Gastric Cancer and Smoking — What Are the Shocking Real Risks?
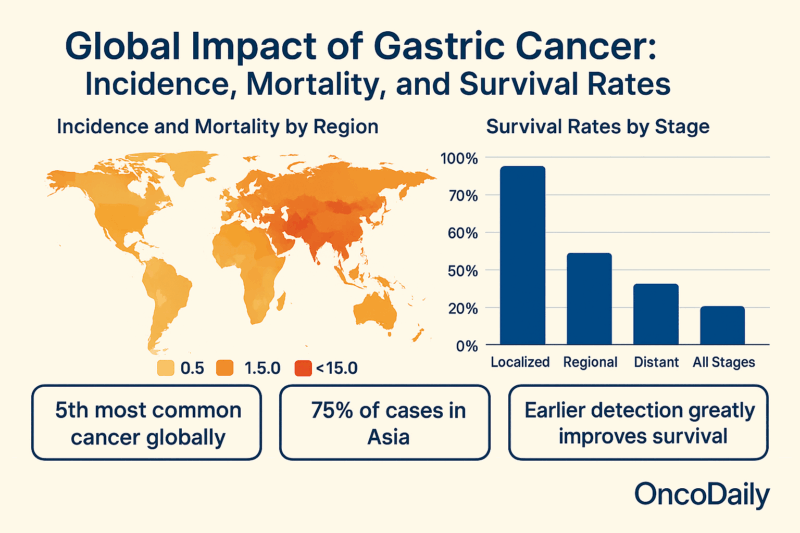
Gastric cancer, also known as stomach cancer, remains a major global health challenge despite gradual declines in its incidence and mortality in recent decades. In 2020 alone, approximately 1.1 million new cases were diagnosed worldwide, making it the fifth most common malignancy, while nearly 800,000 deaths placed it as the fourth leading cause of cancer-related mortality.
The disease disproportionately affects populations in Asia, which accounts for over 75% of new cases and deaths, and is more common in men, with incidence rates roughly double those in women. Survival rates remain poor, with a global five-year survival rate below 20%, and significant geographic variations persist, reflecting differences in risk factors, healthcare access, and screening practices.
Histological image of gastric adenocarcinoma. Photo: Depositphotos
Smoking is a well-established risk factor for gastric cancer, with the risk increasing alongside the duration and intensity of tobacco use.
This article focuses on examining the real risks of gastric cancer and smoking .We will understand the relationship between smoking and gastric cancer is crucial for targeted prevention strategies and for reducing the global burden of this deadly disease.
Understanding Gastric Cancer
Gastric (stomach) cancer remains a significant global health concern. In 2022, there were approximately 968,000 new cases diagnosed worldwide, making it the fifth most common cancer. The disease also ranks as the fifth leading cause of cancer-related deaths globally, with an estimated 660,000 deaths in the same year. In the United States, about 30,300 new cases are expected in 2025, accounting for roughly 1.5% of all new cancer diagnoses each year, and around 10,780 deaths are projected from stomach cancer.
Survival rates for gastric cancer remain relatively low. In the United States, the overall five-year relative survival rate is 36.4%. This rate varies significantly depending on the stage at diagnosis: if the cancer is localized to the stomach, the five-year survival rate is 75.4%; if it has spread to regional lymph nodes, the rate drops to 35.8%; and if it has metastasized to distant organs, the survival rate is just 7.0%. In China, the overall five-year survival rate is 33.5%, with stage-specific rates ranging from 85.1% for stage I to 13.2% for stage IV.
Countries with robust screening programs, such as Japan and South Korea, report higher five-year survival rates of 54% and 57.9%, respectively. These statistics highlight the substantial burden of gastric cancer and the critical importance of early detection and effective treatment strategies. Elizabeth C Smyth, ScienceDirect 2020.
