Metastatic Lung Cancer: Causes, Symptoms, Treatment, and 2025 Advances in Therapy
Metastatic lung cancer, also known as stage IV lung cancer, represents the most advanced form of the disease, in which cancer cells have spread beyond the lungs to distant organs such as the brain, bones, liver, or adrenal glands. This stage signifies a transition from localized cancer to systemic disease, often associated with complex symptoms and requiring comprehensive treatment strategies. The majority of cases of lung cancer diagnosed at this stage are either non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC), both of which demonstrate distinct biological behaviors and responses to treatment.
Due to its aggressive nature and frequent late diagnosis, metastatic lung cancer remains one of the leading causes of cancer-related mortality worldwide. However, recent advances in targeted therapy, immunotherapy, and molecular diagnostics are reshaping the management and prognosis of this challenging condition.
What is the Difference Between Metastatic Lung Cancer and Primary Lung Cancer?
Primary lung cancer originates in the lung tissue itself, typically from the bronchi, bronchioles, or alveoli. This includes types such as non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). These cancers begin in the lung and can later spread (metastasize) to other parts of the body. (Travis, W. D., et al. (2015). WHO Classification of Tumours of the Lung).
You Can Read More About NSCLC on Oncodaily
Metastatic lung cancer, on the other hand, refers to cancer that has spread to the lungs from a primary tumor elsewhere in the body, such as the breast, colon, kidney, or prostate. In this case, the cancer cells found in the lungs are not lung cancer cells but are the same type as the original cancer. The key difference lies in the origin of the cancer cells and how the disease is treated. Primary lung cancer is treated based on lung cancer guidelines, while metastatic cancer to the lung is treated according to the site of the original tumor.
What Does Lung Cancer Usually Metastasize to First?
Lung cancer, particularly in advanced stages, has a well-documented pattern of distant spread through both the blood (hematogenous) and lymphatic systems. Among the most commonly affected organs, the liver frequently emerges as the first site of metastasis, especially in cases of non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). Studies indicate that approximately 34% of patients with metastatic lung cancer present with liver involvement at the time of diagnosis (Riihimäki et al., 2014).
The adrenal glands follow closely, involved in roughly 32% of metastatic cases, often without clinical symptoms due to their silent nature (Quint & Tummala, 2008). Bones are another early site, affecting around 15% of patients, often leading to pain, pathological fractures, or hypercalcemia (Riihimäki et al., 2014). Brain metastases, while also common, may develop either early or later in the disease, depending on the subtype and biological aggressiveness, with SCLC showing a particular predilection for central nervous system involvement (Mountain, 1997).
These metastasis patterns are not only crucial for understanding disease progression but also for staging and treatment planning. Identification of the first site of metastasis often relies on imaging modalities such as PET-CT, MRI, and bone scans to inform prognosis and guide systemic therapies.
Causes of Metastatic Lung Cancer
Metastatic lung cancer develops when primary lung cancer cells acquire the ability to invade distant tissues and organs. The underlying causes are generally the same as those for the initial development of lung cancer, but certain biological and environmental factors increase the likelihood of the disease progressing to a metastatic stage.
The predominant cause remains tobacco smoking, which not only initiates carcinogenesis in lung tissue but also contributes to the accumulation of genetic mutations that enhance tumor invasiveness and metastatic potential (Hecht, 2003). Smoking-induced cancers are more likely to exhibit mutations in genes such as TP53, KRAS, and LKB1, which are associated with aggressive tumor behavior and early dissemination (Sun et al., 2007).
Another key factor is tumor biology. Some tumors inherently possess characteristics that make them more likely to metastasize, such as high proliferative rates, angiogenesis, loss of cell adhesion (e.g., via E-cadherin), and the presence of circulating tumor cells (CTCs) that travel through blood or lymphatics (Valastyan & Weinberg, 2011).
Genetic alterations also play a role. Specific mutations or gene rearrangements—such as EGFR mutations or ALK fusions—are found in certain subsets of lung cancer, and while they can be targeted therapeutically, they also influence metastatic patterns. For example, EGFR-mutant tumors often metastasize to the brain or bones (Camidge et al., 2014). Additionally, delayed diagnosis is a contributing factor. Lung cancer often progresses silently until it reaches an advanced stage, which increases the chance that it will have already metastasized at the time of detection.
Immunosuppression either due to underlying conditions or iatrogenic causes can impair the body’s ability to control tumor spread, facilitating metastasis. Finally, environmental exposures such as radon, air pollution, or occupational carcinogens may contribute to the overall tumor aggressiveness, especially when combined with genetic susceptibility.
What is the Survival Rate for Metastatic Lung Cancer?
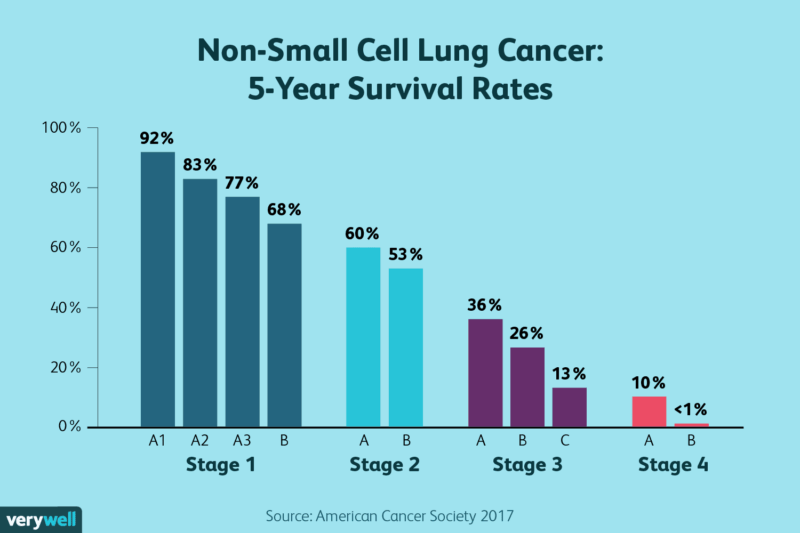
The survival rate for metastatic lung cancer—also known as stage IV lung cancer—remains low, though recent advances in targeted therapies and immunotherapy have begun to improve outcomes for select groups of patients.
Historically, the 5-year survival rate for metastatic non-small cell lung cancer (NSCLC) was around 5% or less, while for small cell lung cancer (SCLC), it was less than 2% due to its more aggressive behavior and early dissemination (Siegel et al., 2023).However, patients with driver mutations, such as EGFR, ALK, or ROS1, may benefit from targeted therapies that can extend survival. For instance, patients with EGFR-mutant NSCLC treated with third-generation EGFR tyrosine kinase inhibitors like osimertinib have shown median overall survival exceeding 38 months in clinical trials (Soria et al., 2018).
Similarly, the introduction of immunotherapy has offered improved outcomes for patients without targetable mutations but with high PD-L1 expression. Trials such as KEYNOTE-024 showed that pembrolizumab monotherapy in this subgroup resulted in a median overall survival of over 26 months, significantly better than with chemotherapy alone (Reck et al., 2019). Despite these advances, prognosis remains guarded, especially for patients without actionable mutations or low immunogenic tumors. Most patients eventually develop resistance or disease progression, highlighting the need for continued clinical research and early diagnosis.
Symptoms of Metastatic Lung Cancer
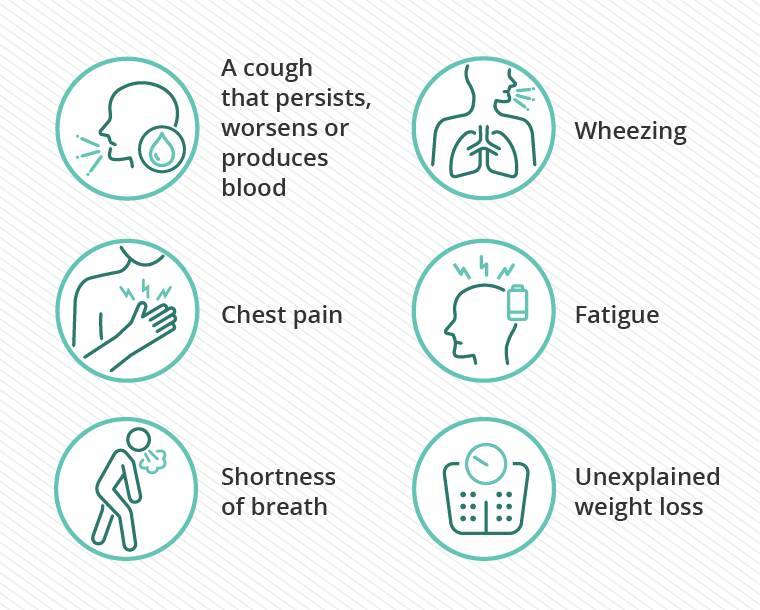
When lung cancer spreads to other organs, it often causes a wide range of symptoms depending on the site of metastasis. Common respiratory symptoms like chronic coughing and shortness of breath may persist or worsen due to tumor burden in the lungs. Chest pain, especially during breathing or coughing, is frequently reported in cases with pleural involvement.
