hospital-based.
Their work involves three core areas: clinical service, where they precisely plan radiation treatments for cancer, manage and calibrate medical equipment for safety and accuracy, and ensure radiation protection; research and development, where they innovate new diagnostic and therapeutic techniques, test equipment, and lead clinical trials; and teaching, educating future medical professionals.
Becoming a medical physicist typically requires an accredited Master’s or Doctoral degree in medical physics followed by a rigorous clinical residency. This comprehensive education ensures they possess the expertise to apply physics with precision, safety, and effectiveness in patient care.
Written By Aren Karapetyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
