Meningiomas are tumors that arise from the meninges, the protective membranes surrounding the brain and spinal cord. While these tumors are more common in adults, they can also occur in children, a condition known as pediatric meningioma. These tumors are typically slow-growing and benign, but they can cause significant symptoms and complications due to their location and potential for compression of surrounding brain structures.
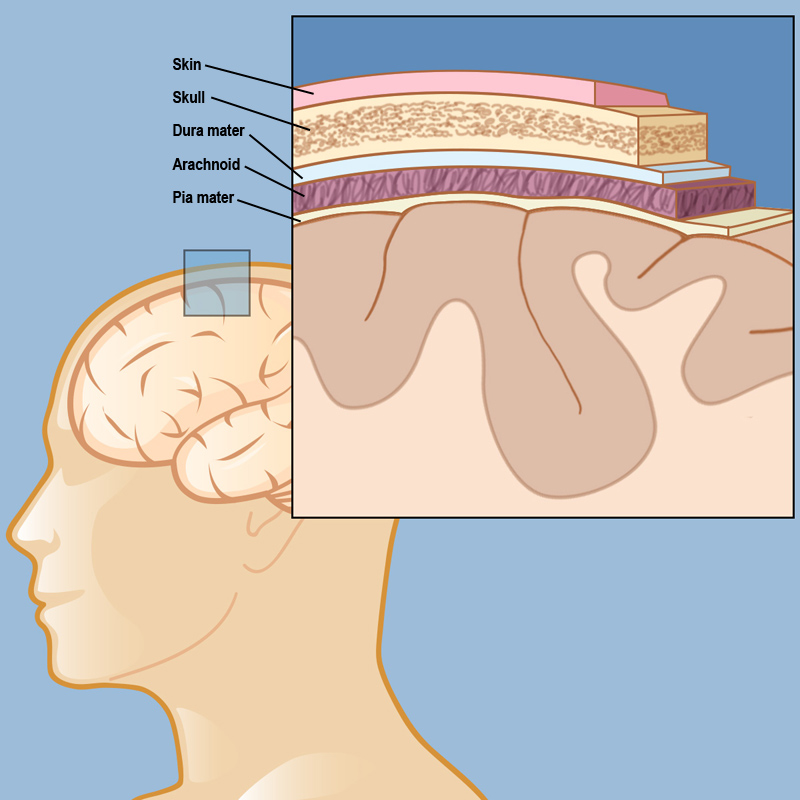
The meninges. The image is taken from neurosurgery.weillcornell.org.
Prevalence and Epidemiology
Pediatric meningiomas are relatively rare, accounting for approximately 0.4% to 4.6% of all primary brain tumors in children. Unlike adult meningiomas, which are more common in females, pediatric meningiomas affect males and females equally. The median age at presentation is around 13 years, with infantile cases (less than 1 year of age) representing less than 4% of cases.
Causes and Risk Factors
The exact cause of these tumors is not fully understood, but several risk factors have been identified:
- Radiation exposure: Exposure to ionizing radiation, particularly in childhood, is a well-established risk factor for developing meningiomas later in life.
- Genetic conditions: Certain genetic conditions, such as neurofibromatosis type 2 (NF2), are associated with an increased risk of developing meningiomas, particularly in children.
- Hormonal factors: Some studies have suggested that hormonal factors, such as estrogen levels, may play a role in the development of meningiomas, although the evidence is not conclusive.
- Environmental factors: Exposure to certain chemicals, such as vinyl chloride and ionizing radiation, has been linked to an increased risk of meningiomas, but more research is needed to establish a clear causal relationship.
Symptoms
The symptoms of pediatric meningioma can vary depending on the tumor’s location, size, and rate of growth. Some common symptoms include:
- Headaches: Persistent or worsening headaches, often more severe in the morning, can be a sign of increased intracranial pressure caused by the tumor.
- Seizures: Meningiomas can cause seizures, especially if they are located in or near the cerebral cortex.
- Visual disturbances: Tumors located near the optic nerves or optic chiasm can cause vision problems, such as blurred vision, double vision, or loss of peripheral vision.
- Hearing loss or tinnitus: Meningiomas near the auditory nerves or temporal lobe can lead to hearing impairment or ringing in the ears.
- Cognitive and behavioral changes: Depending on the tumor’s location, children may experience changes in memory, concentration, personality, or behavior.
- Weakness or numbness: Tumors compressing certain areas of the brain or spinal cord can cause weakness or numbness in the arms, legs, or other parts of the body.
- Hormonal imbalances: Meningiomas near the pituitary gland or hypothalamus can disrupt hormone production, leading to symptoms such as growth problems, precocious puberty, or other endocrine disorders.
It’s important to note that some children with meningiomas may not exhibit any symptoms, especially in the early stages of tumor growth. Regular follow-up and monitoring are crucial for early detection and intervention.
Diagnosis
The diagnosis of pediatric meningioma typically involves a combination of imaging tests and, in some cases, a biopsy:
- Magnetic Resonance Imaging (MRI): MRI is the preferred imaging modality for detecting and characterizing meningiomas. It can provide detailed images of the tumor’s location, size, and relationship to surrounding brain structures.
- Computed Tomography (CT) scan: CT scans can also be used to detect meningiomas, particularly if they have calcifications or bony involvement.
- Biopsy: In some cases, a biopsy may be necessary to confirm the diagnosis and determine the tumor’s grade. This involves surgically removing a small sample of the tumor tissue for microscopic examination by a pathologist.
- Molecular and genetic testing: Advances in molecular and genetic testing have allowed for more accurate classification and characterization of meningiomas, which can guide treatment decisions.
Meningioma Treatment Options
The treatment of pediatric meningioma depends on various factors, including the tumor’s grade, location, size, and the child’s overall health. The primary treatment options include:
- Surgery: Surgical resection, or removal of the tumor, is often the first-line treatment for symptomatic or growing meningiomas. The goal is to remove as much of the tumor as possible while minimizing damage to surrounding brain tissue. Advances in neurosurgical techniques, such as image-guided surgery and intraoperative imaging, have improved the safety and effectiveness of meningioma resection.
- Radiation therapy: Different types of radiation therapy may be used, including external beam radiation therapy (EBRT), stereotactic radiosurgery (SRS), or proton beam therapy, depending on the tumor’s location and the child’s age and overall health. Radiation therapy may be used in several scenarios:
- As an adjuvant treatment after surgery to target any remaining tumor cells and reduce the risk of recurrence.
- As the primary treatment for tumors that are inoperable or located in areas where surgery would be too risky.
- For the treatment of recurrent or residual tumors.
- Chemotherapy: While chemotherapy is not a standard treatment for meningiomas, it may be considered in cases of recurrent or aggressive tumors that do not respond to other treatments.
- Targeted therapies: Ongoing research is exploring the use of targeted therapies, such as anti-angiogenic agents or molecular targeted drugs, for the treatment of meningiomas. These therapies aim to target specific molecular pathways involved in tumor growth and progression.
- Immunotherapy: Immunotherapy, particularly immune checkpoint inhibitors is being tested for its efficacy in treating recurrent and progressive meningiomas. Early-phase clinical trials are evaluating the potential of these therapies to enhance the immune system’s ability to recognize and attack tumor cells. Combining immunotherapy with other treatment modalities, such as radiation therapy, may offer synergistic effects and improve outcomes for patients with aggressive or treatment-resistant meningiomas.
- Supportive care: In addition to the primary treatments, supportive care measures may be necessary to manage symptoms and improve the child’s quality of life. These may include medications for seizure control, physical therapy, occupational therapy, speech therapy, and psychological support.
More information about completed and ongoing clinical trials for pediatric meningiomas can be found here – clinicaltrials.gov
Patient Experience
With advances in treatment and supportive care, the survival rates for children with meningiomas have improved significantly. However, survivors may face various challenges during and after treatment, including:
- Physical challenges: Depending on the tumor’s location and the treatment received, children may experience physical limitations, such as weakness, paralysis, or sensory deficits. Rehabilitation services, including physical therapy, occupational therapy, and speech therapy, can help address these challenges and improve functional outcomes.
- Cognitive and neurodevelopmental challenges: Meningiomas and their treatments can impact cognitive function, learning, and neurodevelopment. Neuropsychological assessments and interventions, such as educational support and cognitive rehabilitation, may be necessary to address these challenges.
- Psychosocial challenges: Children and their families may experience emotional distress, anxiety, depression, and social isolation during and after treatment. Counseling, support groups, and psychosocial interventions can help address these challenges and promote overall well-being.
- Late effects and long-term follow-up: Survivors of pediatric meningioma may be at risk for long-term complications, such as endocrine disorders, vision or hearing problems, and secondary cancers. Regular follow-up and monitoring are essential to detect and manage these potential late effects.
- Transition to adult care: As children with meningiomas reach adulthood, they may need to transition from pediatric to adult healthcare services. Proper planning and coordination are crucial to ensure continuity of care and support during this transition.
Problems During and After Treatment and How to Manage Them
Patients and caregivers should be aware of potential problems that may arise during and after treatment for pediatric meningioma and how to manage them effectively:
- Surgical complications: Potential complications of meningioma surgery include bleeding, infection, cerebrospinal fluid leaks, and neurological deficits. Close monitoring and prompt management of these complications are essential.
- Radiation side effects: Radiation therapy can cause side effects such as fatigue, skin irritation, nausea, and cognitive changes. Supportive care measures, such as medications and counseling, can help manage these side effects.
- Chemotherapy side effects: If chemotherapy is used, patients may experience side effects such as nausea, vomiting, hair loss, and increased risk of infections. Supportive care measures, including anti-nausea medications, nutritional support, and infection prevention strategies, can help manage these side effects.
- Endocrine disorders: Meningiomas near the pituitary gland or hypothalamus can disrupt hormone production, leading to conditions such as growth hormone deficiency, precocious puberty, or other endocrine disorders. Regular monitoring and appropriate hormone replacement therapy may be necessary.
- Vision and hearing problems: Tumors or treatments that affect the optic nerves, auditory nerves, or related brain structures can lead to vision or hearing impairments. Regular assessments and interventions, such as vision therapy or hearing aids, can help manage these problems.
- Cognitive and neurodevelopmental challenges: As mentioned earlier, cognitive and neurodevelopmental challenges may arise due to the tumor or its treatment. Ongoing assessments, educational support, and cognitive rehabilitation can help address these challenges.
- Psychosocial support: Patients and families may benefit from counseling, support groups, and other psychosocial interventions to cope with the emotional and social challenges associated with meningioma diagnosis and treatment.
- Palliative care: In cases of advanced or recurrent meningiomas that do not respond to treatment, palliative care services can provide symptom management, emotional support, and end-of-life care when needed.
Conclusion
Pediatric meningioma is a rare but potentially serious condition that requires comprehensive care and support. While the prognosis for many children with this tumor is favorable, particularly for low-grade tumors, patients and caregivers should be aware of the potential challenges and complications that may arise during and after treatment.
By understanding the causes, symptoms, diagnosis, and treatment options for pediatric meningioma, as well as the potential problems and strategies for managing them, patients and caregivers can be better prepared to navigate this journey and advocate for the best possible care and support. Regular follow-up, multidisciplinary care, and ongoing research into new and improved treatment modalities are crucial for improving outcomes and quality of life for children with meningiomas and their families.
Resources
- American Cancer Society – cancer.org
- National Cancer Institute – cancer.gov
- American Brain Foundation
- American Society of Clinical Oncology – asco.org
- Children’s Hospital of Philadelphia – chop.edu
- Dana-Farber Cancer Institute
- Pediatric meningiomas: A literature review and diagnostic update. Neuro-Oncology Advances.
- Radiopaedia – radiopedia.org