
Nico Gagelmann: Gastrointestinal (GI) manifestations in hematology
Nico Gagelmann, Co-Chair for the European Society for Blood and Marrow Transplantation (EBMT) Trainee Committee, shared a post on X/Twitter:
“Gastrointestinal (GI) manifestations in hematology
A short visual thread with diagnosis
Intro: -lympho-/myeloproliferative disorders
-nodal and/or extranodal
-GI tract one of the most common extranodal sites
-diagnosis of GI hematologic malignancy challenging
- esp in absence of documented nodal/extranodal disease
- due to higher incidence of other pathologies
Importance of imaging:
-although tissue biopsy is often required to reach the definitive diagnosis, imaging plays a crucial role in raising suspicion of underlying hematologic malignancy
-imaging also guides biopsies, staging, and evaluating response to treatment
Lymphoma I:
-primary GI lymphoma comprises only 1–8% of all GI malignancies
-GI tract is the most common site for extranodal lymphomas
-primary GI lymphomas account for 30–40% of extranodal non-Hodgkin lymphoma (NHL)
-secondary dissemination even more frequent: up to 50%
Lymphoma II:
-stomach most common (50–75%)
–followed by small intestine (esp ileum), colon
-pathogenesis very complex
- immune interactions, mutations
- high risk: EBV, Helicobacter pylori, HIV, celiac disease
BUT
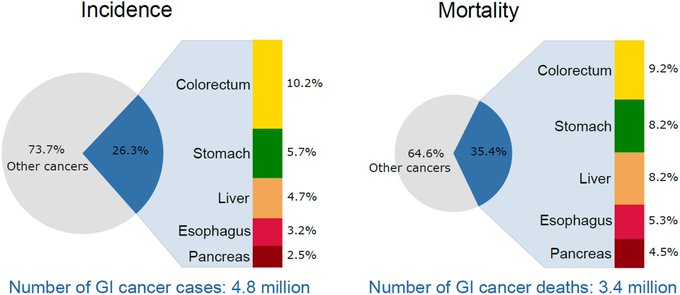
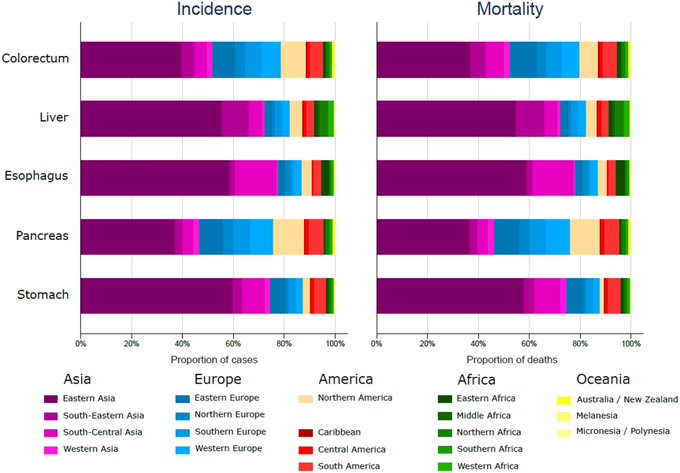
-beware that GI cancers and risk factors vary across regions
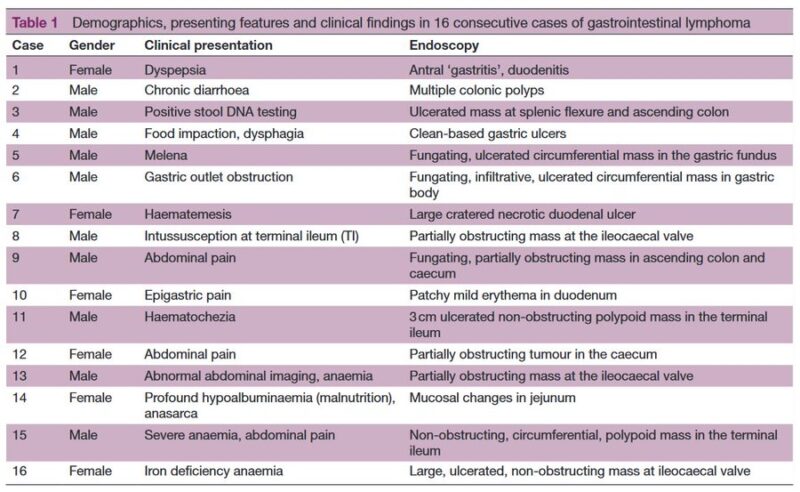
Clinic:
-45–65% of all GI lymphomas present with abdominal pain due to a mass or bowel obstruction -(paradoxical) diarrhea, constipation
-hemorrhage -non-specific upper GI symptoms
-ulceration, intussusception
-accurate diagnostics (imaging, endoscopy+pathology) critical
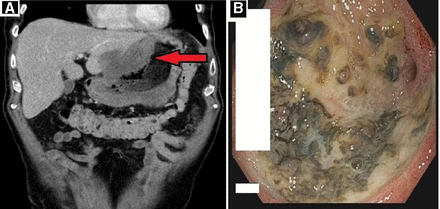
 Diffuse-large B cell lymphoma:
Diffuse-large B cell lymphoma:
-most common GI lymphoma
-beware of epigastric pain/discomfort (75-95%), anorexia (~50%)
-either de novo or transform from low-grade B-cell lymphomas
-high risk: atrophic gastritis, H pylori, immunodeficiency, inflammatory bowel disease, and EBV
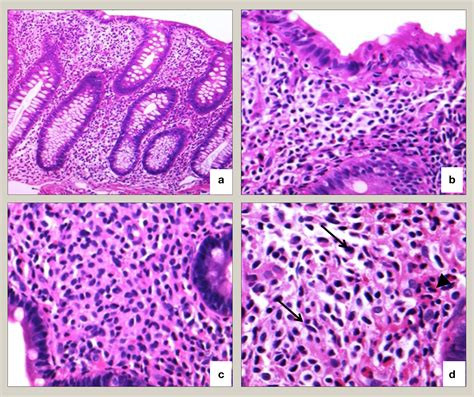
Extranodal marginal zone lymphoma:
-indolent -50% of primary gastric, 10% of bowel lymphomas
-usually multifocal, superficial
-can coexist with DLBCL
