Pediatric Rectal Cancer
Rectal cancer in children is a rare but serious condition that requires prompt diagnosis and comprehensive treatment. While colorectal cancer is more commonly seen in adults, it can also occur in the pediatric population, accounting for approximately 1% of all childhood cancers.
Prevalence and Epidemiology
Colorectal cancer in children is an uncommon occurrence, with an incidence rate of approximately 0.5 cases per 100,000 individuals under the age of 20 in the United States. However, recent studies have suggested a concerning trend of increasing incidence among young adults and adolescents. An analysis of the Surveillance, Epidemiology, and End Results (SEER) Program database from 1973 to 2006 identified 174 cases of colorectal cancer in patients younger than 19 years. Additionally, a study examining SEER data from 2010 to 2015 found 5,350 adolescents and young adults between the ages of 15 and 39 years with colorectal cancer.
Causes and Risk Factors
The exact causes of pediatric rectal cancer are not fully understood, but several risk factors have been identified:
Hereditary Syndromes
Familial adenomatous polyposis (FAP): FAP is an autosomal dominant disorder characterized by the development of numerous colorectal polyps, which have a high risk of progressing to colorectal cancer. FAP accounts for 5-10% of all colorectal cancers in children.
Lynch syndrome (hereditary non-polyposis colorectal cancer): This autosomal dominant disorder is caused by mutations in DNA mismatch repair genes, leading to an increased risk of colorectal and other cancers.
Other syndromes: Juvenile polyposis syndrome, Peutz-Jeghers syndrome, and Li-Fraumeni syndrome have also been associated with an increased risk of pediatric colorectal cancer.
Inflammatory Bowel Diseases
Ulcerative colitis and Crohn’s disease have been linked to an increased risk of colorectal cancer in both adult and pediatric populations.
Environmental Factors
Diet: A diet high in red and processed meats, as well as low in fruits and vegetables, has been associated with an increased risk of colorectal cancer in adults. The impact of diet on pediatric colorectal cancer is less well-studied.
Obesity: Childhood obesity has been linked to an increased risk of various cancers, including colorectal cancer.
Genetic Factors
Certain genetic mutations, such as those in the APC, KRAS, and TP53 genes, have been implicated in the development of colorectal cancer in both adults and children.
It is important to note that the majority of pediatric colorectal cancer cases occur sporadically, without any identifiable risk factors or underlying genetic conditions.
Symptoms
The most common symptoms of pediatric rectal cancer include:
- Bleeding from the rectum
- Blood in the stool
- Constipation
- Diarrhea
- Fatigue (extreme tiredness)
- Pain in the abdomen
- Nausea and vomiting
- Weight loss for no known reason
- Loss of appetite
- Anemia (low red blood cell count)
- Feeling dizzy or having a fast/irregular heartbeat
- Shortness of breath
- Pale skin (often due to anemia)
The specific symptoms can depend on the location of the tumor. For example, tumors in the rectum or lower colon may cause abdominal pain, constipation, and diarrhea, while tumors in the left side of the colon may cause a palpable abdominal mass, weight loss, nausea, and vomiting. It’s important to note that these symptoms can also be caused by other conditions, so a thorough medical evaluation is necessary to diagnose pediatric rectal cancer. Early recognition of symptoms and prompt diagnosis are crucial for improving outcomes in these patients.
