Lung cancer remains the deadliest cancer globally, responsible for nearly one in five cancer deaths. While this diagnosis can feel overwhelming, it’s important to understand that not all lung cancers are the same—and some are curable, particularly when detected early. With the evolution of diagnostic tools, surgical techniques, radiotherapy, immunotherapy, and precision medicine, the lung cancer cure rate is gradually improving across many patient groups. In clinical terms, a “cure” implies complete eradication of disease, with no recurrence over time. For patients, this translates to long-term survival and quality of life, especially if the disease is caught before it spreads.

Read About Metastatic Lung Cancer on OncoDaily
Defining Cure in the Context of Lung Cancer
A cancer “cure” typically implies a sustained remission with little to no chance of relapse. In lung cancer, this is realistically achievable in localized disease, primarily in early-stage non-small cell lung cancer (NSCLC), which accounts for about 85% of all cases. The remaining cases—classified as small cell lung cancer (SCLC)—are more aggressive and rarely curable unless detected at a very limited stage.
Clinical data from the American College of Chest Physicians suggest that for stage I NSCLC treated surgically, the five-year survival rate may exceed 80%, which is often considered a surrogate for cure (Howington et al., 2020). Meanwhile, long-term remission, or durable control, is becoming increasingly common in some cases of advanced disease treated with immune checkpoint inhibitors and targeted therapies.
Non-Small Cell Lung Cancer: The Best Chance for Cure
The majority of lung cancer cases are NSCLC. This group includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. The potential for cure is strongly tied to the stage at diagnosis. In the IASLC’s TNM staging update, patients with stage IA tumors smaller than 2 cm and no nodal involvement demonstrated five-year survival rates nearing 92% after surgical resection alone, marking the highest documented cure rates in lung cancer (Goldstraw et al., 2016).
Patients with stage II disease may also be cured, especially when surgery is followed by adjuvant chemotherapy. With combined-modality treatment, 5-year survival rates in stage IIA and IIB range between 53% and 65%, according to SEER data and international thoracic oncology registries.
For stage IIIA NSCLC, where cancer involves regional lymph nodes, the likelihood of cure diminishes but remains possible. Advances in neoadjuvant chemoimmunotherapy (e.g., nivolumab + platinum doublets) followed by surgical resection have shown promising results. The CheckMate 816 trial reported a significant improvement in pathological complete response and event-free survival in this setting, hinting at increased potential for cure even in stage III disease (Forde et al., 2022).
Read About Non-Small Cell Lung Cancer on OncoDaily
Small Cell Lung Cancer: A More Aggressive Challenge
SCLC tends to spread rapidly and is usually diagnosed at an extensive stage. Cure is achievable only in a minority of patients with limited-stage SCLC treated aggressively with concurrent chemoradiation. In those who respond well to cisplatin-etoposide and thoracic radiotherapy, 5-year survival rates reach up to 25% (Gazdar et al., 2017). However, this accounts for only a fraction of patients, as most present with extensive-stage disease.
Recent advances in first-line immunotherapy, including atezolizumab and durvalumab, have modestly improved survival in extensive-stage disease, yet cure remains elusive (Horn et al., 2018).
Read About Small Cell Lung Cancer on Oncodaily
Cure Rates by Stage: The Impact of Early Detection
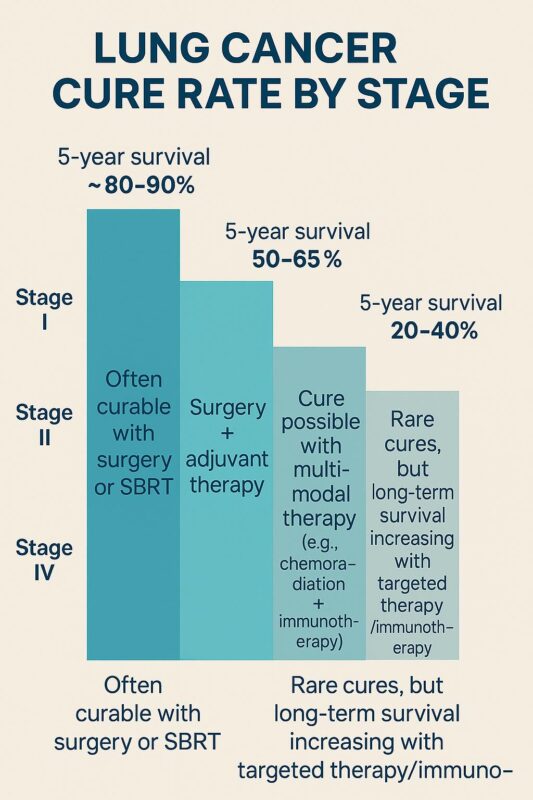
The stage of diagnosis is one of the most powerful predictors of whether lung cancer is curable. For patients diagnosed with stage I disease, particularly tumors under 2 cm and no nodal involvement, the 5-year survival can be as high as 90% after surgery or stereotactic body radiation therapy (SBRT), which is considered curative for non-surgical candidates (Videtic et al., 2015).
