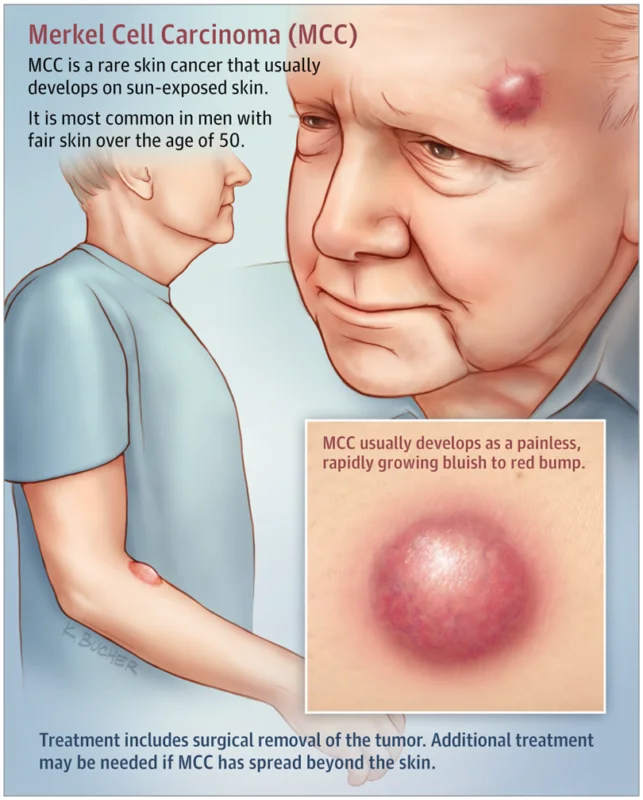
Merkel Cell Carcinoma (MCC) is a rare but aggressive skin cancer that grows quickly and can spread to other parts of the body. It often appears as a painless, firm, red or purple lump, usually on sun-exposed areas like the face or arms.
This article will cover what MCC is, how common it is, its causes and risk factors, symptoms, diagnosis, and staging. We will also discuss treatment options, myths and misconceptions, prevention tips, and new research on emerging therapies. Understanding MCC can help with early detection and better treatment outcomes.
What Is Merkel Cell Carcinoma?
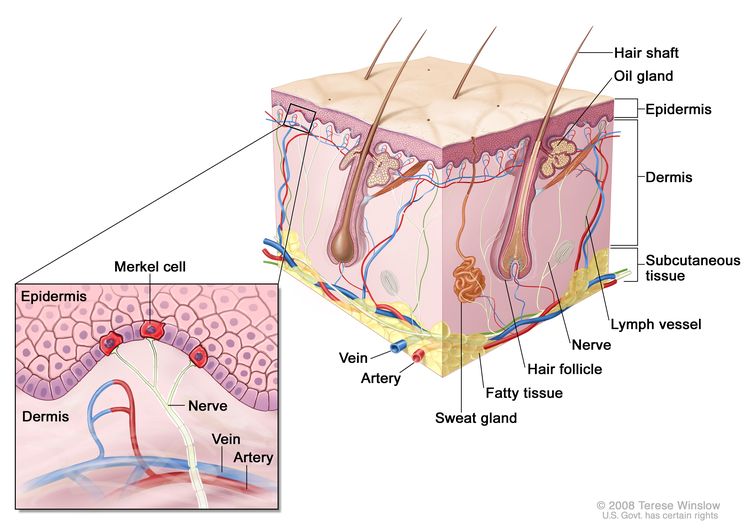
Merkel Cell Carcinoma (MCC) is a rare but aggressive type of skin cancer that develops in Merkel cells, which are found in the top layer of the skin. These cells help with touch sensation, but when they become cancerous, they grow uncontrollably and can spread quickly to the lymph nodes and other organs. While MCC is uncommon, it requires immediate medical attention to improve outcomes.
According to the American Cancer Society, about 3,000 people are diagnosed with MCC each year in the United States. The risk of developing MCC increases with age, and it is very rare in individuals under 50. Approximately 8 out of 10 people diagnosed with MCC are over the age of 70.
Is MCC the Same as Other Skin Cancers?
