MASCC 2025 Highlights BVGH’s Global Solutions to Financial Toxicity in Cancer Care
During the MASCC 2025 plenary session, Jennifer Dent, MBA, President of BIO Ventures for Global Health (BVGH), presented a powerful case for targeted interventions to reduce cancer-related financial toxicity across low- and middle-income countries (LMICs), with a focus on Africa.

The Financial Weight of Cancer in Africa
Dent began by highlighting the immense healthcare burden cancer imposes on African populations. In Nigeria, for example, the average annual income is just $1,880, and 76% of healthcare costs are paid out-of-pocket. Treating non-metastatic colorectal cancer costs $544—29% of annual income—while metastatic cases cost a staggering $9,912, over five times the average income. Patients must also contend with indirect costs such as travel, childcare, and lost wages.
Beyond individual hardships, the economic toll on the continent is profound. The total annual cancer-related economic loss in Africa in 2019 reached $42.9 billion, or approximately $840 million per country. Cancer’s indirect effects are also tragic: for every 100 women who die of cancer, 14–30 of their children may not survive to adulthood.
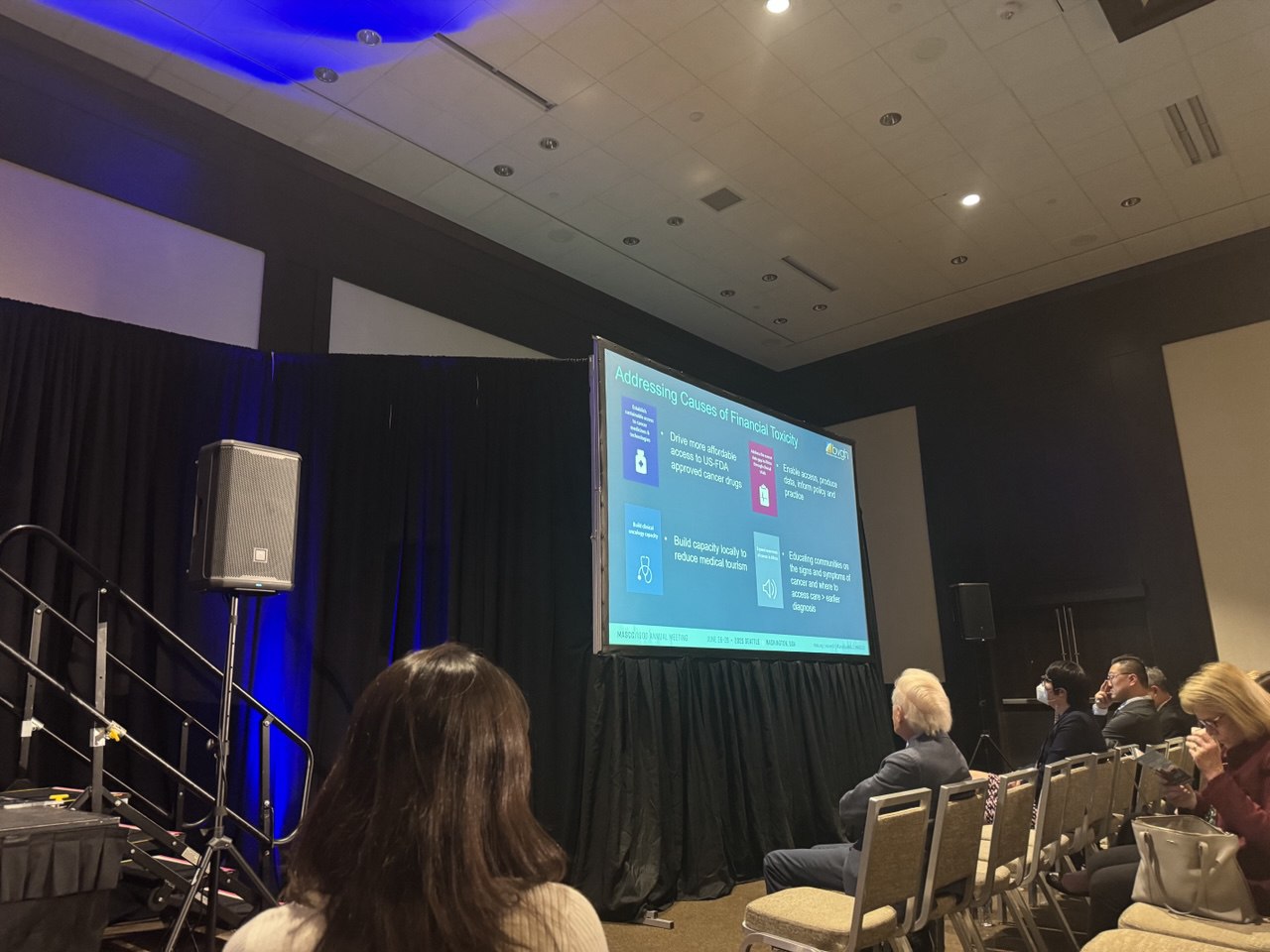
BIO Ventures for Global Health: Strategic Interventions
BVGH’s multipronged initiatives target both patient-level financial strain and system-level inefficiencies. Their flagship program, the African Access Initiative (AAI), addresses financial toxicity through:
- Improved access to US-FDA approved drugs
- Local capacity building to reduce medical tourism
- Enabling early-stage diagnosis
- Expanding availability of innovative cancer treatments
- Case Study: Mbingo Baptist Hospital, Cameroon
Mbingo Baptist Hospital (MBH), a 278-bed facility in Cameroon, treats over 70,000 patients annually, including 1,000 new cancer cases, many from rural and conflict-affected areas. One key challenge identified was the cost of rivaroxaban, commonly needed for cancer patients facing deep vein thrombosis.
In response, BVGH collaborated with Bayer to implement a tiered pricing model for Xarelto (rivaroxaban), based on a patient poverty index that considered occupation, household assets, insurance status, and livelihood. As a result, 4,100 packs of Xarelto were successfully distributed to patients in need.
National-Level Innovation: Nigeria’s NHIA Pilot
At the policy level, BVGH partnered with Nigeria’s National Health Insurance Authority (NHIA) to pilot a cancer drug access program. While NHIA currently does not cover cancer treatments, the pilot aims to integrate access-priced cancer drugs into existing payer schemes and target Nigeria’s most prevalent cancers, setting the groundwork for a more inclusive national policy.
Cost-Effectiveness in Pediatric Oncology
Children with cancer in sub-Saharan Africa are five times more likely to die than those in high-income countries, largely due to a belief that pediatric oncology is too expensive. To challenge this notion, BVGH, in collaboration with Lagos University Teaching Hospital and the Hospital for Sick Children, launched a pediatric cancer cost-effectiveness study across eight cancer hospitals. The study will provide crucial data on:
- Operational costs of pediatric cancer centers
- Impact of treatment abandonment
- Comparative efficiencies between centers
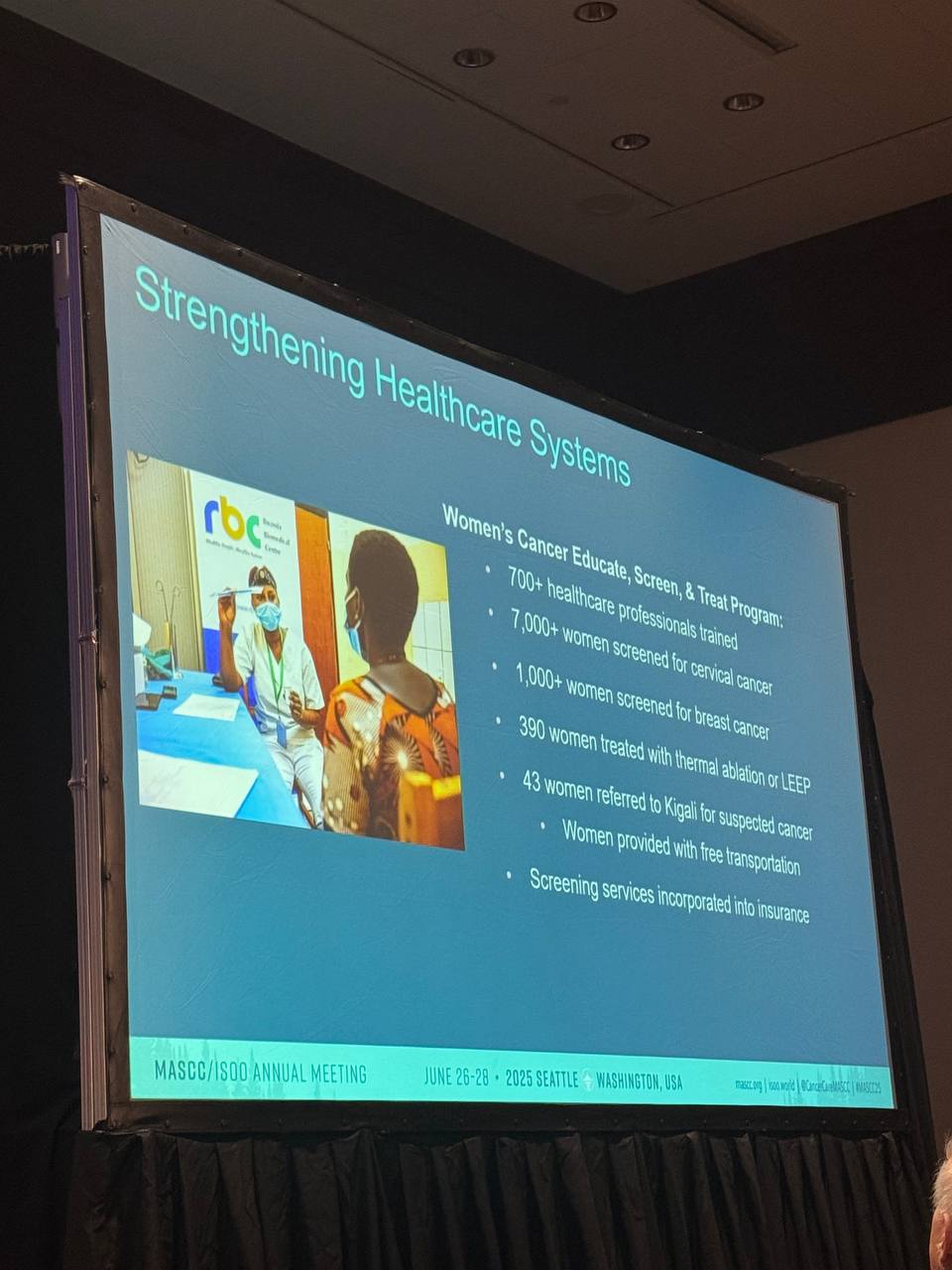
Cervical Cancer: A Preventable Tragedy in Rwanda