For stage II, cure is still possible with surgery plus adjuvant chemotherapy. These patients generally have 5-year survival rates ranging from 40% to 60%, depending on the extent of lymph node involvement.
In stage III disease, particularly stage IIIB where surgical resection may not be feasible, combined chemoradiotherapy followed by durvalumab consolidation has increased the median progression-free survival from 5.6 to 16.8 months and improved 3-year overall survival (Antonia et al., 2018). This approach has redefined long-term management and introduced hope for durable remission in previously inoperable cases.
Once lung cancer reaches stage IV, systemic spread reduces the possibility of cure significantly. Nonetheless, the long-term survival of select patients has improved remarkably due to the integration of targeted therapies for EGFR, ALK, and ROS1 mutations, as well as immune checkpoint blockade with PD-1/PD-L1 inhibitors. In the CheckMate 227 trial, patients with PD-L1 ≥1% NSCLC treated with nivolumab and ipilimumab had 5-year survival rates of over 24%—an outcome once unthinkable for metastatic disease (Hellmann et al., 2021).
Tumor Biology: A Key Determinant of Cure Rate
Molecular profiling has revolutionized how we approach lung cancer, making cure more achievable in selected subgroups. Tumors harboring EGFR mutations, ALK rearrangements, or MET exon 14 skipping mutations can respond dramatically to oral targeted therapies. While not yet curative in stage IV settings, these agents have produced long remissions and are now being trialed in earlier stages with curative intent.
For example, the ADAURA trial showed that adjuvant osimertinib, an EGFR inhibitor, in resected stage IB–IIIA NSCLC, significantly reduced recurrence and improved disease-free survival, suggesting that cure is more likely in EGFR-positive early-stage patients who receive adjuvant therapy (Wu et al., 2020).
Why Lung Cancer Is Often Diagnosed Too Late
The lung has no pain receptors, so tumors often grow silently. Symptoms like persistent cough, weight loss, or chest pain tend to appear only in advanced stages. As a result, over 50% of patients are diagnosed with stage III or IV disease, when cure is much harder to achieve. This is why low-dose CT screening is recommended for high-risk individuals, such as long-term smokers aged 50–80. Early detection through screening has been shown to reduce lung cancer mortality by 20–24% (Aberle et al., 2011).
The Role of Immunotherapy in Long-Term Remission
Immunotherapy is redefining outcomes in advanced lung cancer. Drugs like nivolumab, pembrolizumab, and durvalumab unleash the immune system against tumor cells and have enabled long-term survival in a subset of patients. Some are living beyond five years with stage IV disease—a milestone once unimaginable. While not all these cases qualify as a “cure” by traditional standards, the concept of functional cure—living cancer-free without therapy—is now within reach for some.
Read About Immunotherapy for Lung Cancer on OncoDaily
Disparities in Cure Rates
Unfortunately, not all patients benefit equally from advances in lung cancer care. Studies show that racial and socioeconomic disparities affect access to early detection, high-quality surgery, and systemic treatments. African American and low-income patients are often diagnosed at later stages and have lower survival despite similar tumor biology (Zavala et al., 2021). Addressing these gaps is crucial for improving overall cure rates.
Conclusion
The lung cancer cure rate has improved dramatically over the past two decades—thanks to early diagnosis, precision therapies, and immunotherapy. While stage I patients may have a realistic expectation of cure, patients with more advanced disease are also experiencing longer survival and better quality of life than ever before. As research advances, what was once a terminal diagnosis is increasingly becoming a chronic, and in some cases, curable illness.
Patients are encouraged to discuss their specific type, stage, and molecular profile with their oncologist, as personalized treatment plans can make a significant difference in outcomes. Early screening, participation in clinical trials, and access to expert care remain key tools in the journey toward cure.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD