What is diffuse large B-cell lymphoma?
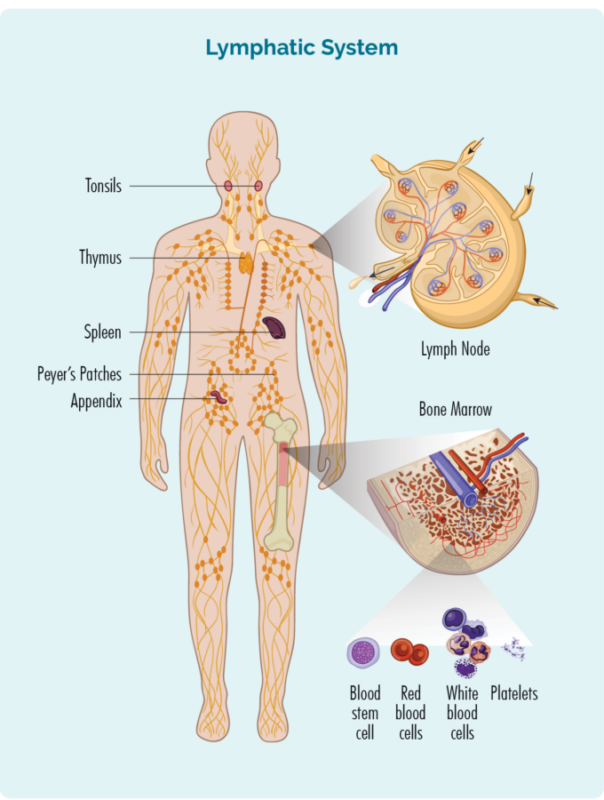
Diffuse large B-cell lymphoma (DLBCL) is an aggressive (fast-growing) form of non-Hodgkin lymphoma that affects B-lymphocytes (B-cells), a type of white blood cell. It can present in both nodal and extranodal sites, with common extranodal involvements including the gastrointestinal tract and skin. It is the most common subtype of non-Hodgkin lymphoma, accounting for about 30-40% of newly diagnosed cases in adults.
Source of image lymphoma.org
Causes and Risk Factors
The exact causes of DLBCL are not fully understood, but several factors have been identified that may contribute to its development:
- Genetic Mutations: Diffuse large B-cell lymphoma occurs when B-cells undergo genetic mutations that lead to uncontrolled growth. These mutations are typically acquired during a person’s lifetime rather than inherited.
- Immune System Dysfunction: A compromised immune system is a significant risk factor. This includes individuals with autoimmune diseases, those who have undergone organ transplants, or those with HIV/AIDS.
- Previous Cancer Treatments: Exposure to chemotherapy and radiation therapy for other cancers can increase the risk of developing DLBCL later in life.
- Infections: Certain viral infections, such as Epstein-Barr virus (EBV) and hepatitis C, have been linked to an increased risk of diffuse large B-cell lymphoma.
Other risk factors that may increase the likelihood of developing DLBCL:
- Age: The incidence of diffuse large B-cell lymphoma increases with age, with most cases diagnosed in individuals over 60 years old.
- Family History: Having a first-degree relative with DLBCL or other types of lymphoma can slightly increase the risk.
- Autoimmune Diseases: Conditions such as rheumatoid arthritis, systemic lupus erythematosus, and Sjögren’s syndrome are associated with a higher risk of DLBCL.
- Immunosuppressive Therapy: Medications used to suppress the immune system, such as those taken after organ transplants, can increase the risk of DLBCL.
- Environmental Exposures: Exposure to certain chemicals, such as benzene, pesticides, and herbicides, has been linked to an increased risk of DLBCL.
- Obesity: Excess body weight and obesity have been associated with a higher risk of developing DLBCL.
Symptoms
Diffuse large B-cell lymphoma (DLBCL) is characterized by a variety of symptoms, which can vary depending on the location and extent of the disease.
