Francisco Conesa Buendía: Unveiling the Long-Term Safety of CAR-T and Gene-Modified T Cell Therapies
Francisco Conesa Buendía, Assistant of Cell and Gene Therapies Manufacturing at Memorial Sloan Kettering Cancer Center, shared a post on LinkedIn:
“Unveiling the Long-Term Safety of CAR-T and Gene-Modified T Cell Therapies
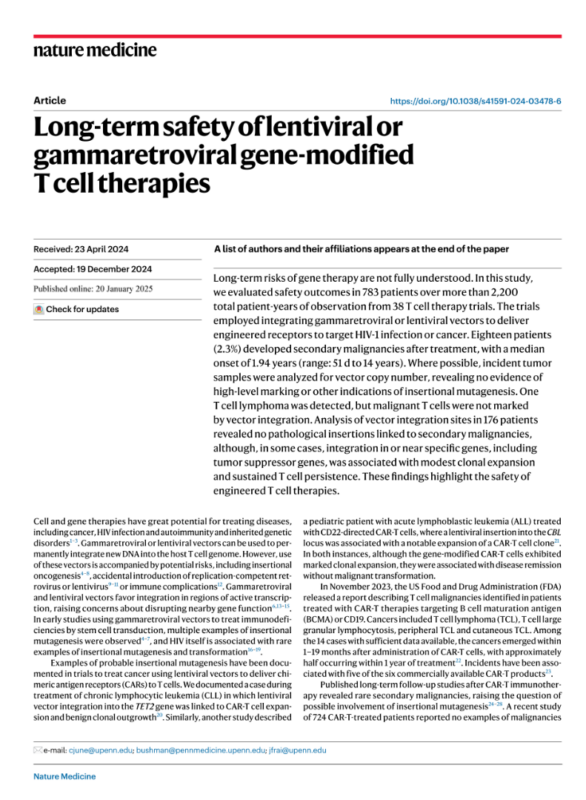
A recent Nature Medicine study offers groundbreaking insights into the long-term safety of lentiviral and gammaretroviral gene-modified T cell therapies, analyzing 783 patients across 38 trials with over 2,200 patient-years of follow-up. This pivotal research highlights the promise and safety of CAR-T therapies while identifying areas for optimization.
Key Findings
1. Secondary Malignancies (SPMs):
- Incidence: 18 patients (2.3%) developed SPMs, a rate of 0.0082 events/patient-year.
- Timing: Median onset was 1.94 years post-infusion (range: 51 days–14 years).
- Types: Hematologic (AML, MDS, EBV-driven DLBCL) and solid tumors (lung, prostate, melanoma).
- Reassurance: Tumor analysis found no evidence of insertional mutagenesis, confirming the safety of lentiviral and gammaretroviral vectors.
2. Adverse Events:
- Most common: Infections and immune complications, linked to B cell depletion (CD19/BCMA CAR-T) and lymphodepletion chemotherapy.
- Persistent hypogammaglobulinemia affected 76% of BCMA CAR-T patients, requiring IV immunoglobulin.
- Severe events (≥Grade 3): Only 5.36% of patients, with infections leading.
3. Clonal Dynamics:
- Integration hotspots were identified near tumor suppressor genes (e.g., EP300, CBFB, KMT2D), linked to non-malignant clonal growth and therapeutic persistence.
- No malignant transformations were observed, even in cases with clonal expansions (e.g., TET2 integration in one patient).
4. Demographics:
- Disease types: 81% hematological cancers, 12% solid tumors, and 7% HIV.
- Adults had a higher SPM risk (0.0125 events/patient-year) than children (0.0030 events/patient-year).
Implications for the Field
1. Safety Confirmation: CAR-T therapies exhibit a low risk of SPMs, with no detectable vector-mediated oncogenesis.
2. Therapeutic Optimization: Targeting integration hotspots near tumor suppressor genes could improve T cell persistence and efficacy.
3. Future Innovations: Emerging in vivo CAR-T platforms could further enhance safety, accessibility, and scalability.
What’s Next for CAR-T Therapies?
To maximize potential:
– Minimize infection risks and immune-related complications.
– Refine vector integration for enhanced safety and durability.
– Expand CAR-T applications to solid tumors and rare diseases.
These findings align with the exciting progress we’re making toward improving cancer treatments. They also echo the importance of fundraising efforts like Cycle for Survival at MSK, which supports innovative therapies for rare cancers.
For more, check out my earlier post here.”
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