Gastric Cancer and Smoking — Understanding the True Risk Factors
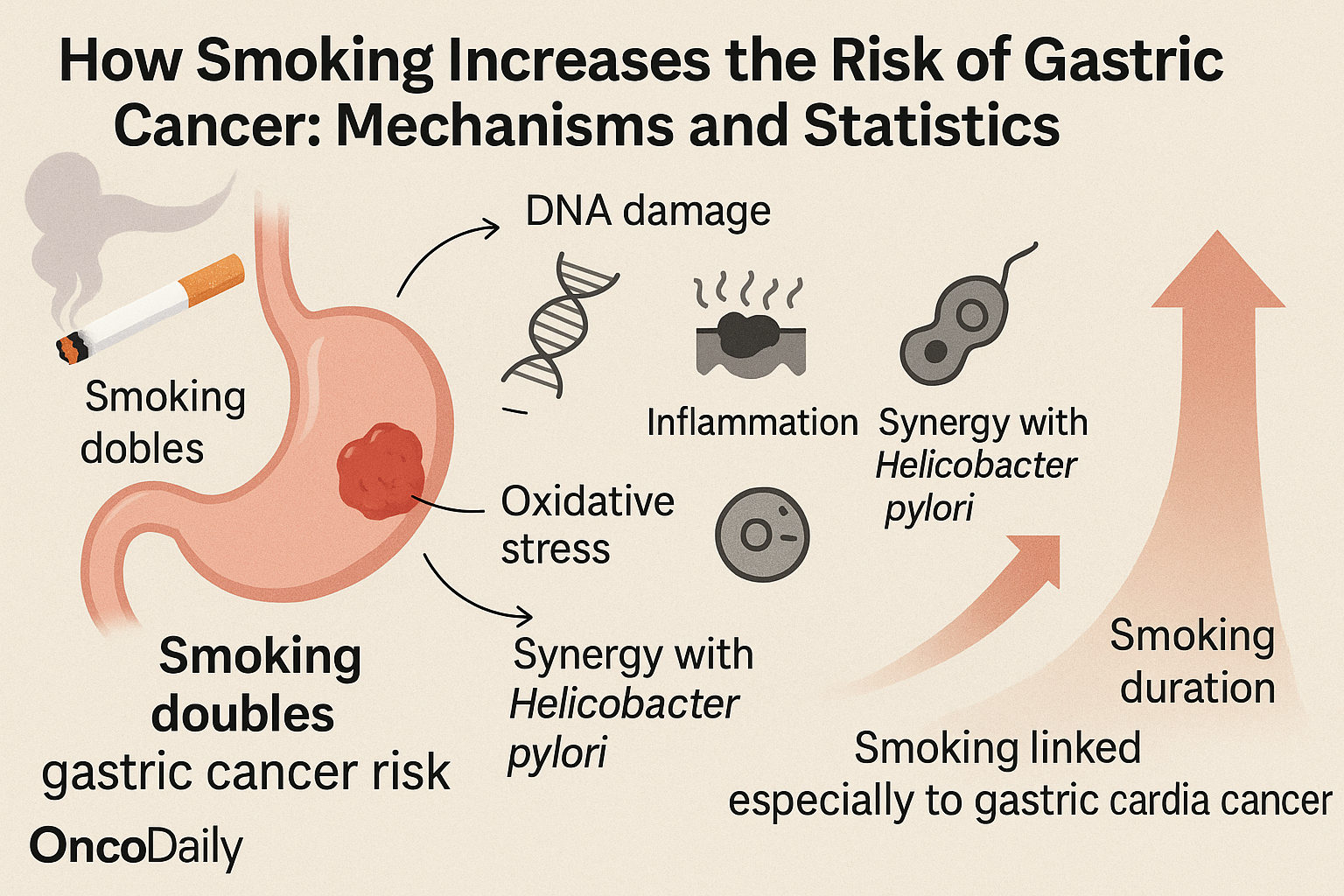
The relationship between smoking and gastric (stomach) cancer is well-established, with smoking recognized as a significant risk factor that notably increases the likelihood of developing this malignancy. Research indicates that smoking approximately doubles the risk of stomach cancer, particularly affecting the upper part of the stomach near the esophagus, known as the gastric cardia. Globally, smoking is attributed to about 11% to 20% of stomach cancer cases, highlighting its substantial contribution to the disease burden.
The risk of gastric cancer rises with the intensity and duration of tobacco use. Studies show a clear dose-response relationship: the more cigarettes smoked per day, the longer the years of smoking, and the younger the age at which smoking begins, the higher the risk. For example, heavy smokers—those with higher pack-years (a measure combining the number of packs smoked per day and years smoked)—face significantly greater risk compared to light or moderate smokers. Even former smokers with a history of heavy smoking retain an elevated risk, underscoring the lasting impact of tobacco exposure.
A large Korean cohort study involving nearly 100,000 men demonstrated that current smokers had the highest hazard ratios for gastric cancer compared to never smokers, with risk increasing in a dose-dependent manner according to pack-years. Former smokers who had smoked heavily also showed a significant increase in risk, emphasizing that quitting smoking reduces but does not entirely eliminate risk, especially for those with substantial prior tobacco exposure. This study adjusted for other factors such as age, body mass index, alcohol intake, and physical activity, strengthening the evidence for smoking as an independent risk factor. Sung Keun Park, Epidemiology and Health 2022.