Common Symptoms
Swollen Lymph Nodes:
- The most common symptom is painless swelling in the lymph nodes, often noticed in the neck, armpit, or groin.
- These swollen lymph nodes can grow quickly and may form large lumps known as ‘bulky disease’.
B Symptoms:
- Fever (higher than 38ºC).
- Drenching night sweats that soak nightclothes and bedding.
- Unexplained weight loss (at least 10% of body weight over six months).
Other Symptoms
Localized Symptoms:
- Chest or Abdominal Pain: Pain in the chest or stomach area due to swollen lymph nodes pressing against organs.
- Bone Pain: This can occur if the lymphoma affects the bones.
- Skin Lumps: Lymphoma can present as lumps on the skin.
- Coughing or Breathlessness: If the lymphoma is in the chest, it can cause respiratory symptoms.
Extranodal Symptoms:
- DLBCL can develop outside the lymph nodes, affecting organs such as the gastrointestinal tract, skin, thyroid, breast, bone, brain, and others.
- Symptoms depend on the affected area, such as abdominal pain, diarrhea, or bleeding if the gastrointestinal tract is involved.
General Symptoms:
- Fatigue: Extreme tiredness that does not go away with rest.
- Loss of Appetite: General loss of interest in eating.
- Itching: Can be widespread or localized
Diagnosis
The diagnosis of diffuse large B-cell lymphoma (DLBCL) typically involves the following steps:
Biopsy
The main way to diagnose diffuse large B-cell lymphoma is through a biopsy, which involves removing a sample of tissue (usually a lymph node or other affected area) for examination under a microscope. Common biopsy procedures include:
- Excisional or incisional biopsy to remove an entire lymph node or part of a lymph node
- Core needle biopsy using imaging guidance to sample a lymph node or tumor
- Surgical biopsy to obtain a sample from an organ like the stomach or brain
- The biopsy sample is examined microscopically to look for large, abnormal B-lymphocytes that are a hallmark of DLBCL. Immunohistochemistry tests are done on the sample to confirm the cancer cells are of B-cell origin by checking for B-cell markers.
Imaging Tests
Imaging tests are done to determine the extent (stage) of diffuse large B-cell lymphoma in the body :
- Computed tomography (CT) scan
- Positron emission tomography (PET) scan
- Magnetic resonance imaging (MRI) scan to look at the brain/spinal cord
- Bone scan or bone marrow biopsy to check for bone marrow involvement
Blood Tests
Blood tests are performed to evaluate general health and can include :
- Complete blood count (CBC)
- Comprehensive metabolic panel to assess kidney/liver function
- Lactate dehydrogenase (LDH) levels
- Testing for HIV, hepatitis B/C
Lumbar Puncture
A lumbar puncture to collect cerebrospinal fluid may be done if there are signs the lymphoma has spread to the brain/spinal cord.
Molecular/Genetic Testing
Additional molecular or genetic tests on the biopsy sample may be performed to identify specific subtypes of diffuse large B-cell lymphoma and genetic mutations that can impact prognosis and treatment.
The combined results from the biopsy, imaging, blood tests, and other studies allow doctors to make an accurate diagnosis of diffuse large B-cell lymphoma and determine the optimal treatment approach.
Treatment
The treatment of diffuse large B-cell lymphoma (DLBCL) involves a combination of therapies tailored to the patient’s specific condition, including the stage of the disease, overall health, and other individual factors.
Standard Frontline Treatment
R-CHOP Regimen
The most common and standard frontline treatment for diffuse large B-cell lymphoma is the R-CHOP regimen, which includes:
- Rituximab: A monoclonal antibody targeting B-cells.
- Cyclophosphamide: A chemotherapy drug.
- Doxorubicin: A chemotherapy drug.
- Vincristine (Oncovin): A chemotherapy drug.
- Prednisone: A steroid.
R-CHOP is typically administered in 21-day cycles, with the number of cycles depending on the stage and response to treatment.
