Bladder cancer is one of the most common cancers, particularly affecting men over the age of 55. Chemotherapy remains a cornerstone in the treatment of bladder cancer, especially for patients with advanced stages of the disease or muscle-invasive forms. Understanding the bladder cancer chemotherapy success rate is critical for patients, clinicians, and caregivers, as it provides insight into the effectiveness of various treatment options. This article explores the chemotherapy success rates for bladder cancer, highlighting the different treatment approaches, patient outcomes, and the factors that influence treatment efficacy.

Also Read About Bladder Cancer Cure Rate on OncoDaily
Chemotherapy in Bladder Cancer: An Overview
Bladder cancer can present in different stages, ranging from localized superficial tumors to advanced cancer that has spread beyond the bladder. Chemotherapy is used in several settings, either alone or in combination with other therapies such as surgery or immunotherapy. For muscle-invasive and metastatic bladder cancer, chemotherapy is particularly important as it can significantly affect survival outcomes. The success of chemotherapy, however, is highly dependent on the stage of the cancer, the patient’s overall health, and the specific chemotherapy regimen employed.
Neoadjuvant and Adjuvant Chemotherapy
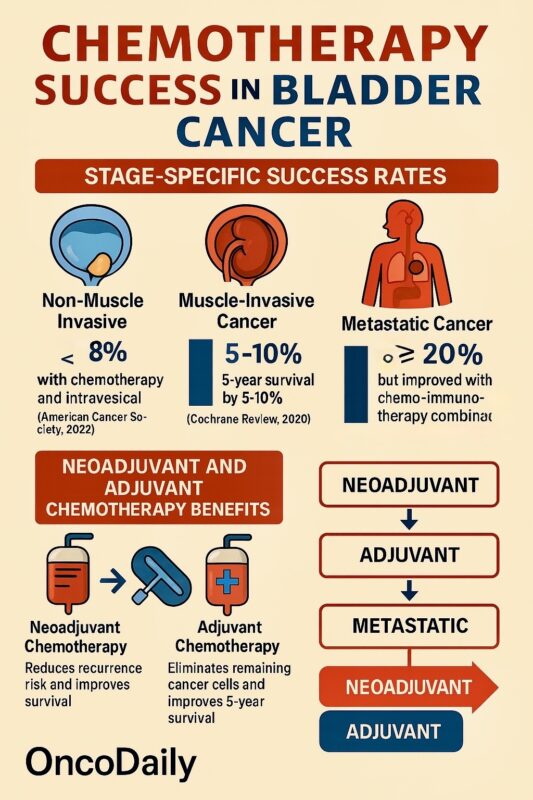
Neoadjuvant chemotherapy, administered before surgery, is commonly recommended for patients with muscle-invasive bladder cancer. Its goal is to shrink tumors and improve the success of subsequent surgeries. Multiple studies have demonstrated that patients who receive neoadjuvant chemotherapy experience better overall survival compared to those who undergo surgery alone (Advanced Bladder Cancer [ABC] trial, 2018). In particular, neoadjuvant chemotherapy has been shown to reduce the risk of cancer recurrence and improve long-term outcomes, with survival rates increasing by up to 10% in some cases.
Adjuvant chemotherapy, given after surgery, aims to eliminate any remaining cancer cells and reduce the risk of recurrence. This approach is typically employed when cancer has spread to the lymph nodes or surrounding tissues. Research has consistently shown that adjuvant chemotherapy improves survival outcomes in patients who have undergone cystectomy (Bladder Cancer: The Complete Guide, 2017). These patients have a markedly improved five-year survival rate, which is higher than that of those who did not receive chemotherapy post-surgery.
Chemotherapy for Metastatic Bladder Cancer
Chemotherapy is also the primary treatment for advanced or metastatic bladder cancer. In these cases, chemotherapy is used to control the disease, prolong survival, and improve the patient’s quality of life. Regimens such as cisplatin and gemcitabine are frequently used, often in combination with immunotherapies. Although chemotherapy does not offer a cure for metastatic bladder cancer, it can still extend life significantly, with some patients achieving partial or complete remission (National Cancer Institute, 2021). The median overall survival for patients receiving chemotherapy for metastatic disease is typically around 15–18 months, although this varies widely based on individual health factors and the specific chemotherapy combination.
Success Rates of Chemotherapy
The success of chemotherapy in bladder cancer treatment is largely determined by the stage at which the cancer is diagnosed. For non-muscle invasive bladder cancer, the prognosis is generally good, especially when detected early. In these cases, chemotherapy, combined with intravesical therapies, can have cure rates of 80% or higher (American Cancer Society, 2022). However, the bladder cancer chemotherapy success rate drops significantly as the cancer progresses.
For patients with muscle-invasive bladder cancer, chemotherapy can provide a significant benefit when used as part of a neoadjuvant regimen before surgery. Studies indicate that neoadjuvant chemotherapy can increase the five-year survival rate by 5–10% (Cochrane Review, 2020). These findings highlight the effectiveness of chemotherapy in reducing the risk of recurrence following cystectomy, the primary surgical procedure for muscle-invasive bladder cancer.
In advanced and metastatic bladder cancer, chemotherapy success rates are lower, with five-year survival rates typically under 20%. However, in the metastatic setting, newer combinations of chemotherapy and immunotherapy have led to improvements in progression-free survival, allowing patients to live longer with manageable symptoms. Research on combining chemotherapy with immune checkpoint inhibitors has shown promising results in increasing overall survival in these patients (Clinical Cancer Research, 2021).
Factors Affecting Chemotherapy Success
Several factors can influence the success of chemotherapy in bladder cancer. The stage of cancer is one of the most significant. Earlier stages generally have higher chemotherapy success rates. Patients with localized disease, especially those with non-muscle invasive cancer, tend to have better outcomes with chemotherapy alone or combined with other therapies like immunotherapy.
Patient-related factors such as age, comorbidities, and overall health also play a vital role in determining treatment effectiveness. Younger patients or those without significant health issues tend to have better responses to chemotherapy. Furthermore, specific genetic and molecular characteristics of the tumor can impact how well a patient responds to chemotherapy. For instance, tumors with certain genetic mutations may be more resistant to standard chemotherapy drugs, making alternative therapies necessary (Journal of Clinical Oncology, 2020).
Additionally, the type of chemotherapy regimen used influences outcomes. Cisplatin-based regimens, for example, remain the gold standard in muscle-invasive and metastatic bladder cancer, offering higher response rates than other combinations. However, not all patients are eligible for cisplatin due to its toxic side effects, which can lead oncologists to use less aggressive alternatives with varying success rates.
Side Effects and Management
Chemotherapy for bladder cancer is not without its side effects. Common side effects include nausea, fatigue, hair loss, and increased susceptibility to infections. These side effects can impact a patient’s quality of life but are often manageable with supportive care. Newer medications have been developed to mitigate some of these side effects, and patients are encouraged to discuss any symptoms with their healthcare team for optimal management.
Conclusion
Chemotherapy plays a crucial role in the treatment of bladder cancer, offering substantial benefits in improving survival rates, especially when used at earlier stages. However, its success is influenced by a variety of factors, including cancer stage, patient health, and the specific chemotherapy regimen used. While chemotherapy alone may not always provide a cure, it can extend life and improve the quality of life for many patients.
Patients diagnosed with bladder cancer should have an open discussion with their oncologist about the potential benefits and risks of chemotherapy. With advancements in treatment options, including the integration of immunotherapy, the outlook for patients with bladder cancer continues to improve.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD