What is Insulinoma?
Insulinoma is a rare neuroendocrine tumor originating from the pancreas’s insulin-producing beta cells. These tumors are responsible for the excessive secretion of insulin, leading to recurrent episodes of hypoglycemia, which can have severe and potentially life-threatening consequences if left untreated. Tumors are the most common functioning pancreatic neuroendocrine tumors, accounting for approximately 1-4 cases per million people per year.
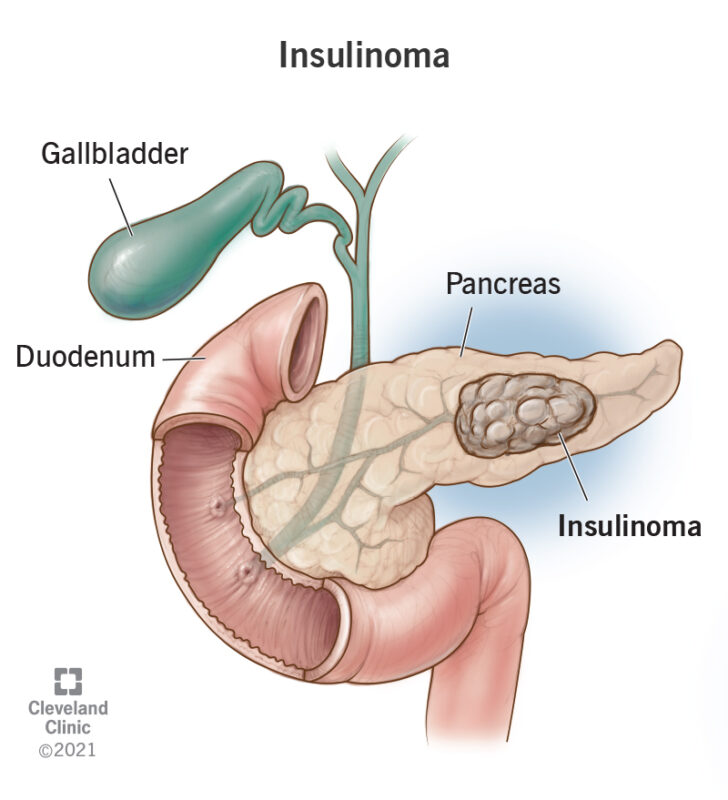
This image is taken from my.clevelandclinic.org
Causes and Risk Factors of Insulinoma
- Genetic Syndromes:
- Multiple endocrine neoplasia type 1 (MEN1) syndrome: This inherited condition raises the risk of pancreatic and other NETs, including tumors.
- Von Hippel-Lindau (VHL) syndrome: This condition causes mutations to the VHL gene that may result in pancreatic NETs.
- Neurofibromatosis type 1 (NF1) syndrome: Changes to the NF1 gene cause a small portion of pancreatic NETs.
- Tuberous sclerosis: This condition causes tumors to develop.
- Age: The most common age range for a diagnosis of pancreatic NETs such as is between 50 and 60 years old.
- Smoking: Smoking increases the risk of developing tumors.
- Alcohol: Heavy drinking has been associated with an increase in pancreatic NETs.
- Diabetes: People with diabetes, a condition that makes blood sugar levels increase, are at increased risk of tumors and other pancreatic NETs.
- Family History: If a close relative has or has had cancer, the risk increases.
- Other Factors: The exact cause of insulinomas remains unknown, but patients with certain genetic syndromes are more likely to develop NETs due to specific DNA mutations.
These risk factors can increase the likelihood of developing tumor, but there is no way to know for sure whether it will happen.