Current smokers had nearly double the risk compared to never smokers, with consistent findings across ethnic groups and both sexes. The risk was particularly pronounced for gastric cardia cancer compared to distal gastric cancer, and a stronger association was observed for the intestinal histologic subtype of gastric cancer. Former male smokers also exhibited increased risk, although this was less clear among females.
The global burden of stomach cancer attributable to smoking is especially high in East Asia, where age-standardized rates of mortality and disability-adjusted life years (DALYs) due to smoking-related gastric cancer remain elevated, despite some declines in recent decades. This regional disparity reflects higher smoking prevalence and other environmental and genetic factors in these populations. Kaijuan Wang, ScienceDirect 2024.
While smoking is a critical behavioral risk factor, it often acts synergistically with other factors such as Helicobacter pylori infection, a major cause of gastric cancer. Smoking can exacerbate the carcinogenic effects of H. pylori, although some studies lack data on infection status, which is a limitation in fully understanding the combined risk.
How Smoking Causes Stomach Cancer?
Gastric cancer pathogenesis involves a complex interplay of environmental factors—such as tobacco smoke—and genetic alterations that disrupt normal cellular regulation. Tobacco smoke contains carcinogens like polycyclic aromatic hydrocarbons (PAHs), tobacco-specific nitrosamines (TSNAs), and heavy metals that induce DNA damage in gastric epithelial cells. These carcinogens form DNA adducts, leading to mutations in oncogenes and tumor suppressor genes, which initiate malignant transformation.
Nicotine, although not directly mutagenic, promotes tumor progression by activating nicotinic acetylcholine receptors (nAChRs) and β-adrenergic receptors on gastric cells. This activation triggers intracellular signaling cascades including the extracellular signal-regulated kinase (ERK) pathway, which increases expression of cyclooxygenase-2 (COX-2) and vascular endothelial growth factor (VEGF). Elevated COX-2 promotes inflammation and prostaglandin synthesis, while VEGF stimulates angiogenesis, both facilitating tumor growth and metastasis.
Smoking-induced oxidative stress generates reactive oxygen species (ROS), which cause further DNA damage and promote chronic inflammation in the gastric mucosa. This inflammatory microenvironment supports carcinogenesis by enhancing cell proliferation and inhibiting apoptosis (programmed cell death).
Moreover, smoking exacerbates Helicobacter pylori-induced gastric injury. Both smoking and H. pylori infection activate overlapping molecular pathways, amplifying mucosal damage, inflammation, and genetic instability. This synergistic effect significantly increases the risk of gastric cancer, particularly non-cardia types. Waku Hatta, MDPI 2024.
You Can Also Read Does Vaping Cause Lung Cancer? Myths and Facts by Oncodaily

How Does Quitting Smoking Affect the Risk of Gastric Cancer?
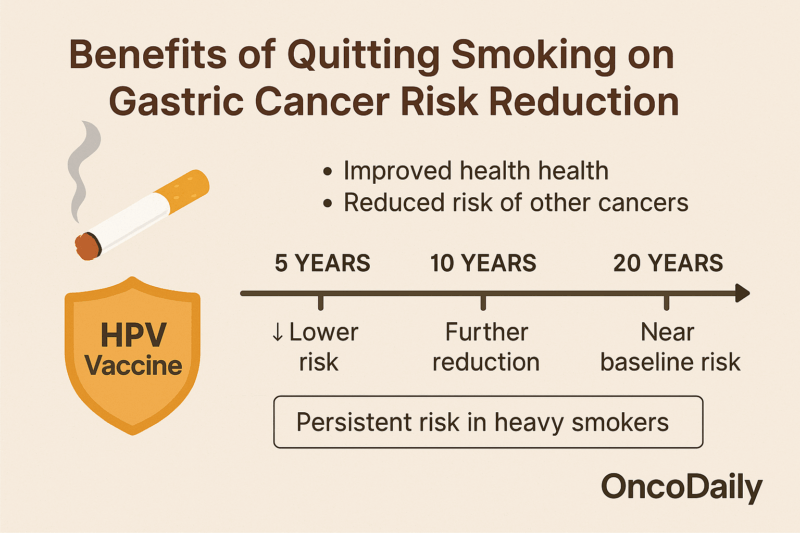
Quitting smoking leads to a significant reduction in the risk of developing gastric (stomach) cancer compared to continuing smokers. Numerous epidemiological studies have demonstrated that former smokers have a substantially lower risk than current smokers, reflecting the body’s ability to repair some of the damage caused by tobacco carcinogens once exposure ceases. However, it is important to note that the risk does not immediately return to the baseline level of never smokers. Instead, some elevated risk persists for years after quitting, particularly among individuals with a history of heavy or long-term smoking.