No, Merkel Cell Carcinoma (MCC) is different from other skin cancers like basal cell carcinoma, squamous cell carcinoma, and melanoma. While all skin cancers start in the skin, MCC is rarer and more aggressive than most.Unlike basal cell carcinoma and squamous cell carcinoma, which grow slowly and rarely spread, MCC can grow quickly and spread to other parts of the body, including the lymph nodes and organs. This makes early diagnosis and treatment especially important.
MCC is also different from melanoma, which starts in the pigment-producing cells of the skin and is often linked to moles. MCC develops in Merkel cells, which help with touch sensation and are found in the upper layers of the skin. While both MCC and melanoma are serious, MCC is less common but spreads faster, making early treatment critical.
Since MCC can sometimes look like a harmless lump or cyst, it is often misdiagnosed at first. That’s why any unusual growth, bump, or skin change—especially if it grows fast or changes color—should be checked by a doctor as soon as possible.
Causes and Risk Factors
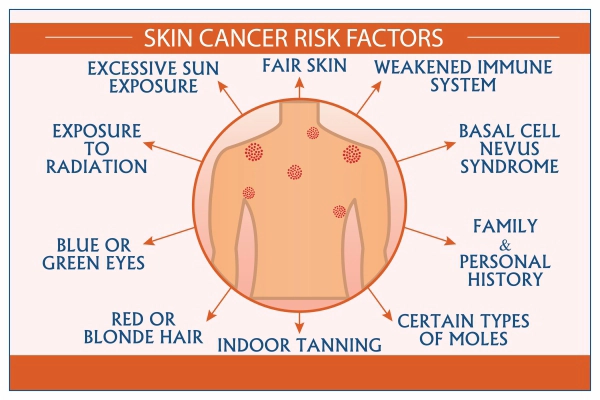
Merkel Cell Carcinoma (MCC) happens when skin cells start growing uncontrollably, but the exact cause isn’t always clear. Doctors have found several risk factors that can increase the chances of developing MCC. One of the biggest risk factors is too much sun exposure. Spending a lot of time in the sun without protection, especially over many years, can damage the skin and lead to MCC. People with fair skin are at a higher risk because their skin has less natural protection from UV rays.
A weakened immune system can also make MCC more likely. This includes people who have had an organ transplant, certain autoimmune diseases, or conditions like HIV/AIDS. A weaker immune system makes it harder for the body to fight off abnormal cell growth. Another important risk factor is the Merkel Cell Polyomavirus. This virus is found in many MCC cases, though not everyone who has the virus will develop cancer. Scientists are still studying how this virus might trigger MCC.Age also plays a role, as MCC is much more common in people over 50, and the risk increases with age. Men are also slightly more likely than women to develop MCC.
While these factors increase the risk, anyone can develop MCC, so it’s important to watch for unusual skin changes and talk to a doctor if you notice anything new or concerning.
Symptoms and Warning Signs
Merkel Cell Carcinoma (MCC) often appears as a painless lump on the skin that grows quickly. Because it can look like a harmless bump, cyst, or pimple, many people don’t realize it’s cancer at first. Recognizing the early signs can help with early detection and better treatment outcomes.
The most common symptom is a firm, dome-shaped lump that may be red, pink, purple, or skin-colored. It usually appears on sun-exposed areas like the face, neck, arms, or scalp. Unlike a normal pimple or bug bite, MCC doesn’t go away and tends to grow fast. In some cases, the skin around the lump may become shiny, stretched, or ulcerated (open sore). MCC is usually not painful, which can make it easy to ignore. As the cancer progresses, swollen lymph nodes (lumps under the skin in the neck, armpits, or groin) may appear, which can mean the cancer has started to spread. Because MCC can be aggressive, any new lump or skin change that grows quickly should be checked by a doctor right away. Early diagnosis can make a big difference in treatment success.
When to See a Doctor
You should see a doctor as soon as you notice any unusual skin changes that don’t go away. If a new lump, bump, or growth appears on your skin and keeps getting bigger, it’s important to have it checked. Even if it doesn’t hurt, any skin change that looks different from the rest of your skin should be evaluated.
If you have a history of skin cancer or a weakened immune system, regular skin checks are even more important. A doctor can examine the area, perform tests if needed, and rule out anything serious. Early detection of Merkel Cell Carcinoma can make treatment more successful, so don’t ignore a growth that seems unusual. If something doesn’t look or feel right, it’s always best to get it checked!