-involvement of small intestinal disease in 1/3 of GI lymphomas in Middle East
-associations: H pylori, Campylobacter jejuni
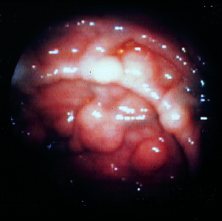
Mantle cell lymphoma (MCL):
-rare and aggressive
-5–13% of primary GI lymphomas
-can develop multiple lymphomatous polyposis
-main involvement of jejunum/ileum, colon, rectum
-nearly all cases of MCL overexpress cyclin D1 due to the t(11;14)
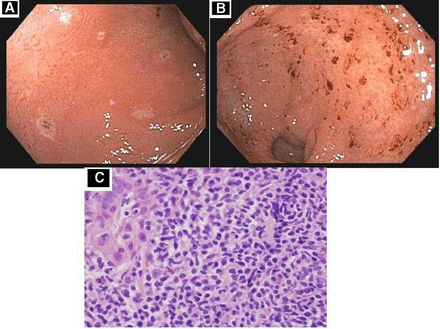
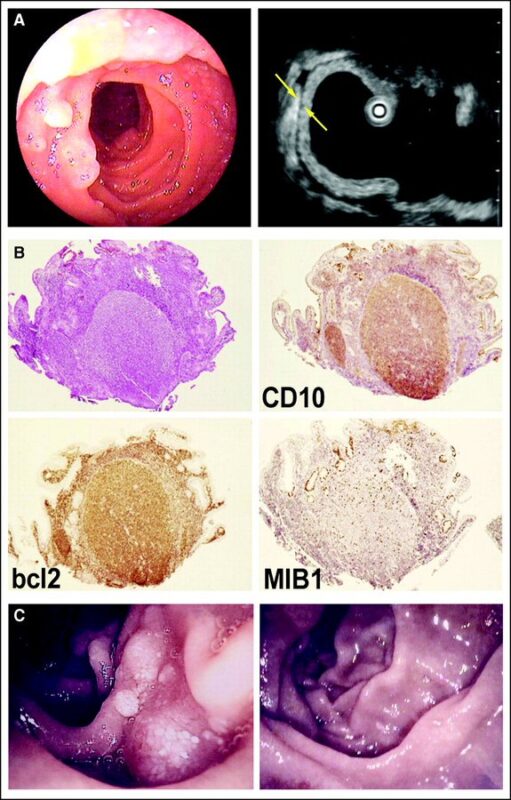
 Follicular lymphoma (FL):
Follicular lymphoma (FL):
-low-grade B-cell lymphoma
-uncommon in GI tract, representing only 5–12% of primary GI NHL
-usually involves duodenum followed by jejunum and ileum
-invades villous mucosamultifocal mucosal polyposis -cytogenetic hallmark is t(14; 18), in 90%
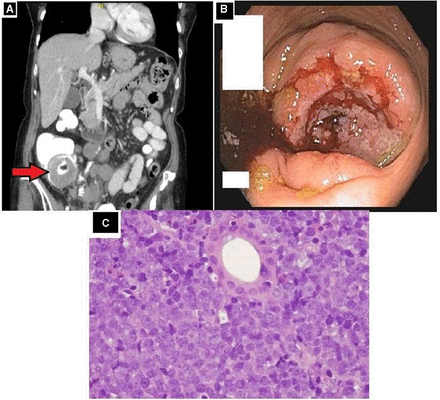
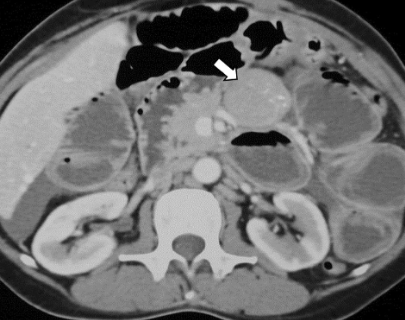
Burkitt lymphoma (BL):
-rare and aggressive
-most common pediatric NHL, 40% of all pediatric lymphomas
-accounts for 5% only of primary GI NHL
-endemic, sporadic, immunodeficiency (HIV)
-grows fast
-terminal ileum or ileocecal
- extensive wall thickening, large mass
Plasmablastic lymphoma (PBL):
-extremely rare