If the cancer spreads to the bones, patients may experience localized pain, especially in areas like the spine, hips, or ribs. Brain metastases can present with neurological symptoms such as persistent headaches, dizziness, vision disturbances, weakness in limbs, or seizures. Liver involvement may result in symptoms such as upper abdominal discomfort, jaundice, or swelling. General signs like fatigue, loss of appetite, and significant weight loss are also typical, reflecting the body’s systemic response to widespread cancer.
Diagnosis of Metastatic Lung Cancer
Diagnosing metastatic lung cancer involves a combination of imaging, histological confirmation, and molecular testing to determine the extent and biology of the disease. The process often begins with a chest X-ray or a more detailed CT scan of the chest and abdomen to identify the primary lung tumor and potential metastatic sites. PET-CT scans are commonly used to evaluate the metabolic activity of lesions and detect distant spread, especially in bones, liver, or adrenal glands.
For patients with neurological symptoms, MRI of the brain is essential to rule out or confirm brain metastases. When metastases are suspected, tissue confirmation is critical. This can be achieved through image-guided biopsy (e.g., from lung, liver, or lymph nodes), bronchoscopy with biopsy for centrally located tumors, or mediastinoscopy for lymph node evaluation.
Histopathological examination identifies the tumor type (e.g., adenocarcinoma, squamous cell carcinoma) and helps differentiate primary lung cancer from metastatic tumors originating from other organs. Molecular profiling of the tumor tissue is essential in non-small cell lung cancer to detect mutations such as EGFR, ALK, ROS1, and PD-L1, guiding targeted therapy and immunotherapy decisions.
Does Metastasis Occur Quickly in Lung Cancer?
Metastasis in lung cancer, particularly in small cell lung cancer (SCLC), can occur very quickly. SCLC is well-recognized for its aggressive clinical course, rapid cellular proliferation, and early dissemination to distant organs, including the brain, liver, adrenal glands, and bones (Travis et al., 2015). This rapid progression is a hallmark of the disease and often results in patients presenting with extensive-stage cancer at diagnosis (Kalemkerian et al., 2013).
Non-small cell lung cancer (NSCLC), while generally slower-growing compared to SCLC, is also capable of early metastasis, especially in the presence of aggressive molecular features such as EGFR mutations or ALK rearrangements. These subtypes may metastasize to the brain or bones earlier than previously recognized, particularly in patients with delayed diagnosis or no initial symptoms (Rudin et al., 2019). The speed at which metastasis occurs depends on a combination of tumor histology, molecular profile, and host factors. SCLC’s ability to double in size within 25 to 30 days highlights its propensity for fast systemic spread if not identified and treated promptly (Kalemkerian et al., 2013).
Treatment Strategies for Metastatic Lung Cancer
Treatment for metastatic lung cancer depends on the histological type (non-small cell vs. small cell), molecular characteristics, extent of metastasis, and overall health of the patient. In most cases, the goal is to prolong survival, relieve symptoms, and maintain quality of life, as a cure is typically not possible in advanced disease stages.
In metastatic non-small cell lung cancer (NSCLC), targeted therapy has dramatically improved outcomes for patients with specific genetic mutations. Patients with EGFR mutations may benefit from tyrosine kinase inhibitors like osimertinib, while those with ALK or ROS1 rearrangements may receive ALK inhibitors such as alectinib or lorlatinib (Reck et al., 2021). Immune checkpoint inhibitors, such as pembrolizumab or nivolumab, have also become standard for tumors expressing PD-L1, either alone or in combination with chemotherapy (Garon et al., 2015).