Symptoms of Insulinoma
The hallmark of the tumor is the development of recurrent episodes of hypoglycemia, which can manifest with a variety of symptoms. The most common symptoms associated with insulinoma include:
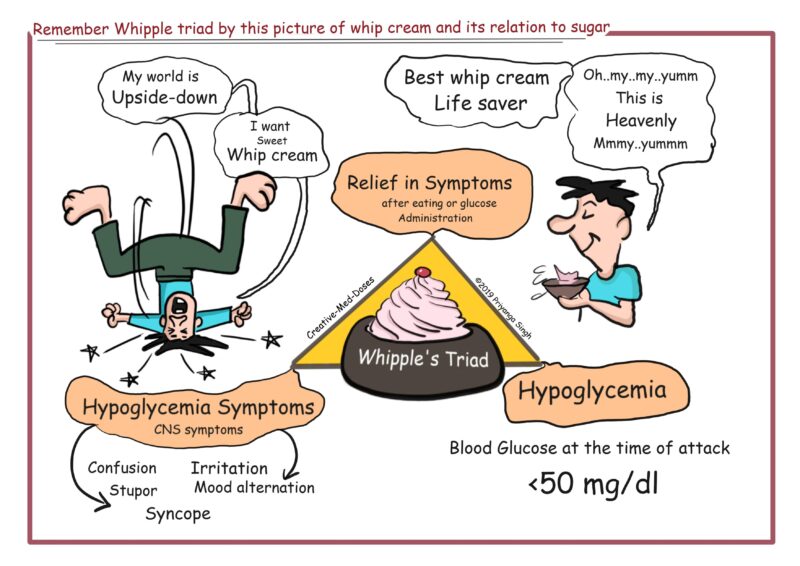
This image is taken from Creativemeddoses.com
- Neuroglycopenic symptoms:
- Confusion
- Dizziness
- Blurred vision
- Seizures
- Coma
- Adrenergic symptoms:
- Sweating
- Tremors
- Palpitations
- Anxiety
- Gastrointestinal symptoms:
- Nausea
- Vomiting
- Abdominal pain
Patients with tumors often experience these symptoms, particularly during fasting or after physical exertion, as the tumor’s excessive insulin secretion leads to an inability to maintain normal blood glucose levels. In some cases, patients may also report weight gain, which can be a consequence of the hyperinsulinemic state. It is important to note that the severity and frequency of symptoms can vary among individuals, and some patients may have atypical presentations or experience only mild symptoms. In rare instances, tumors may also secrete other hormones, such as glucagon or somatostatin, leading to additional clinical manifestations.
Diagnosis of Insulinoma
The diagnosis of a tumor involves a series of tests and procedures to confirm the presence of the tumor and its associated hyperinsulinism. The diagnostic process includes:
- Symptoms and Clinical Evaluation:
- Patients may present with symptoms of hypoglycemia, such as confusion, sweating, weakness, and palpitations, which can prompt further investigation.
- A thorough clinical evaluation, including a detailed medical history and physical examination, is essential to assess the patient’s symptoms and overall health status.
- Blood Tests:
- Measurement of glucose and insulin levels during symptoms of hypoglycemia is crucial for diagnosing tumor.
- A fasting blood test is often performed to assess glucose and insulin levels, with low blood glucose levels (<55 mg/dL) and elevated insulin levels suggestive of hyperinsulinism.
- Endoscopic Ultrasound:
- Endoscopic ultrasound is a valuable imaging modality with high sensitivity for locating tumors within the pancreas.
- This procedure allows for detailed visualization of the pancreas and the identification of any abnormal lesions or tumors.
- Imaging Studies:
- Computed tomography (CT) and magnetic resonance imaging (MRI) are non-invasive imaging techniques used to localize suspected insulinomas and assess for metastases.
- These imaging modalities provide detailed anatomical information and help guide treatment planning.
- Functional Tests:
- Invasive modalities, such as arterial stimulation venous sampling (ASVS), can be used to accurately localize insulinomas preoperatively.
- ASVS involves injecting calcium into the arteries supplying the pancreas to stimulate insulin release, followed by sampling blood from the hepatic vein to identify the site of pathological insulin secretion.
- Biopsy:
- In some cases, a biopsy may be performed to obtain tissue samples for histological analysis and to confirm the presence of tumors.
- Biopsies can help differentiate insulinomas from other pancreatic lesions and guide treatment decisions.
The diagnosis of tumors requires a comprehensive approach, combining clinical evaluation, biochemical testing, imaging studies, and, in some cases, invasive procedures to accurately identify and localize the tumor. Timely and accurate diagnosis is essential for initiating appropriate treatment and improving patient outcomes.
Treatment of Insulinoma
The primary treatment for tumors is surgical resection of the tumor, which is the only curative option. The specific surgical approach depends on the location and size of the tumor, as well as the presence of any metastatic disease.
- Surgery:
-
- Surgery is the mainstay of treatment for insulinoma, aiming to remove the tumor and preserve pancreatic function.
- Surgical options include enucleation for small tumors, distal pancreatectomy for tumors in the body or tail of the pancreas, and Whipple procedure for tumors in the head of the pancreas.
- The extent of surgery depends on the size, location, and number of tumors, as well as the presence of metastases.
- Medical management:
- Diazoxide is the drug of choice for managing insulinoma, as it inhibits insulin release from the tumor.
- In cases where patients are unresponsive or intolerant to diazoxide, somatostatin analogs like octreotide and lanreotide may be used to prevent hypoglycemia.