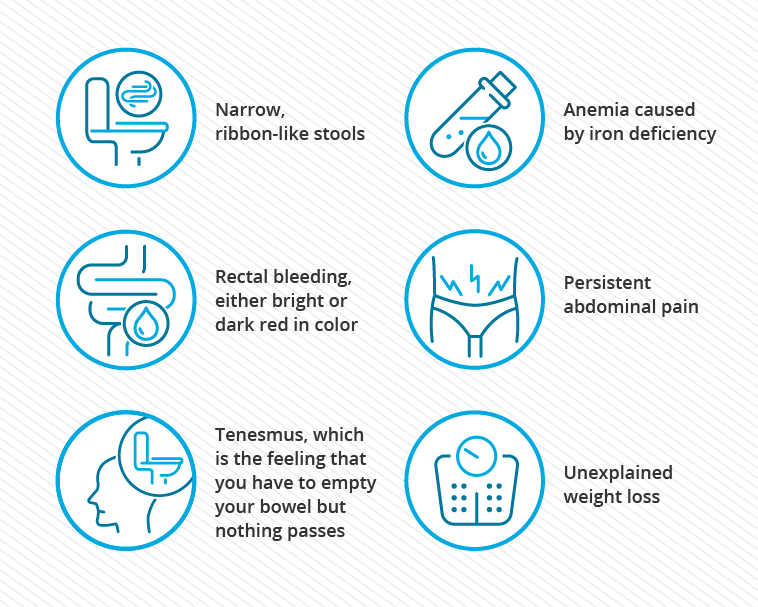
Rectal Cancer Symptoms and Signs. This image is taken from cancercenter.com.
Diagnosis and Types
The diagnosis of pediatric rectal cancer can be challenging due to the rarity of the condition and the non-specific nature of the presenting symptoms. Common symptoms include abdominal pain, rectal bleeding, weight loss, and anemia, which can often be mistaken for more common gastrointestinal conditions. This frequently leads to a delay in diagnosis, with the majority of patients being diagnosed at an advanced stage of the disease. The diagnostic workup typically includes:
Physical Examination
Digital rectal examination can help identify the presence of a palpable mass or other abnormalities.
Imaging Studies
Colonoscopy and biopsy: This is the gold standard for diagnosing colorectal cancer, as it allows for direct visualization of the tumor and collection of a tissue sample for histological analysis.
CT or MRI: These imaging modalities can help assess the extent of the disease, including the presence of metastases.
PET scan: PET scans can be used to detect the presence of distant metastases and guide treatment planning.
Laboratory Tests
Tumor markers: Elevated levels of carcinoembryonic antigen (CEA) and other tumor markers may be helpful in the diagnosis and monitoring of colorectal cancer, although their utility in the pediatric population is less well-established.
Genetic testing: Genetic analysis, such as testing for mutations in the APC, KRAS, and TP53 genes, may be performed to identify underlying hereditary syndromes.
Types of Pediatric Rectal Cancer
Adenocarcinoma
Adenocarcinoma is the most common histological subtype of pediatric rectal cancer, accounting for the majority of cases.
Pediatric adenocarcinomas are often more aggressive and have a higher incidence of unfavorable histological subtypes, such as mucinous adenocarcinoma and signet-ring cell carcinoma, compared to adult colorectal cancers.
Mucinous Adenocarcinoma
Mucinous adenocarcinoma is a rare subtype of colorectal cancer that is more commonly seen in the pediatric population, with some studies reporting it in up to 50% of cases.
Mucinous adenocarcinomas are characterized by the production of large amounts of extracellular mucin and are associated with a poorer prognosis compared to other histological subtypes.
Signet-Ring Cell Carcinoma
Signet-ring cell carcinoma is another rare and aggressive subtype of colorectal cancer that is more frequently observed in the pediatric population.
Signet-ring cell carcinomas are defined by the presence of more than 50% of tumor cells with intracytoplasmic mucin, which pushes the nucleus to the periphery of the cell.
These tumors are also associated with a worse prognosis compared to other histological subtypes.
It is important to note that the aggressive nature of the disease, the presence of unfavorable histological subtypes, and the delayed diagnosis contribute to the poorer prognosis observed in pediatric rectal cancer patients compared to their adult counterparts.
This video guide can assist in reassuring your child and alleviating their concerns about the upcoming endoscopy procedure.
Treatment
The treatment of pediatric rectal cancer typically involves a multidisciplinary approach, including surgery, chemotherapy, and radiation therapy. The specific treatment plan is tailored to the individual patient’s disease stage, tumor characteristics, and overall health status.
Surgery
Complete surgical resection of the primary tumor is the most important prognostic factor and the primary goal of treatment.
Depending on the location and extent of the tumor, surgical options may include partial colectomy, subtotal colectomy, or abdominoperineal resection.
In cases of advanced or metastatic disease, the role of surgery is often limited to palliative measures, such as relieving bowel obstruction or controlling bleeding.
Chemotherapy
Adjuvant chemotherapy, often using a combination of fluorouracil (5-FU) and leucovorin, is commonly used in the treatment of pediatric colorectal cancer, especially for patients with advanced-stage disease.
Other chemotherapeutic agents, such as irinotecan, may also be incorporated into the treatment regimen.
Neoadjuvant chemotherapy, administered before surgery, may be used to shrink the tumor and improve the chances of complete surgical resection.
Radiation Therapy
Radiation therapy is often used in the treatment of rectal cancers, particularly for tumors located in the lower part of the colon or rectum.
Radiation therapy may be used in combination with chemotherapy, either before or after surgery, to improve local control and overall survival.
Targeted Therapies
Emerging evidence suggests that targeted therapies, such as those targeting the EGFR or VEGF pathways, may have a role in the treatment of pediatric colorectal cancer, especially in cases with specific genetic alterations.
However, the use of targeted therapies in the pediatric population is still limited, and more research is needed to establish their efficacy and safety.
Immunotherapy
Immunotherapeutic approaches, including checkpoint inhibitors, have shown promise in the treatment of adult colorectal cancer, particularly in cases with microsatellite instability or mismatch repair deficiencies.
The role of immunotherapy in pediatric colorectal cancer is an area of active research, with ongoing clinical trials exploring the potential benefits of these treatments.
The treatment of pediatric rectal cancer is often challenging due to the aggressive nature of the disease, the presence of unfavorable histological subtypes, and the limited evidence-based guidelines specific to the pediatric population. Ongoing clinical trials and collaborative efforts among pediatric oncologists are crucial to improving the understanding and management of this rare condition.
In this video, Ahmed Allawi, MD elucidates the progression of rectal cancer and the intricate array of treatments involved in addressing this condition.
Prognosis and Survival
The prognosis for pediatric rectal cancer is generally poorer compared to adults, primarily due to delayed diagnosis and the presence of advanced-stage disease at presentation. Studies have shown that only about 19% of pediatric colorectal cancer cases are diagnosed with localized disease, while the majority (55.3%) present with regional lymph node involvement or distant metastases. This is in contrast to adult colorectal cancer, where a higher proportion of patients are diagnosed at an earlier stage.
The 5-year survival rates for pediatric colorectal cancer range from 20% to 50%, depending on the stage of the disease at diagnosis. This is significantly lower than the 5-year survival rates for adult colorectal cancer, which can exceed 90% for early-stage disease. Several factors contribute to the poor prognosis of pediatric rectal cancer:
Aggressive Disease Behavior
Pediatric colorectal cancers are often characterized by more aggressive biological behavior, with a higher incidence of unfavorable histological subtypes, such as mucinous adenocarcinoma and signet-ring cell carcinoma.
These subtypes are associated with a poorer prognosis and increased resistance to standard treatment modalities.
Delayed Diagnosis
The non-specific nature of the presenting symptoms often leads to a delayed diagnosis, with the majority of patients being diagnosed at an advanced stage of the disease.
This delay can negatively impact the chances of successful treatment and long-term survival.
Younger Age
Studies have shown that younger age (≤21 years) is a significant predictor of mortality for both colon and rectal cancers, even after adjusting for other factors.
This suggests that the underlying tumor biology and response to treatment may be different in the pediatric population compared to adults.