For patients without actionable mutations, platinum-based chemotherapy remains a core component, often given in combination with immunotherapy. For example, the KEYNOTE-189 trial demonstrated improved overall survival when pembrolizumab was added to chemotherapy in patients with nonsquamous NSCLC (Gandhi et al., 2018).
Read More About Immunotherapy for Lung Cancer in OncoDaily
In small cell lung cancer (SCLC), especially in the extensive stage, treatment traditionally includes a combination of cisplatin or carboplatin and etoposide. The addition of immunotherapy, such as atezolizumab or durvalumab, has improved outcomes and is now included in first-line treatment (Horn et al., 2018; Paz-Ares et al., 2019).
Radiotherapy is also used in a palliative role to manage pain from bone metastases. For brain metastases, treatment depends on the number, size, and location of lesions. Options include whole-brain radiation therapy, stereotactic radiosurgery, and, in some cases, surgical resection. Advances like hippocampal-sparing techniques and neuroprotective agents are helping reduce cognitive side effects (Gondi et al., 2014).
Role of Surgery in Metastatic Lung Cancer Management
Surgery in metastatic lung cancer is typically reserved for highly selected patients and specific clinical circumstances. In general, metastatic disease is treated with systemic therapies because of its widespread nature. However, in cases of oligometastatic disease, where the cancer has spread to a limited number of sites, surgical intervention may offer a survival benefit or even a chance for long-term disease control. This approach is supported by the concept introduced by Hellman and Weichselbaum (1995), who proposed that oligometastases might represent an intermediate stage of cancer spread where aggressive local therapy could be beneficial.
For example, patients with non-small cell lung cancer (NSCLC) who present with a solitary brain metastasis and have otherwise controlled disease may benefit from both resection of the brain lesion and surgery for the primary lung tumor. This combined approach has been associated with improved outcomes in several retrospective studies (Xu et al., 2021). Similarly, surgical removal of isolated adrenal metastases has shown potential for prolonged survival, especially in patients with good performance status and controlled primary tumors (Tanvetyanon et al., 2008).
Resection is considered more frequently in patients with actionable molecular alterations such as EGFR mutations or ALK rearrangements, where systemic targeted therapy controls disseminated disease and leaves room for local treatment of residual sites. In contrast, surgery has no routine role in metastatic small cell lung cancer (SCLC) due to its aggressive biology and early widespread dissemination (Hellman & Weichselbaum, 1995).
Ultimately, surgical decisions are individualized and made by multidisciplinary teams, taking into account factors like tumor burden, site of metastases, patient health status, and response to prior treatments. Metastasectomy should always be viewed as part of a multimodal approach and not a standalone treatment (Takanami, 2003).
Is Metastatic Lung Cancer Curable?
Metastatic lung cancer is generally considered incurable with current treatment approaches, primarily due to its widespread nature at diagnosis. However, advances in therapy, especially targeted therapy and immunotherapy, have significantly improved survival and quality of life for many patients.
In rare cases of oligometastatic lung cancer, where the disease is limited to a few metastatic sites, aggressive local treatments like surgery or stereotactic body radiotherapy (SBRT) combined with systemic therapy may lead to long-term disease control and even durable remission in select patients (Hellman & Weichselbaum, 1995; Gomez et al., 2016).
You Can Read More about IMRT on OncoDaily
Despite these advances, for the majority of patients with widespread metastatic non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC), the disease remains incurable. The focus is typically on prolonging survival, alleviating symptoms, and preserving quality of life using personalized treatment strategies that may include chemotherapy, targeted therapy, immunotherapy, and palliative care (Planchard et al., 2018; Reck et al., 2016).
Palliative Care in Metastatic Lung Cancer
Palliative care plays a crucial role in the management of metastatic lung cancer. Since metastatic disease is generally considered incurable, the primary goals shift toward improving quality of life, managing symptoms, and providing psychological and emotional support. Palliative interventions may include pain relief, treatment of dyspnea, management of fatigue, nutritional support, and addressing anxiety or depression. It also involves helping patients and families with advanced care planning and decision-making throughout the disease course (Temel et al., 2010). Studies have shown that early integration of palliative care alongside standard oncologic treatments not only enhances patient comfort but may also improve survival outcomes (Bakitas et al., 2015).