Alternative Regimens
For patients with cardiovascular comorbidities or those who cannot tolerate R-CHOP, alternative regimens include:
- R-CEOP: Rituximab, cyclophosphamide, etoposide, vincristine, and prednisone.
- R-GCVP: Rituximab, gemcitabine, cyclophosphamide, vincristine, and prednisone.
Radiotherapy
Radiotherapy is often used as a consolidation treatment after chemotherapy, especially in patients with bulky disease or localized presentations. It can also be used for palliation in symptomatic patients.
Treatment for Relapsed/Refractory DLBCL
High-Dose Chemotherapy and Stem Cell Transplant
For patients with relapsed or refractory diffuse large B-cell lymphoma, high-dose chemotherapy followed by autologous stem cell transplantation (ASCT) is a common approach.
CAR T-Cell Therapy
Chimeric Antigen Receptor (CAR) T-cell therapy is a promising option for patients with relapsed or refractory diffuse large B-cell lymphoma. This involves modifying the patient’s T-cells to target and kill lymphoma cells.
Information about completed and ongoing clinical trials for DLBCL can be found in this huge database – clinicaltrials.gov
Supportive Treatments
Steroids
Steroids like prednisone are often used alongside chemotherapy to enhance its effectiveness and manage side effects.
Growth Factor Injections
Growth factor injections (G-CSF) are used to stimulate the production of white blood cells and reduce the risk of infection during chemotherapy.
Prognosis and Survivorship
The prognosis for diffuse large B-cell lymphoma (DLBCL) can be quite positive, especially with modern treatments. About 60-70% of people with DLBCL can be cured with standard chemotherapy combined with rituximab (R-CHOP). Achieving remission for at least two years is a strong indicator of long-term survival. However, the outlook can vary based on factors like age, overall health, and the stage of the disease at diagnosis. Younger patients and those diagnosed at an early stage generally have better outcomes. While some patients may experience relapse, new and innovative treatments are continually improving survival rates. It’s important to discuss your specific situation with your healthcare team to get a clearer understanding of your individual prognosis.
Watch George’s Cancer Survival Story from Lymphoma Research Foundation
Survivorship Challenges
Survivorship challenges for patients with diffuse large B-cell lymphoma (DLBCL) encompass a range of physical, emotional, and social issues that can persist long after treatment has ended. Here are some key challenges based on the provided sources:
Risk of Second Primary Malignancies (SPMs)
Survivors of diffuse large B-cell lymphoma are at an increased risk of developing second primary malignancies (SPMs). This risk is influenced by factors such as the type of treatment received (chemotherapy, radiation therapy, or a combination), age at diagnosis, and genetic predispositions. The risk of SPMs is particularly high in younger patients and those treated with combined chemoradiation therapy.
Long-Term Health Monitoring
Regular follow-up visits with healthcare providers are crucial for monitoring potential late effects of treatment, including the risk of SPMs, cardiovascular diseases, and other health issues. These visits often include blood tests, imaging scans, and assessments of overall health to detect any recurrence of lymphoma or new health problems early.
Quality of Life (QoL)
Survivors often experience a range of quality-of-life issues, including:
- Physical Fatigue: Persistent tiredness that can affect daily activities.
- Emotional Impact: Increased levels of anxiety, depression, and emotional distress.
- Cognitive Impairment: Issues with memory, attention, and other cognitive functions.
- Physical Symptoms: Pain, neuropathy, and dyspnea (difficulty breathing) are common, especially in those who underwent multiple cycles of chemotherapy.
Immune Health
DLBCL survivors may have long-term immune system impairments, making them more susceptible to infections. This includes a higher incidence of viral or fungal pneumonia, meningitis, and other infections. The use of rituximab, a common treatment for diffuse large B-cell lymphoma, has been linked to long-term immune deficiencies such as hypogammaglobulinemia (low levels of antibodies).
