Multiple Endocrine Neoplasia Type 2A (MEN2A) is a rare, inherited condition that causes tumors to form in certain hormone-producing glands. These tumors can affect the thyroid gland, adrenal glands, and parathyroid glands, often leading to hormone imbalances and other health problems.
This article will explain what MEN2A is, its causes, symptoms, and how it is diagnosed and treated. It will also cover the types of tumors involved, genetic testing, family screening, and long-term care, helping patients and families better understand and manage this condition.
What Is MEN2A?
Multiple Endocrine Neoplasia Type 2A (MEN2A) is a rare genetic condition that causes growth of tumors in certain glands of the body. These tumors usually form in the thyroid gland, adrenal glands, and parathyroid glands, which are all part of the system that controls hormones.
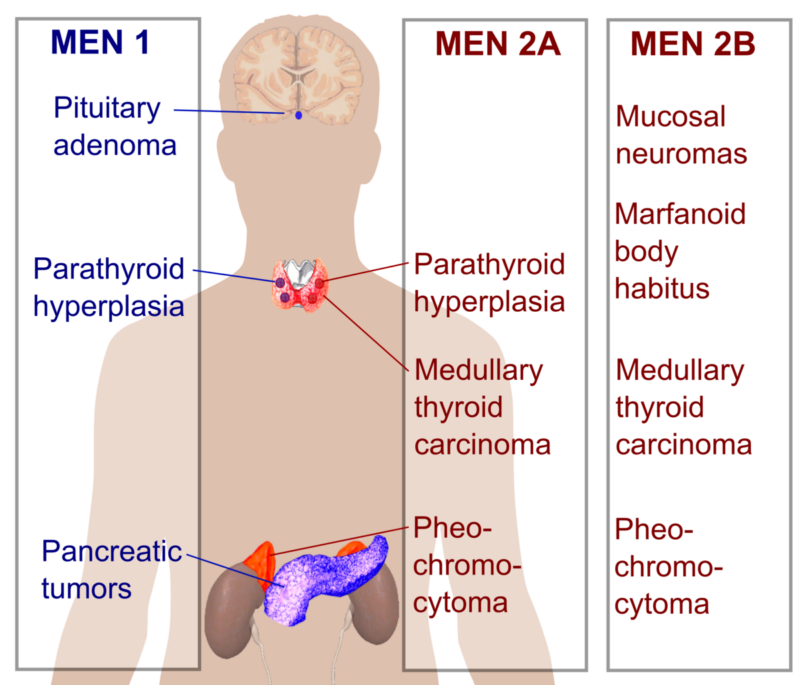
People with MEN2A are at risk of developing:
- Medullary thyroid cancer (a type of thyroid cancer)
- Pheochromocytoma (tumors in the adrenal glands that affect blood pressure)
- Parathyroid tumors (which can cause high calcium levels)
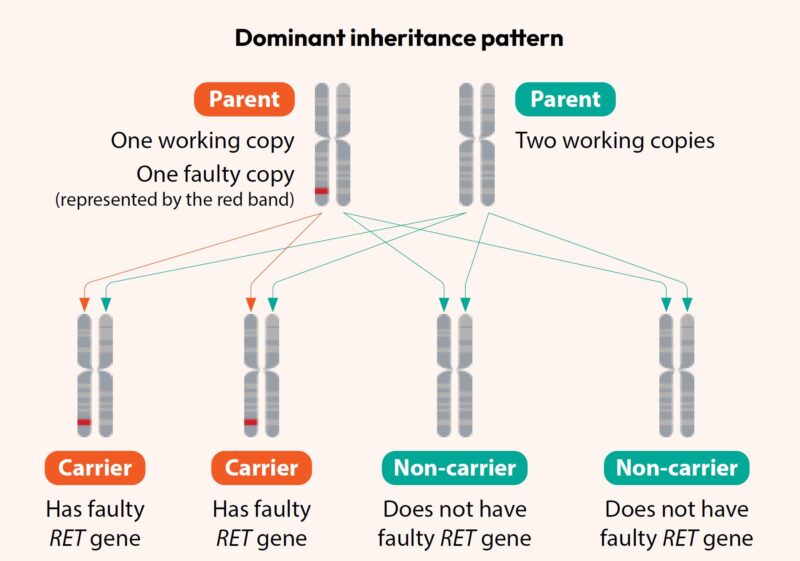
MEN2A is passed down in families, meaning if one parent has it, there’s a 50% chance their child might inherit it. Early diagnosis and regular check-ups help manage the condition and prevent serious health problems.
What Causes MEN2A?