How Is MCC Diagnosed?
If a doctor suspects Merkel Cell Carcinoma (MCC), they will perform a series of tests to confirm the diagnosis. The first step is usually a skin exam, where the doctor checks the lump and looks for any other unusual areas. To know for sure if the lump is cancerous, the doctor will perform a biopsy. This means removing a small sample of the lump and examining it under a microscope. A biopsy is the only way to confirm MCC. If cancer is found, further tests are needed to see if it has spread.
Doctors may also order imaging tests, such as CT scans, MRIs, or PET scans, to check if the cancer has reached the lymph nodes or other parts of the body. In some cases, a sentinel lymph node biopsy is done to see if cancer has spread to the lymph nodes near the tumor. Early and accurate diagnosis is important because MCC can grow and spread quickly. If you have a suspicious lump, seeing a doctor as soon as possible can help with early detection and better treatment options.
What Are the Stages of Merkel Cell Carcinoma?
Merkel Cell Carcinoma (MCC) is staged based on how far the cancer has spread in the body. Staging helps doctors decide the best treatment options. The stages range from Stage 0 (earliest) to Stage IV (most advanced).
In Stage 0, the cancer is only in the top layer of the skin and has not spread deeper. Stage I and Stage II mean the tumor is still in the skin but may be larger or growing deeper into the tissue. Stage III indicates the cancer has spread to nearby lymph nodes, which may cause swelling in areas like the armpit or neck. Stage IV, the most advanced stage, means MCC has spread to distant parts of the body, such as the liver, lungs, or bones. The earlier MCC is found, the better the chances of successful treatment. That’s why seeing a doctor as soon as you notice any unusual skin changes is so important.
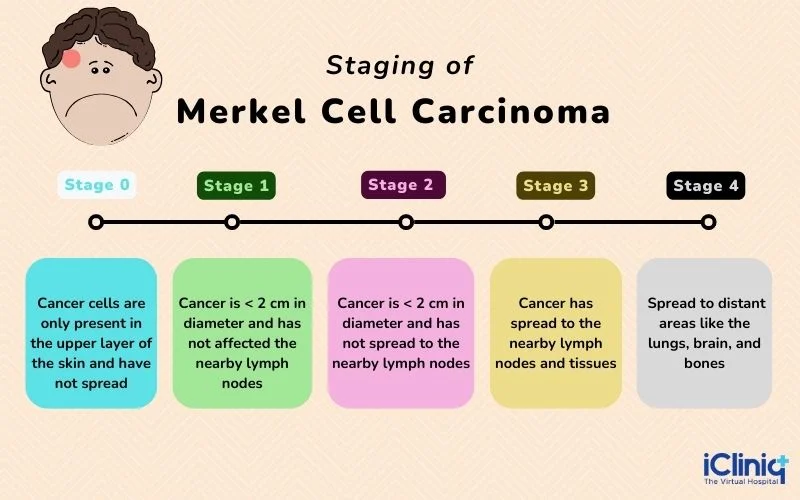
How Does Staging Affect Treatment?
The stage of Merkel Cell Carcinoma (MCC) plays a big role in deciding which treatment is best. Early-stage MCC (Stages 0, I, and II) is usually treated with surgery to remove the tumor, often followed by radiation therapy to destroy any remaining cancer cells and reduce the risk of recurrence.
In Stage III, where the cancer has spread to nearby lymph nodes, treatment often includes surgery to remove both the tumor and affected lymph nodes, followed by radiation therapy. In some cases, immunotherapy or chemotherapy may also be recommended to help the immune system fight any remaining cancer. For Stage IV MCC, where the cancer has spread to distant organs, treatment focuses on controlling the disease and improving quality of life. Immunotherapy is the main treatment, as it helps the body’s immune system attack cancer cells. Chemotherapy may be used in some cases, but immunotherapy has shown better long-term results.
Treatment Options
The primary treatment options include surgery, radiation therapy, chemotherapy, and immunotherapy. Each modality has its own benefits and limitations, and often, a combination of these treatments is employed to achieve the best outcomes.The choice of treatment depends on the stage of the cancer, whether it has spread, and overall health.