The persistence of increased risk among former smokers is primarily due to the cumulative genetic and epigenetic damage caused by prolonged exposure to carcinogens in tobacco smoke. DNA mutations, chronic inflammation, and alterations in the gastric mucosal environment may take years or even decades to resolve fully. For example, studies have shown that former smokers who smoked heavily (e.g., many pack-years) retain a higher risk of gastric cancer than light smokers or those who quit earlier in life.
Health Benefits of Quitting at Any Age
Despite the lingering risk, quitting smoking at any age confers substantial health benefits and reduces the likelihood of gastric cancer progression. The risk of gastric cancer declines progressively the longer a person remains smoke-free. Research indicates that after approximately 10 to 15 years of cessation, the risk of gastric cancer among former smokers approaches that of never smokers, although some studies suggest it may never completely normalize, especially in heavy smokers.
Quitting smoking also improves overall gastric health by reducing inflammation, oxidative stress, and the harmful effects of nicotine and other chemicals on gastric mucosa. It enhances immune function and promotes healing of the gastric lining, which helps reverse precancerous changes and reduces the risk of malignant transformation.
Broader Health Impacts
Beyond gastric cancer, quitting smoking reduces the risk of many other cancers, cardiovascular diseases, respiratory illnesses, and overall mortality. These broad health benefits provide additional motivation for smoking cessation at any stage of life. Tajul Islam Mamun, ScienceDirect 2024.
You Can Also Read Smoking and Bladder Cancer: What You Need to Know to Protect Yourself by Oncodaily

You Can Also Read Dr. Patricia Keegan on Neoadjuvant Chemotherapy for Gastric Cancer with Toripalimab by OncoDaily
Public Health Implications
Smoking is estimated to cause over 80,000 cases of stomach cancer globally each year, representing a significant public health burden. This highlights the critical importance of implementing effective smoking cessation programs and raising public awareness about the risks of tobacco use. Evidence shows that quitting smoking reduces the risk of stomach cancer substantially, with risk declining progressively the longer a person remains smoke-free. Smoking cessation not only lowers cancer risk but also improves treatment outcomes and survival for cancer patients.
Public health initiatives that provide accessible, evidence-based smoking cessation support—including behavioral counseling and pharmacotherapy—are essential to reduce tobacco-related stomach cancer incidence. Programs like Ontario’s STOP Program, which offers free nicotine replacement therapy and healthcare provider training, demonstrate how removing barriers to quitting can increase cessation rates. Moreover, integrating smoking cessation into cancer care improves prognosis and reduces the risk of second primary cancers. CDC 2024
Written by Meri Kirakosyan
FAQ
What are the warning signs or symptoms of gastric (stomach) cancer?
Early symptoms are often vague and include heartburn, indigestion, nausea, vomiting (sometimes with blood), feeling full quickly, abdominal discomfort or pain, unexplained weight loss, and anemia. Advanced signs may include difficulty swallowing, swelling of the abdomen, black stools, and jaundice if the cancer spreads to the liver.
Is gastric cancer hereditary?
Gastric cancer is rarely hereditary, accounting for about 1-3% of cases, often linked to inherited genetic mutations such as CDH1, which causes hereditary diffuse gastric cancer. Family history and certain genetic syndromes can increase risk.
What tests are available to diagnose or rule out gastric cancer?
Diagnosis primarily involves upper endoscopy with biopsy to examine stomach tissue, supported by imaging tests like CT scans and endoscopic ultrasound to assess spread. Genetic testing may be done for hereditary cases.
How does smoking increase the risk of stomach cancer?
Smoking introduces carcinogens that damage stomach lining cells and worsen Helicobacter pylori infection effects, increasing cancer risk.
Does quitting smoking reduce the risk of gastric cancer?
Yes, quitting smoking lowers the risk over time compared to current smokers.
Are current smokers at higher risk of gastric cancer compared to former or never smokers?
Current smokers have a significantly higher risk than former or never smokers.
Does smoking affect all types or locations of gastric cancer equally?
Smoking is more strongly linked to cancers in the upper stomach (cardia) but can affect other locations as well.
How does smoking contribute to the development of gastric cancer on a cellular level?
Smoking causes DNA damage, inflammation, and oxidative stress in stomach cells, promoting mutations and cancer development.
Are men more at risk of stomach cancer from smoking than women?
Men have higher rates of smoking-related stomach cancer, partly due to higher smoking prevalence.
Can passive smoking also increase the risk of gastric cancer?
Yes, passive (secondhand) smoking also increases gastric cancer risk, though less than active smoking.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