- Other medications, such as verapamil, diphenylhydantoin, and steroids like prednisolone, can also help control blood sugar levels.
- Liver-directed therapies:
- Radiofrequency ablation (RFA) and transarterial embolization (TAE) are procedures that can target and treat liver metastases in cases of advanced insulinoma.
- Systemic therapies:
- Chemotherapy may be considered for metastatic insulinoma, although its efficacy is limited.
- Targeted therapies like everolimus, which inhibits cell proliferation and angiogenesis, are indicated for progressive neuroendocrine tumors located in the pancreas.
The choice of treatment approach depends on various factors, including the size and location of the tumor, the presence of metastases, the patient’s overall health, and the availability of specialized expertise. A multidisciplinary team, including endocrinologists, surgeons, oncologists, and interventional radiologists, is often involved in the management of insulinoma patients to ensure a comprehensive and personalized treatment plan.
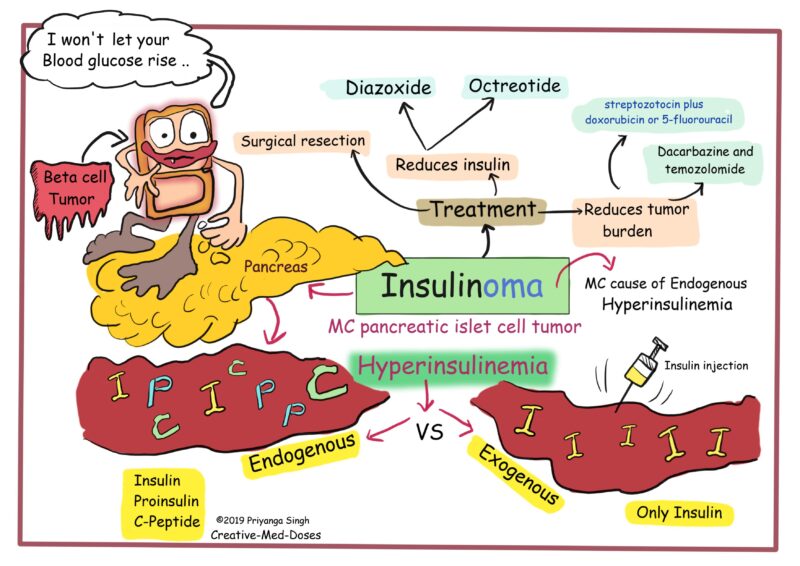
This image is taken from Creativemeddoses.com.
Prognosis and Survival
- Benign Insulinomas:
- The 10-year survival rate for patients with benign tumors who undergo successful surgical removal is around 88%.
- Approximately 87.5% of patients with benign tumors are considered cured (free of symptoms for at least six months) after surgery.
- Malignant Insulinomas:
- The prognosis for patients with malignant tumors is less favorable compared to those with benign tumors.
- The 10-year survival rate for patients with metastatic or malignant tumors is reported to be around 29%.
- In a more recent study, the 5-year survival rate for patients with metastatic insulinoma improved to 55.6%.
- Factors Affecting Prognosis:
- The presence of metastases at diagnosis is a key factor that negatively impacts the prognosis of tumor patients.
- Patients with multiple endocrine neoplasia type 1 (MEN1) syndrome or other genetic syndromes associated with insulinomas tend to have a higher rate of malignant tumors and poorer outcomes.
- Larger tumor size (>3 cm) and higher tumor grade (G2 or G3) are also associated with a worse prognosis.
- Perioperative Mortality:
- The perioperative mortality rate, defined as any death occurring within 30 days after surgery, is reported to be around 2.7%.
In summary, the prognosis for patients with benign tumors is generally favorable, with high long-term survival rates after successful surgical treatment. However, patients with malignant or metastatic insulinomas have a significantly poorer prognosis, although recent advancements in treatment options have shown some improvement in survival outcomes.
Challenges and Considerations
Insulinoma presents several unique challenges in its management, which healthcare providers must be aware of to provide optimal care for these patients.
Diagnostic Challenges:
- Insulinoma presents with a wide range of symptoms that can mimic other conditions, leading to delays in diagnosis and potentially inappropriate treatments.
- The rarity of insulinoma and the variability in symptom presentation can make it challenging to recognize and differentiate from other disorders.
Localization of Tumor:
- Identifying the precise location of the insulinoma within the pancreas is crucial for surgical planning and successful tumor removal.