Surgery
Surgery is usually the first treatment for early-stage MCC (Stages 0, I, and II). The goal is to remove the cancerous tumor along with some surrounding healthy tissue to ensure all cancer cells are taken out. If the cancer has spread to nearby lymph nodes, those may also be removed in a procedure called a lymph node dissection. Surgery is a quick and effective way to remove localized cancer, but MCC has a high chance of returning, so additional treatments like radiation or immunotherapy may be recommended.
Radiation Therapy
Radiation therapy uses high-energy rays to kill cancer cells that may have been left behind after surgery. It is often used to reduce the risk of recurrence in the same area where the tumor was removed. If surgery is not possible, radiation may be used as the main treatment to shrink the tumor. Radiation is a targeted treatment, meaning it only affects the specific area being treated, unlike chemotherapy, which affects the whole body. However, it can cause skin irritation, fatigue, and swelling in the treated area.
Chemotherapy
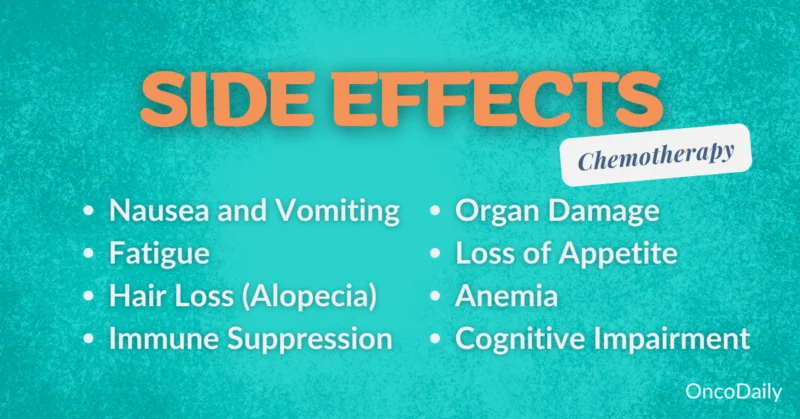
Chemotherapy is a traditional cancer treatment that uses strong drugs to kill rapidly growing cancer cells. It is usually given through an IV (intravenous infusion) and travels throughout the body.
While chemotherapy can shrink tumors, especially in advanced MCC (Stage IV), it is not as effective as immunotherapy for long-term control. It also comes with more side effects, including nausea, hair loss, and a weakened immune system. Because of this, doctors now prefer immunotherapy over chemotherapy in most cases.
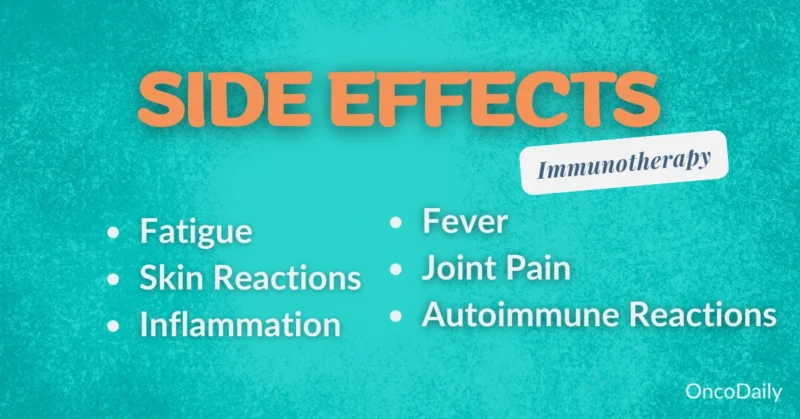
Immunotherapy
Immunotherapy has become one of the most important new treatments for MCC, especially in advanced cases where the cancer has spread. It works by helping the immune system recognize and attack cancer cells. Drugs like Avelumab (Bavencio) and Pembrolizumab (Keytruda) are commonly used for MCC. Unlike chemotherapy, which kills both cancer and healthy cells, immunotherapy specifically targets the cancer, often leading to better long-term results. However, it can cause immune-related side effects, such as inflammation in organs like the lungs or liver.
Myths and Misconceptions About MCC
Because Merkel Cell Carcinoma (MCC) is a rare type of skin cancer, there are many myths and misconceptions about it. Understanding the truth about MCC can help patients recognize the importance of early detection and treatment.