Cardiovascular Health
There is an increased risk of cardiovascular diseases among diffuse large B-cell lymphoma survivors, particularly those who received treatments like doxorubicin, which can be cardiotoxic. Conditions such as hypertension, diabetes, and baseline use of aspirin can further elevate this risk.
Psychological and Social Support
The emotional and psychological impact of surviving diffuse large B-cell lymphoma can be significant. Survivors may experience post-traumatic stress, anxiety, and depression. Supportive care, including counseling and support groups, is essential to help manage these issues and improve overall well-being.
Long-Term Follow-Up Care
Effective long-term follow-up care involves a multidisciplinary approach, including regular health check-ups, management of late effects, and lifestyle modifications to reduce the risk of recurrence and secondary health issues. Survivorship care plans tailored to individual needs can help manage these challenges effectively.
In summary, while many diffuse large B-cell lymphoma survivors achieve long-term remission, they face various challenges that require ongoing medical and psychosocial support to maintain their quality of life and overall health.
During Treatment
Common side effects include:
During treatment for diffuse large B-cell lymphoma (DLBCL), patients may experience a variety of side effects, particularly from the R-CHOP chemotherapy regimen. Here are some common side effects:
Common Side Effects of R-CHOP Chemotherapy
- Nausea and Vomiting: Chemotherapy can cause nausea and vomiting, which can often be managed with anti-nausea medications.
- Fatigue: Many patients experience significant tiredness and fatigue during and after treatment.
- Hair Loss: Temporary hair loss is a common side effect of chemotherapy.
- Decreased Appetite: Patients may have a reduced appetite, leading to weight loss.
- Constipation and Diarrhea: Both constipation and diarrhea can occur as side effects of chemotherapy.
- Mouth Sores: Chemotherapy can cause painful sores in the mouth.
- Low Blood Cell Counts: This includes low white blood cell count (neutropenia), increasing the risk of infections; low red blood cell count (anemia), causing fatigue and shortness of breath; and low platelet count (thrombocytopenia), leading to easy bruising or bleeding.
- Skin and Nail Changes: Patients may experience changes such as brittle nails and skin rashes.
- Increased Blood Glucose Levels: Prednisone, a component of R-CHOP, can raise blood sugar levels, which is particularly concerning for patients with diabetes.
Rare Side Effects
- Allergic Reactions: Rituximab can cause mild allergic reactions, especially with the first dose, including symptoms like feeling hot, flushed, or breathless; facial swelling; and back or abdominal pain.
- Cardiac Toxicity: Doxorubicin may cause heart rhythm abnormalities or heart failure.
- Peripheral Neuropathy: Nerve damage can cause numbness, tingling, or pain in the hands or feet.
- Lung Problems: These might include inflammation or scarring.
- Kidney or Liver Damage: Cyclophosphamide can irritate the bladder and potentially harm the kidneys or liver.
- Tumor Lysis Syndrome: This condition occurs when cancer cells are killed rapidly, releasing substances into the bloodstream that can harm the kidneys and cause muscle cramps, irregular heartbeat, and seizures.
Managing Side Effects
- Anti-Nausea Medications: Drugs like Zofran can help manage nausea and vomiting.
- Growth Factor Injections: These can help boost white blood cell counts to reduce infection risk.
- Supportive Care: Regular monitoring and supportive care from the healthcare team can help manage and mitigate side effects.
It’s important for patients to communicate with their healthcare providers about any side effects they experience, as there are often ways to manage and alleviate these symptoms.
Resources
- American Cancer Society – Cancer.org
- National Cancer Institute – Cancer.gov
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Cancer Research Institute – cancerresearch.org
- Լymphoma Research Foundation – lymphoma.org
- Blood Cancer UK – bloodcancer.org
- Treatment of Diffuse Large B-Cell Lymphoma – PubMed
- How I treat diffuse large B-cell lymphoma – PubMed
- Leukemia and Lymphoma Society – lls.org