New 2025 Advances in Treatment of Metastatic Lung Cancer
In 2025, the treatment landscape for metastatic lung cancer continues to evolve rapidly, with innovative strategies significantly improving survival and quality of life. One of the most notable advances includes the development and approval of new targeted therapies such as repotrectinib, which has demonstrated efficacy in patients with ROS1-positive non-small cell lung cancer (NSCLC), particularly those who have developed resistance to previous tyrosine kinase inhibitors (Lin et al., 2025). Additionally, zenocutuzumab, a bispecific antibody targeting HER2/HER3 receptors, has shown promising results in treating patients with NSCLC harboring neuregulin 1 (NRG1) gene fusions, a previously difficult-to-treat molecular subtype (Nguyen et al., 2025).
Read More About Zenocutuzumab on Oncodaily
Immunotherapy also remains at the forefront, with trials evaluating novel checkpoint inhibitors and their combinations with existing therapies. The EMPOWER-Lung 1 trial reported updated five-year outcomes, showing that cemiplimab continues to provide long-term survival benefits in patients with advanced NSCLC and high PD-L1 expression, highlighting the durability of immunotherapeutic responses (Ramalingam et al., 2025).
Read More About Cemiplimab on Oncodaily
In addition to systemic therapies, advancements in liquid biopsy and circulating tumor DNA (ctDNA) analysis are now enhancing real-time monitoring of treatment response and early detection of resistance mutations, allowing for timely therapeutic adjustments (Patel & Yu, 2025). These technologies have enabled more personalized and dynamic treatment approaches, shifting the paradigm toward precision oncology.
Radioligand therapies are also under active investigation, including trials using lutetium-labeled peptides that target specific tumor receptors, showing encouraging tumor control rates with tolerable safety profiles (Cheng et al., 2025). The integration of artificial intelligence into radiology and pathology is further optimizing diagnosis, prognostication, and treatment selection, contributing to more efficient clinical decision-making.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
FAQ
What is metastatic lung cancer?
Metastatic lung cancer occurs when cancer that originated in the lungs spreads to other parts of the body, such as the brain, bones, liver, or adrenal glands.
What causes lung cancer to metastasize?
Metastasis happens when cancer cells break away from the primary tumor and travel through the bloodstream or lymphatic system to form new tumors in other organs. Factors like tumor aggressiveness and genetic mutations can influence this process.
What are common symptoms of metastatic lung cancer?
Symptoms vary depending on where the cancer has spread. Common signs include persistent cough, chest pain, shortness of breath, bone pain, neurological symptoms like headaches or seizures, and unexplained weight loss.
Where does lung cancer typically spread first?
Lung cancer commonly spreads to the brain, bones, liver, adrenal glands, and lymph nodes.
How is metastatic lung cancer diagnosed?
Diagnosis involves imaging tests like CT scans, MRIs, PET scans, and bone scans, along with biopsies to confirm the presence and extent of cancer spread.
What treatment options are available for metastatic lung cancer?
Treatment may include chemotherapy, targeted therapy, immunotherapy, radiation therapy, and palliative care to manage symptoms and improve quality of life.
What are the latest advancements in treating metastatic lung cancer as of 2025?
Recent advancements include the development of new targeted therapies and immunotherapies, such as the combination of amivantamab and lazertinib, which has shown promise in prolonging progression-free survival in patients with advanced non-small cell lung cancer.
Can surgery be used to treat metastatic lung cancer?
Surgery is generally not the primary treatment for metastatic lung cancer but may be considered in select cases where metastasis is limited and the patient is otherwise healthy.
What is the prognosis for someone with metastatic lung cancer?
Prognosis varies based on factors like cancer type, extent of spread, and overall health. Generally, metastatic lung cancer has a lower survival rate, but treatments can help manage symptoms and extend life.
What supportive care options are available for patients with metastatic lung cancer?
Palliative care focuses on relieving symptoms and improving quality of life, addressing issues like pain, breathing difficulties, and emotional support.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
