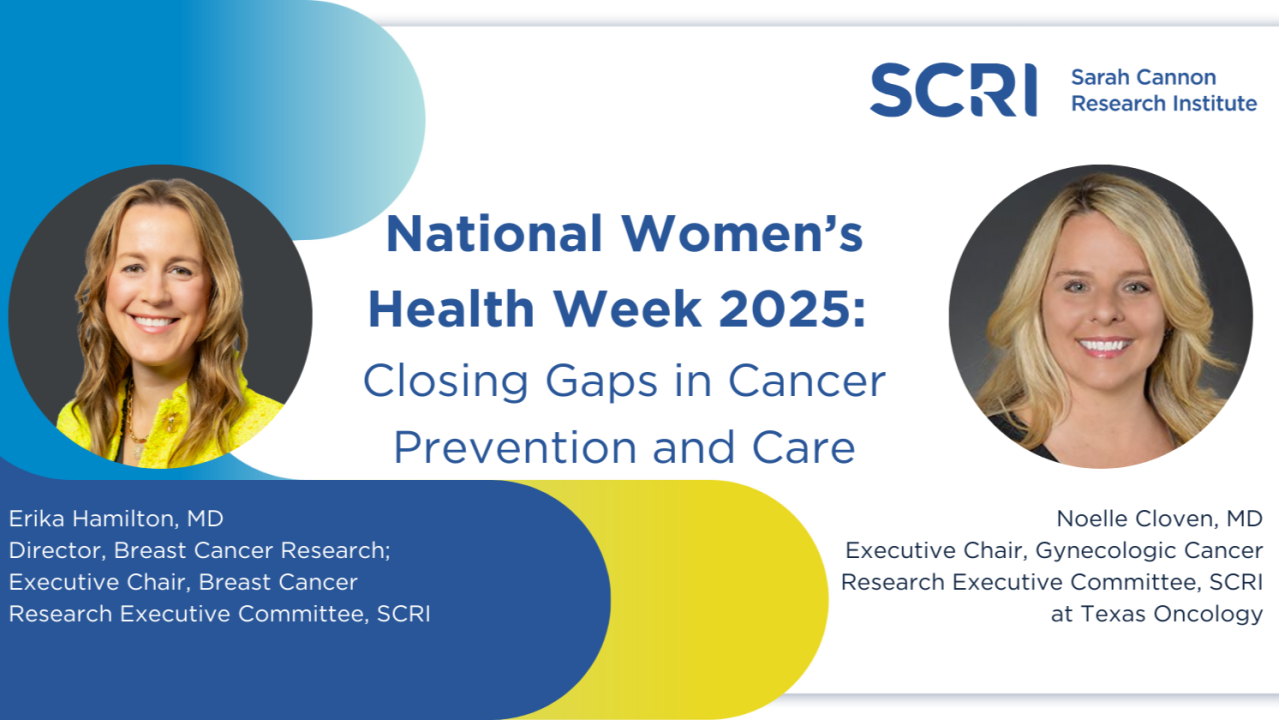
Erika Hamilton and Noelle Cloven on National Women’s Health Week 2025
Erika Hamilton, Medical Oncologist and the Director of Breast Cancer Program at Sarah Cannon Research Institute, shared a post on LinkedIn:
“What if one conversation could change a life? As physicians, we know it can, especially when that conversation leads to a better understanding of risk factors, early screening, and for those who need it, treatment and access to innovative clinical trials.
This National Women’s Health Week, I partnered with Dr. Noelle Cloven, Executive Chair, Gynecologic Cancer Research Executive Committee, SCRI at Texas Oncology, to reflect on the progress we’re making in breast and cervical cancer and the urgent work that still lies ahead. Read our co-authored piece below on how early action, education, and equitable community-based care can make all the difference for women.”
National Women’s Health Week 2025: Closing Gaps in Cancer Prevention and Care
“When we think about advancing women’s health, we often think of research, new treatments, and screening guidelines. But for us, it starts with something simpler…a conversation.
Sometimes it begins in the exam room, where a patient confides that it’s been years since their last mammogram. Or during a routine checkup, when unexpected symptoms lead to a life-changing diagnosis. We have experienced caring for a woman diagnosed with advanced breast cancer after skipping mammograms for four years. Had her cancer been found earlier, her journey might have been different.
Other times, it begins with hope. Like the patient who enrolled in a breast cancer clinical trial, and is now cancer-free, knowing that her participation not only helped her, but may help thousands of others in the future.
These moments remind us that when it comes to women’s health, early action matters.
The role of prevention
Breast and cervical cancers are two of the most common cancers in women. But they are also among the most preventable or treatable when caught early. That’s why screenings like mammograms for breast cancer and Pap tests along with HPV vaccination for cervical cancer, remain essential tools in protecting women’s health.
Yet barriers still exist. Many women are unsure when to start screening or think they may not need one as they are absent of clinical symptoms. In cervical cancer, for example, nearly one-third of cases occur in women over age 65, even though guidelines often recommend stopping screening at that age if past results have been consistently normal. In breast cancer, we’ve seen significant changes in who gets diagnosed and when. More aggressive cancers are increasingly being found in younger women, especially among Black women, underscoring why new recommendations now suggest starting mammograms at age 40.
But screening is only the first step. When a result comes back positive for cancer, the conversation must quickly shift from early detection to proactive, informed care. That’s where timely access to expert guidance, treatment options, and clinical trials becomes essential.
Research within reach
Early detection is powerful, and our work at Sarah Cannon Research Institute brings the latest treatment options to people facing cancer in their communities.
Through more than 1,000 active community-based clinical trials in collaboration with more than 1,300 research physicians, we’re able to offer patients cutting-edge care where they live. This network helps reduce burdens that often go unacknowledged (missed work, childcare, transportation) which can be barriers to care, especially in underserved or rural communities. It also improves trial accessibility and helps ensure new therapies reflect and serve real-world populations.
In our roles, we’re proud to have witnessed how this network transforms lives. For example, we’ve helped women access minimally invasive surgeries designed to preserve fertility and reduce long-term side effects. We’ve also enrolled patients in trials that offer newly diagnosed women the option to receive immunotherapy earlier in their treatment journey.
Where innovation meets impact
The science behind cancer care is evolving rapidly. From more precise genomic profiling to new classes of therapies like antibody-drug conjugates and immunotherapies, we’re seeing meaningful progress in both breast and cervical cancer treatment.
In breast cancer, personalization has become a strong focus. By identifying tumor characteristics, we can avoid overtreatment and better match therapies to a patient’s unique needs. In cervical cancer, newer strategies including less invasive surgeries and novel drug combinations are leading to better outcomes and fewer long-term side effects.
But our work doesn’t stop there. As practicing physicians, we’re also focused on expanding education and raising awareness so that patients understand their full range of options and stay informed on the latest screening guidelines and lifestyle recommendations such as reducing alcohol intake.
A shared responsibility
This National Women’s Health Week, our message is simple: Start the conversation. Talk to your doctor about your risk factors, know when you’re due for a screening and ask about clinical trials early in your care journey. And if you notice something that doesn’t feel right, whether it’s unusual bleeding, persistent fatigue or a new lump, don’t wait. Getting checked early could make all the difference.
As physicians, we’ve seen how small steps can lead to life-changing outcomes. And as researchers, we’re working toward a future where no woman’s outcome is determined by her ZIP code, background, or age. Because in the fight against cancer, progress can happen when women are empowered to take charge of their health and when communities are equipped to help them do so.”
More posts featuring Erika Hamilton.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