-strongly associated with immunodeficiency disorders and EBV
-typically positive for plasma cell antigens
– originally discovered in the oral cavity of HIV-infected patients
-evidence of imaging still limited
Enteropathy‑associated T‑cell lymphoma (EATL):
-~3–4% of all primary GI NHL
-2 types: (1) associated with celiac disease (~85%) or (2) not
-often multifocal
-type 1 often with transmural necrosis with a high risk of bowel perforation as well (19–50%)

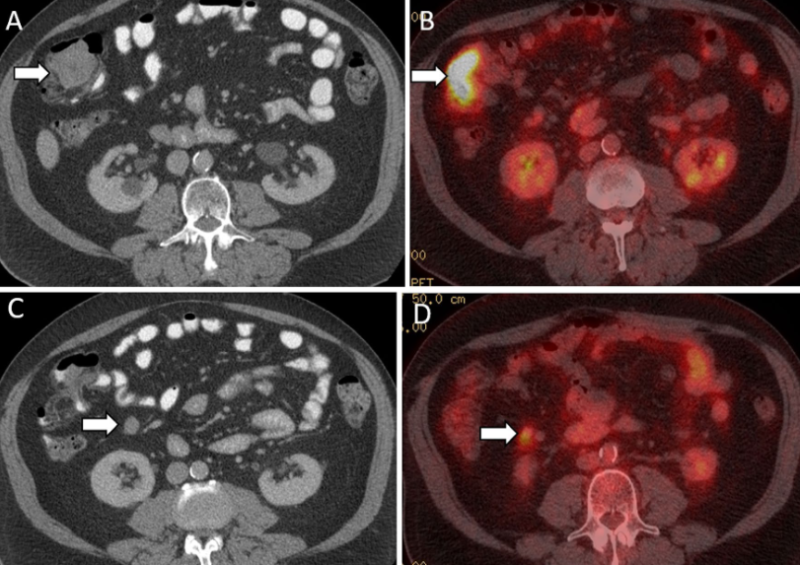
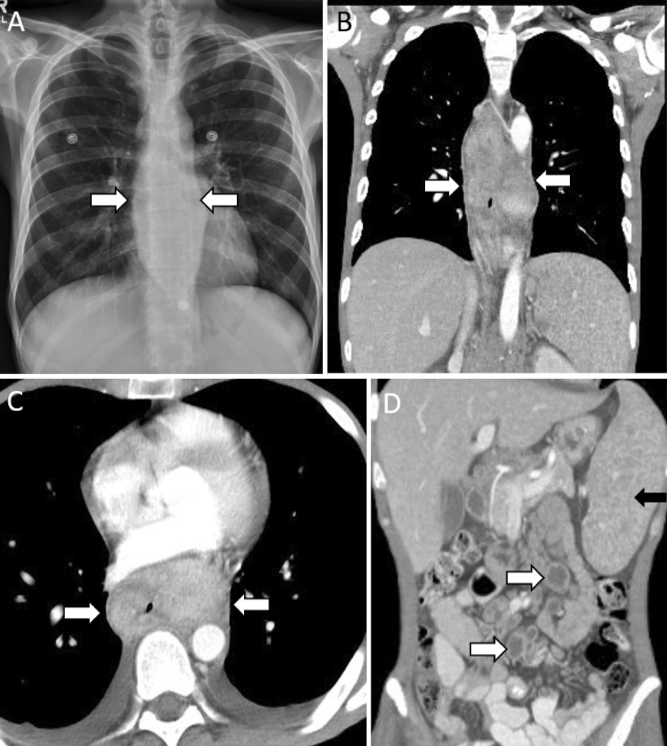
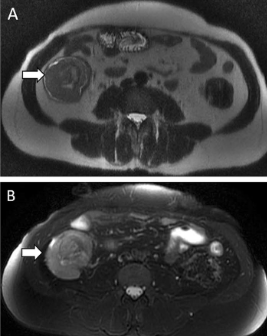
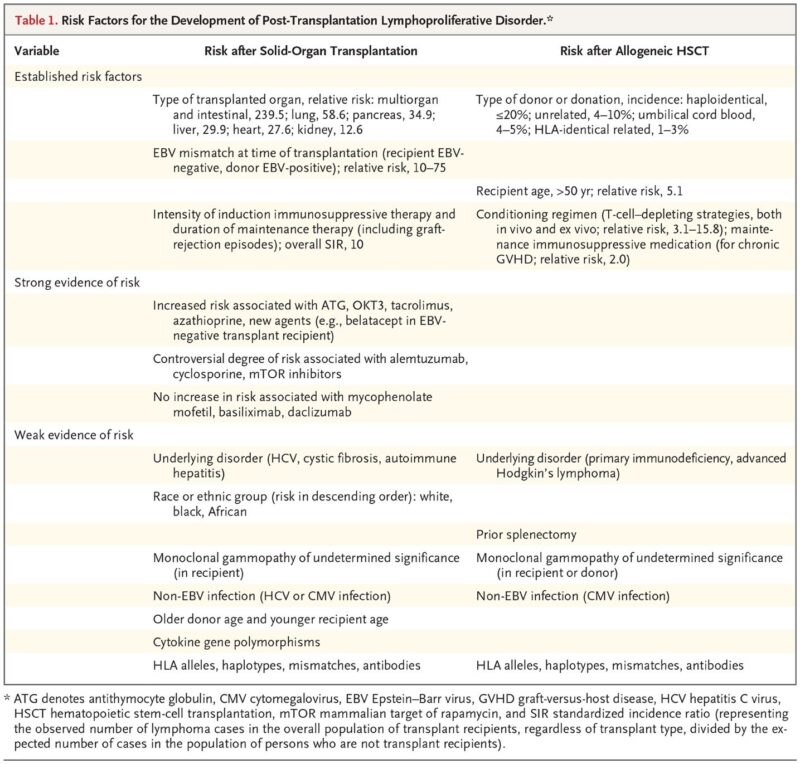
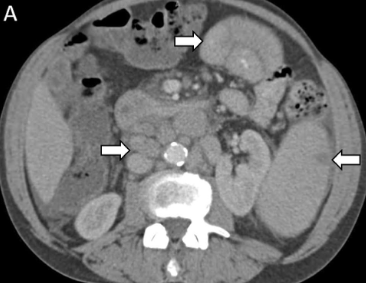
Post‑transplant lymphoproliferative disorder (PTLD):
-heterogeneous lymphocytic disorders in transplant recipients
-risk varies, higher for small bowel (22%) and transplant (4–10%)
-extranodal involvement in 80%
-differential: infection, primary GI cancer, metastases
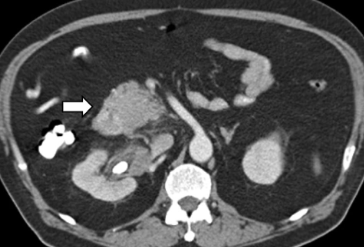
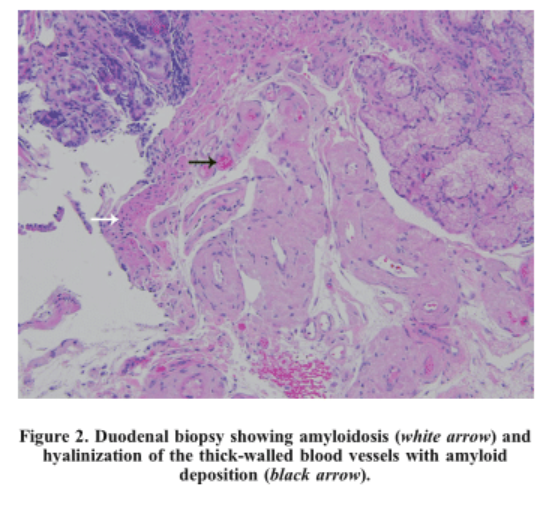
 Multiple myeloma:
Multiple myeloma:
-uncontrolled clonal proliferation of plasma cells
-extramedullary disease (EMD) incidence varies (20-60% of cases)