BVGH’s Educate, Screen & Treat (EST) initiative, in partnership with Rwanda’s Ministry of Health, integrated cervical cancer screening into routine care in Bugesera District:
- 7,000 women screened for cervical cancer
- 1,000 women screened for breast cancer
- 390 women treated with thermal ablation or LEEP
- 43 referred for tertiary care
- Over 700 healthcare professionals trained
- Screening services are now covered by insurance
This program showcases how well-integrated, community-based initiatives can dramatically increase access and reduce disease burden.
Radiotherapy: Hypofractionation for Cost Reduction
Dent also highlighted the radiotherapy gap: sub-Saharan Africa has only 195 radiotherapy machines compared to 4,172 in the U.S. and Canada. To maximize existing capacity, BVGH is leading HypoAfrica, a multi-country Phase II trial investigating hypofractionated radiotherapy (HFRT) for localized prostate cancer. HFRT involves fewer sessions with higher doses, offering:
- Lower costs ($1,699 vs. $3,389)
- Reduced treatment time
- Potential $606 million savings over 6 years in Africa
- Feasibility and toxicity outcomes comparable to European studies
New studies are expanding this model to cervical and breast cancer, and HFRT protocols are being refined through international mentorship networks and clinical collaborations.
Conclusion
Jennifer Dent’s plenary presentation made it clear: financial toxicity is both a medical and economic emergency in LMICs. Through programs like AAI, national insurance pilots, pediatric cost-effectiveness studies, and hypofractionated radiotherapy trials, BVGH is reshaping how cancer care is delivered—prioritizing affordability, sustainability, and equity.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