- Various imaging modalities and localization techniques are used, such as multiphase computed tomography (CT) and selective arterial calcium stimulation test, to pinpoint the tumor accurately.
Surgical Management:
- Surgical resection is the primary treatment for insulinoma, but the decision to proceed with surgery can be complex, especially in cases where the tumor is small, multiple, or located near critical structures.
- Balancing the risks and benefits of surgery, particularly in the context of potential complications and the need for postoperative care, requires careful consideration.
Resource Limitations:
- Managing rare disorders like insulinoma in resource-challenged environments, as seen in many countries in sub-Saharan Africa, presents significant challenges.
- Limited availability of investigations, treatments, and healthcare infrastructure can hinder the timely diagnosis and optimal management of insulinoma in these settings.
Delayed Diagnosis:
- Unusual presentations of insulinoma, such as seizures, can lead to misdiagnosis and delays in appropriate treatment, resulting in increased morbidity and mortality.
- The atypical symptoms and variable duration of symptoms before diagnosis contribute to the challenges in promptly identifying and managing insulinoma.
During Treatment
Common side effects include
- Diazoxide (a medication used to manage insulinoma):
- Peripheral edema (fluid buildup in the legs or other body parts)
- Hyperuricemia (high uric acid levels)
- Hirsutism (excessive hair growth)
- Nausea
- Elevated uric acid levels
- Thrombocytopenia (low platelet count)
- Somatostatin Analogues (e.g., octreotide, lanreotide):
- Gastrointestinal bloating
- Abdominal cramping
- Malabsorption
- Cholelithiasis (gallstone formation)
- Decreased glucagon and growth hormone levels, which can worsen hypoglycemia in some patients
- Surgical Complications:
- Bleeding
- Infection
- Pain
- Pancreatic fistula (leakage of pancreatic fluid)
- Low digestive enzyme levels (if a large part of the pancreas is removed)
- Chemotherapy (for metastatic or advanced insulinoma):
- The specific side effects depend on the chemotherapeutic agents used, but they may include nausea, fatigue, hair loss, and bone marrow suppression.
Management Strategies
- Surgical Management:
- Surgical resection is the primary treatment for insulinoma, aiming to remove the tumor and preserve pancreatic function.
- The choice of surgical approach depends on the tumor’s location, size, and the patient’s overall health status.
- Medical Management:
- Diazoxide is a medication used to manage insulinoma by inhibiting insulin secretion from pancreatic beta cells and increasing hepatic glucose production.
- Somatostatin analogs like octreotide and lanreotide can also be used to control hypoglycemia and manage symptoms.
- Liver-Directed Therapies:
- For patients with liver metastases, liver-directed therapies like chemoembolization or radiofrequency ablation (RFA) can be used to target and treat the tumors.
- Systemic Therapies:
- Chemotherapy may be considered for metastatic or advanced insulinoma, although its efficacy is limited.
- Follow-Up Care:
- Regular follow-up appointments and monitoring are essential to assess treatment response, manage symptoms, and detect any recurrence or progression of the disease.
- Multidisciplinary Approach:
- A multidisciplinary team, including endocrinologists, surgeons, oncologists, and other specialists, collaborates to develop the most appropriate treatment plan for each patient.
These management strategies aim to control hypoglycemia, manage symptoms, and improve patient outcomes for individuals with insulinoma.
After Treatment
Follow-up Care
- Frequency of Follow-up:
- After surgery, patients typically have an appointment with their doctor or specialist nurse within 2-6 weeks of being discharged.
- Thereafter, follow-up appointments are scheduled every 3-6 months, especially for patients who have insulinoma that has spread to other parts of the body.
- Patients who had successful surgical removal of the insulinoma may have less frequent follow-up visits.
- Monitoring and Assessments:
- During follow-up appointments, the doctor or nurse will examine the patient, ask about any symptoms or side effects, and order relevant blood tests.
- Patients are encouraged to contact their healthcare team between appointments if they have any new concerns or symptoms.
- Multidisciplinary Approach:
- The follow-up care for insulinoma patients often involves a multidisciplinary team, including endocrinologists, surgeons, oncologists, and other specialists.
- Importance of Adherence:
- Consistent follow-up and adherence to the recommended schedule are crucial for early detection of any recurrence or complications, allowing for timely intervention.
- Individualized Care:
- The frequency and duration of follow-up are tailored to the individual patient’s needs and the specific characteristics of their insulinoma.
By maintaining regular follow-up care, patients with insulinoma can be closely monitored, and any issues or concerns can be addressed promptly, ultimately improving their overall health outcomes.