Multiple Endocrine Neoplasia Type 2A (MEN2A) is caused by a change, or mutation, in a specific gene called the RET gene. This gene provides instructions for making a protein that helps control how cells grow and develop, especially in the hormone-producing glands. In MEN2A, the mutation in the RET gene leads to abnormal signals that cause cells in the thyroid, adrenal, and parathyroid glands to grow uncontrollably, forming tumors. Some of these tumors may produce excess hormones, leading to symptoms like high blood pressure or high calcium levels.
Because MEN2A is an inherited condition, the RET gene mutation is usually passed down from a parent. If a parent has the RET mutation, there is a 50% chance their child will inherit the same mutation and develop MEN2A. Genetic testing can detect this mutation early, allowing doctors to monitor for tumors and start treatment before serious problems develop. Early detection is key to managing MEN2A effectively.
Types of Tumors in MEN2A
People with Multiple Endocrine Neoplasia Type 2A (MEN2A) can develop tumors in three main glands in the body. These tumors affect how the body produces certain hormones and can cause different health problems. Here’s a simple explanation of the types of tumors:
- Medullary Thyroid Cancer: This is the most common tumor in MEN2A. It starts in the thyroid gland, which is located in the neck and helps control your metabolism. The cancer can grow slowly or quickly, but if found early, it can often be treated successfully by removing the thyroid.
- Pheochromocytoma (Adrenal Tumors): These tumors grow in the adrenal glands, which sit on top of the kidneys. They can cause the body to release too much adrenaline, leading to high blood pressure, headaches, sweating, and a fast heartbeat. Surgery to remove the tumors is usually needed.
- Parathyroid Tumors: These tumors affect the parathyroid glands, small glands in the neck that help control calcium levels in the blood. Tumors in these glands can cause high calcium levels, leading to kidney stones, weak bones, and fatigue. Surgery is often used to remove the overactive glands.
Knowing about these tumors helps doctors monitor and treat MEN2A early, improving health and preventing complications.
Symptoms and Warning Signs
In MEN2A, different tumors can cause different symptoms, depending on which glands are affected.The most common tumor is medullary thyroid cancer, which grows in the thyroid gland. Early on, this cancer may not cause obvious symptoms. But as it grows, some people might notice a lump or swelling in the neck, trouble swallowing, or a change in their voice. Pheochromocytoma tumors develop in the adrenal glands and can lead to the release of too much adrenaline. This can cause noticeable symptoms like high blood pressure, pounding headaches, heavy sweating, a racing heartbeat, and feelings of anxiety. These symptoms may come and go but can be severe when they appear.
When MEN2A affects the parathyroid glands, it can cause them to make too much parathyroid hormone, leading to high calcium levels in the blood. This may result in fatigue, muscle weakness, kidney stones, bone pain, or frequent urination.In addition to the more common symptoms linked to tumors in the thyroid, adrenal, and parathyroid glands, people with Multiple Endocrine Neoplasia Type 2A (MEN2A) may also experience several other symptoms that affect their overall health.
One such symptom is chronic diarrhea. This can occur due to hormonal imbalances caused by the tumors, particularly those in the thyroid gland. The excessive hormones can affect the digestive system, leading to frequent, loose bowel movements, which can impact daily life and nutrition. Another symptom seen in some MEN2A patients is a skin condition called cutaneous lichen amyloidosis. This presents as itchy, thickened, or dark patches of skin, often appearing on the upper back. While it doesn’t occur in everyone with MEN2A, it is a recognized sign in some cases and can cause discomfort.
Additionally, Hirschsprung disease is occasionally associated with MEN2A. This condition affects the nerves in parts of the gut, leading to problems with bowel movements. It can cause intestinal blockages and severe constipation, usually diagnosed early in life. Because these symptoms can sometimes be mild or easily confused with other conditions, regular check-ups and early testing are very important for anyone at risk of MEN2A. Early treatment can prevent serious problems and improve long-term health.

How Is MEN2A Diagnosed?
MEN2A is usually diagnosed through a combination of genetic testing, blood tests, and scans. Since MEN2A is inherited, doctors often recommend genetic testing first. This involves a simple blood test to check if a person has a mutation in the RET gene, which is the cause of MEN2A. If the mutation is found, it confirms the diagnosis. Doctors may also use blood tests to look for high levels of certain hormones. For example, if there is a tumor in the thyroid gland, hormone levels related to the thyroid may be higher than normal. Similarly, hormone levels from the adrenal or parathyroid glands may show signs of tumors.
In addition, imaging tests like ultrasounds, CT scans, or MRIs might be used to check for tumors in the neck, adrenal glands, or other areas. Because MEN2A runs in families, if one family member is diagnosed, doctors usually recommend testing other family members, even if they don’t have symptoms yet. Finding MEN2A early allows treatment to start before serious health problems develop.
Treatment Options for MEN2A
Because MEN2A is genetic, doctors often recommend genetic testing for family members to check for the RET gene mutation. Finding out early allows people to take steps to monitor their health and treat any tumors before they cause serious problems.
The main treatment for MEN2A focuses on removing tumors and preventing complications. Surgery is a key part of treatment. This often includes a thyroidectomy, where the thyroid gland is removed to prevent or treat medullary thyroid cancer. If tumors are found in the adrenal glands, an adrenalectomy may be performed to remove one or both adrenal glands. Additionally, if the parathyroid glands are overactive and causing high calcium levels, surgery may be done to remove the affected glands.
After surgery, doctors may also prescribe medications to help control hormone levels and manage symptoms, especially if certain glands have been removed. Since MEN2A is a lifelong condition, ongoing care is essential. Patients need regular monitoring, including blood tests, imaging scans, and follow-up check-ups. This helps doctors catch any new tumors early and keep hormone levels balanced. Early diagnosis and ongoing treatment help prevent serious complications and allow patients to stay healthy.
Myths and Misconceptions About MEN2A
Because Multiple Endocrine Neoplasia Type 2A (MEN2A) is a rare condition, there are several misunderstandings about it. Let’s clear up some of the most common myths:
- MEN2A is contagious: MEN2A is not contagious. It is a genetic condition, meaning it is inherited and passed down from parents to children through genes. You cannot catch MEN2A from someone else.
- Myth 2: Only older people get MEN2A: MEN2A can affect people at any age, even in childhood. Because it is genetic, many people are born with the gene mutation and may develop tumors at a young age. Early testing and monitoring are key.
- Myth 3: MEN2A always leads to cancer: While MEN2A increases the risk of certain cancers, especially medullary thyroid cancer, regular check-ups and early treatment (such as thyroid removal surgery) can prevent cancer from developing or spreading. Not everyone with MEN2A will have advanced cancer if monitored properly.
- Myth 4: Surgery cures MEN2A: Surgery, like removing the thyroid or adrenal glands, can effectively treat tumors, but MEN2A is a lifelong condition. Even after surgery, people need regular follow-ups to check for new tumors or hormone imbalances.
- Myth 5: If no one else in the family has it, you can’t have MEN2A: Although MEN2A is inherited, in rare cases, a new RET gene mutation can happen even if there is no family history. That’s why genetic testing is important if symptoms or tumors suggest MEN2A
You Can Watch More on OncoDaily Youtube TV
FAQ
What is Multiple Endocrine Neoplasia Type 2A (MEN2A)?
MEN2A is an inherited disorder characterized by the development of tumors in multiple endocrine glands, primarily affecting the thyroid (medullary thyroid carcinoma), adrenal glands (pheochromocytomas), and parathyroid glands.
What causes MEN2A?
MEN2A is caused by mutations in the RET gene, which provides instructions for producing a protein involved in cell signaling and growth. These mutations lead to uncontrolled cell growth in certain endocrine glands.
How is MEN2A inherited?
MEN2A is inherited in an autosomal dominant pattern, meaning a person needs only one copy of the mutated gene from one parent to develop the condition. Each child of an affected parent has a 50% chance of inheriting the mutation.
What are the common symptoms of MEN2A?
Symptoms vary depending on the affected glands but may include neck lumps (due to thyroid tumors), high blood pressure, headaches (from adrenal tumors), and elevated calcium levels leading to kidney stones or bone pain (from parathyroid involvement).
How is MEN2A diagnosed?
Diagnosis involves genetic testing for RET gene mutations, blood tests to assess hormone levels, and imaging studies like ultrasounds or CT scans to detect tumors in endocrine glands.
What treatment options are available for MEN2A?
Treatment typically includes surgical removal of affected glands, such as thyroidectomy for medullary thyroid carcinoma, adrenalectomy for pheochromocytomas, and parathyroidectomy for hyperparathyroidism. Lifelong monitoring is essential to manage and detect any new tumors.
Can MEN2A be detected before symptoms appear?
Yes, genetic testing can identify RET gene mutations before symptoms develop, allowing for early intervention and monitoring to prevent or minimize complications.
Is there a cure for MEN2A?
While there is no cure for the genetic mutation causing MEN2A, early detection and appropriate treatment of tumors can manage the condition effectively and improve quality of life.
What is the prognosis for individuals with MEN2A?
With early diagnosis and proper management, individuals with MEN2A can have a normal life expectancy. Regular follow-ups are crucial to monitor for new tumor development and manage hormone levels.
Should family members of someone with MEN2A be tested?
Yes, since MEN2A is hereditary, it is recommended that immediate family members undergo genetic testing to determine if they carry the RET gene mutation, enabling early monitoring and intervention.