-most common sites: liver, lymph nodes, spleen, kidneys, pleura
-GI uncommon (mostly stomach and small bowel), GI hemorrhage, GI amyloidosis
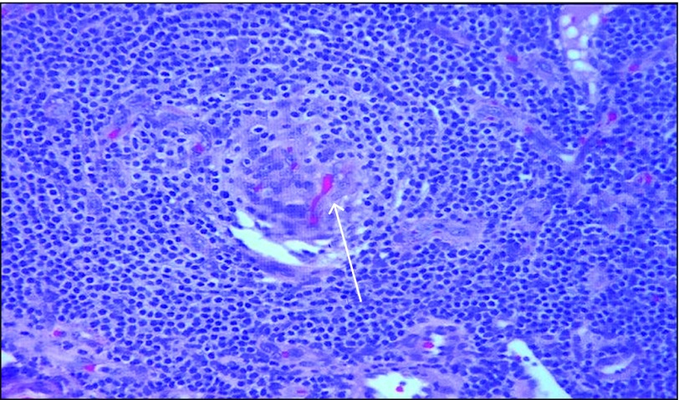
Mastocytosis:
-rare
-lymphoproliferative disorders: proliferation and accumulation of mast cells in one or more organs
-skin (80%): urtikaria, rash
-GI involved in 70–80% of systemic mastocytosis, also liver, spleen
-histamines cause diarrhea, peptic ulcer disease
 ”
”
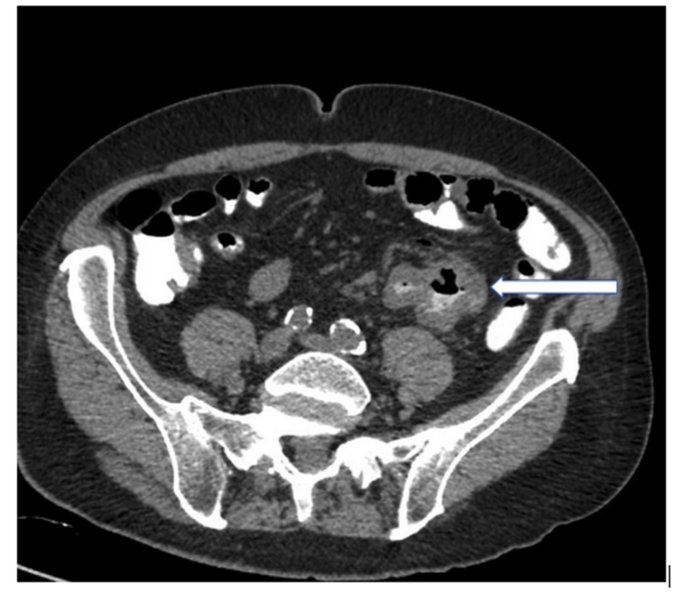
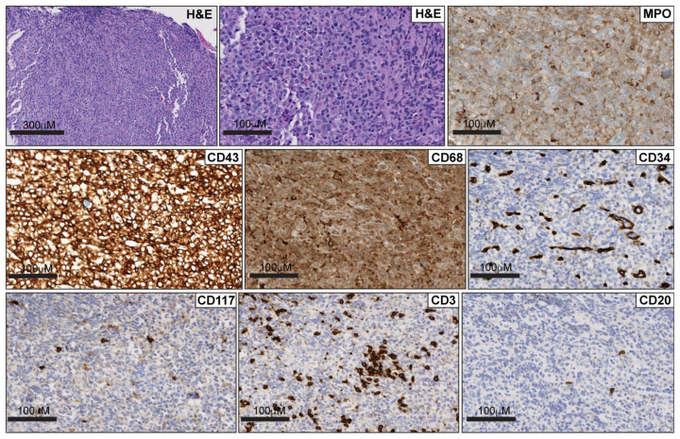
Myeloid sarcoma (MS):
-extramedullary proliferation of immature myeloid cells or blasts
-seen in patients with acute myeloid leukemia
-rarely isolated, preceding leukemia diagnosis
-GI common -mass effect: acute pain, obstruction
-polypoid mass or bowel wall thickening

Castleman disease (CD):
-rare heterogeneous group of pnon-clonal lymphoproliferative disorders
-mostly lymph node involvement -uni-or multicentric
-hyaline vascular variant (most common 90%), plasma cell variant, mixed variant
-GI involvement only in cases, mainly stomach
Source: Nico Gagelmann/X
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