- MCC Is Just Another Skin Cancer and Isn’t That Serious: MCC is one of the most aggressive types of skin cancer. Unlike basal cell carcinoma or squamous cell carcinoma, which grow slowly, MCC spreads quickly to lymph nodes and other organs if not treated early. That’s why early detection and treatment are crucial.
- MCC Only Affects Older Adults: While MCC is more common in people over 50, younger individuals can also develop it, especially if they have a weakened immune system. No matter your age, any new lump or skin change should be checked by a doctor.
- MCC Is Always Caused by Too Much Sun Exposure: While sun exposure increases the risk, MCC can also be caused by the Merkel Cell Polyomavirus, which is present in many cases. People with weakened immune systems (due to organ transplants, HIV, or autoimmune diseases) are also at a higher risk.
- MCC Always Causes Pain: MCC is often painless, which can make it easy to ignore. Many patients don’t feel discomfort, even as the lump grows. That’s why it’s important to watch for any unusual bumps, swelling, or skin changes, even if they don’t hurt.
- If the Lump Is Small, It’s Not Cancer: MCC often starts as a small, firm lump that grows quickly. Even if a bump seems harmless at first, any fast-growing or changing lump should be checked by a doctor.
- MCC Is Untreatable and Always Fatal: While MCC can be aggressive, it is treatable, especially if caught early. Treatments like surgery, radiation, and immunotherapy have improved survival rates. Many patients respond well to treatment and live for many years after diagnosis.
Preventing Merkel Cell Carcinoma
While Merkel Cell Carcinoma (MCC) can’t always be prevented, there are ways to lower the risk. Protecting your skin from the sun is one of the most important steps—using sunscreen, wearing protective clothing, and avoiding tanning beds can help reduce UV damage.
Regular skin checks are also essential, as MCC often appears as a painless, fast-growing lump. Catching any unusual changes early can make treatment more effective. A strong immune system plays a role in reducing the risk of MCC. Eating a healthy diet, exercising, and avoiding smoking or excessive alcohol use can help keep your body strong. People with weakened immune systems, such as those on immunosuppressive medications, should be especially cautious and have regular check-ups. While MCC is rare, staying aware of your skin and overall health can improve early detection and outcomes. If you notice any unusual lumps or skin changes, seeing a doctor right away is the best way to stay protected.
You Can Watch More on OncoDaily Youtube TV
Written by Toma Oganezova, MD
FAQ
What is Merkel Cell Carcinoma (MCC)?
Merkel Cell Carcinoma (MCC) is a rare but aggressive type of skin cancer that develops in Merkel cells, which are found in the top layer of the skin.
What does Merkel Cell Carcinoma look like?
MCC usually appears as a firm, painless, red, pink, or purple lump that grows quickly, often on sun-exposed areas like the face, neck, or arms.
How common is Merkel Cell Carcinoma?
MCC is rare, with about 3,000 new cases diagnosed in the U.S. each year. It is most common in people over 50 and those with weakened immune systems.
What causes Merkel Cell Carcinoma?
MCC is linked to excessive sun exposure, a weakened immune system, and the Merkel Cell Polyomavirus, which is found in many cases of the disease
Is Merkel Cell Carcinoma more dangerous than other skin cancers?
Yes, MCC is more aggressive than common skin cancers like basal cell carcinoma and squamous cell carcinoma. It can spread quickly to lymph nodes and other organs
How is Merkel Cell Carcinoma diagnosed?
Doctors diagnose MCC through a skin biopsy, where a tissue sample is taken and examined. Imaging tests like CT or PET scans may be used to check for spreading.
What are the treatment options for Merkel Cell Carcinoma?
Treatment options include surgery, radiation therapy, chemotherapy, and immunotherapy. The choice depends on the stage and spread of the cancer.
Can Merkel Cell Carcinoma be prevented?
While not always preventable, reducing sun exposure, wearing sunscreen, and maintaining a healthy immune system can lower the risk of developing MCC.
Is Merkel Cell Carcinoma curable?
If detected early, MCC can be treated successfully. However, because it spreads quickly, early diagnosis and treatment are crucial for better outcomes.
What is the survival rate for Merkel Cell Carcinoma?
Survival rates depend on the stage at diagnosis. Early-stage MCC has a higher survival rate, while advanced-stage MCC is more difficult to treat.