It is important to note that while the overall prognosis for pediatric rectal cancer is poorer, there have been some success stories reported in the literature. These cases highlight the importance of early recognition of symptoms, prompt diagnosis, and access to specialized multidisciplinary care to improve outcomes for these patients.
Patient’s Survivorship
Challenges Before Treatment
Delayed Diagnosis
The non-specific nature of the presenting symptoms, such as abdominal pain, rectal bleeding, and weight loss, often leads to a delayed diagnosis of pediatric rectal cancer.
This delay in diagnosis results in the majority of patients being diagnosed at an advanced stage of the disease, which negatively impacts their chances of successful treatment and long-term survival.
To address this challenge, healthcare providers must maintain a high index of suspicion for rectal cancer, especially in children with known risk factors or a family history of the disease. Early recognition of symptoms and prompt referral to a pediatric oncologist are crucial.
Aggressive Disease Behavior
Pediatric rectal cancers are often characterized by more aggressive biological behavior, with a higher incidence of unfavorable histological subtypes, such as mucinous adenocarcinoma and signet-ring cell carcinoma.
These aggressive subtypes are associated with a poorer prognosis and increased resistance to standard treatment modalities.
Ongoing research is needed to better understand the unique molecular and genetic characteristics of pediatric rectal cancer, which may inform the development of more targeted and effective treatment strategies.
Challenges After Treatment
Adverse Effects of Treatment
The intensive treatment regimens, including surgery, chemotherapy, and radiation therapy, can have significant short-term and long-term adverse effects on the growing and developing bodies of pediatric patients.
These may include growth and developmental delays, infertility, secondary malignancies, and organ dysfunction.
Comprehensive supportive care, including close monitoring and management of treatment-related side effects, is essential to mitigate these challenges and improve the quality of life for pediatric rectal cancer survivors.
Psychosocial Challenges
Pediatric patients with rectal cancer and their families face significant psychosocial challenges, including the emotional and social impact of the diagnosis, the disruption of normal childhood activities, and the long-term effects of the disease and its treatment on the child’s physical and mental well-being.
Providing access to specialized psychosocial support services, such as counseling, support groups, and educational resources, can help address these challenges and improve the overall well-being of the patient and their family.
Lack of Specialized Care
The rarity of pediatric rectal cancer can make it challenging for healthcare providers to gain extensive experience in the management of this condition.
This can lead to a lack of specialized care and the need for referral to tertiary care centers with expertise in pediatric oncology.
Establishing collaborative networks among pediatric oncology centers and developing specialized guidelines for the management of pediatric rectal cancer can help address this challenge and ensure that patients have access to the best possible care.
To manage these challenges, a multidisciplinary approach involving pediatric oncologists, surgeons, radiation oncologists, gastroenterologists, and supportive care specialists is crucial. Additionally, the continued development of targeted therapies, immunotherapies, and personalized treatment strategies, as well as the expansion of clinical trial opportunities for pediatric rectal cancer patients, may help improve outcomes and quality of life for these patients.
Resources
- American Society of Clinical Oncology (ASCO) – Cancer.net
- Colorectal Cancer Alliance – colorectalcancer.org
- National Cancer Institute – cancer.gov
- American Cancer Society – cancer.org
- National Library of Medicine – clinicaltrials.gov
- Journal of Clinical Oncology (ASCO) Publications – ascopubs.org
- Memorial Sloan Kettering Cancer Center – mskcc.org
- An Unusual Presentation of Rectal Carcinoma in a Child – PubMed
- Colorectal cancer in children: case report and review of literature – PubMed
- Annals of Palliative Medicine – apm.amegroups.org
- Risk Factors for the Diagnosis of Colorectal Cancer – PubMed
- Palliative Care in Paediatric Oncology: an Update – PubMed
- Standford Medicine – med.stanford.edu
- Pathological Features and Prognostication in Colorectal Cancer – PubMed
- Oncodaily.com – Online platform where you can find anything related to cancer such as everyday news, blogs, videos, podcasts, etc.