
Cancer During Pregnancy: Overcoming Diagnostic Challenges, Treatment Strategies, and Patient Support
Cancer diagnosed during pregnancy is a rare but increasingly recognized condition, occurring in approximately 1 in 1,000 to 2,000 pregnancies worldwide. As more women delay childbirth to later reproductive years, the incidence of pregnancy-associated cancers is rising. The most common cancers diagnosed during pregnancy include breast cancer, melanoma, cervical cancer, and hematologic malignancies. Diagnosing cancer in pregnant women is particularly challenging because many cancer symptoms overlap with normal pregnancy changes, often leading to delayed detection.

Balancing maternal health and fetal safety is critical. Treatment decisions must carefully weigh the benefits of timely cancer therapy against potential risks to the developing fetus, requiring a multidisciplinary approach to optimize outcomes for both mother and baby. Adriana Hepner, World J Oncol. 2019.
What Are the Challenges of Diagnosing Cancer During Pregnancy?
Diagnosing cancer during pregnancy is particularly challenging because many cancer symptoms overlap with normal pregnancy changes, often leading to delays. Common signs such as nausea, vomiting, breast tenderness, abdominal pain, or fatigue are frequently attributed to pregnancy itself rather than underlying malignancy. For example, breast lumps may be missed due to breast engorgement, and abdominal discomfort can mask gastrointestinal cancers. This symptom overlap contributes to later-stage cancer diagnoses and poorer prognoses in some cases. Min Hee Shim,Obstet Gynecol Sci. 2016
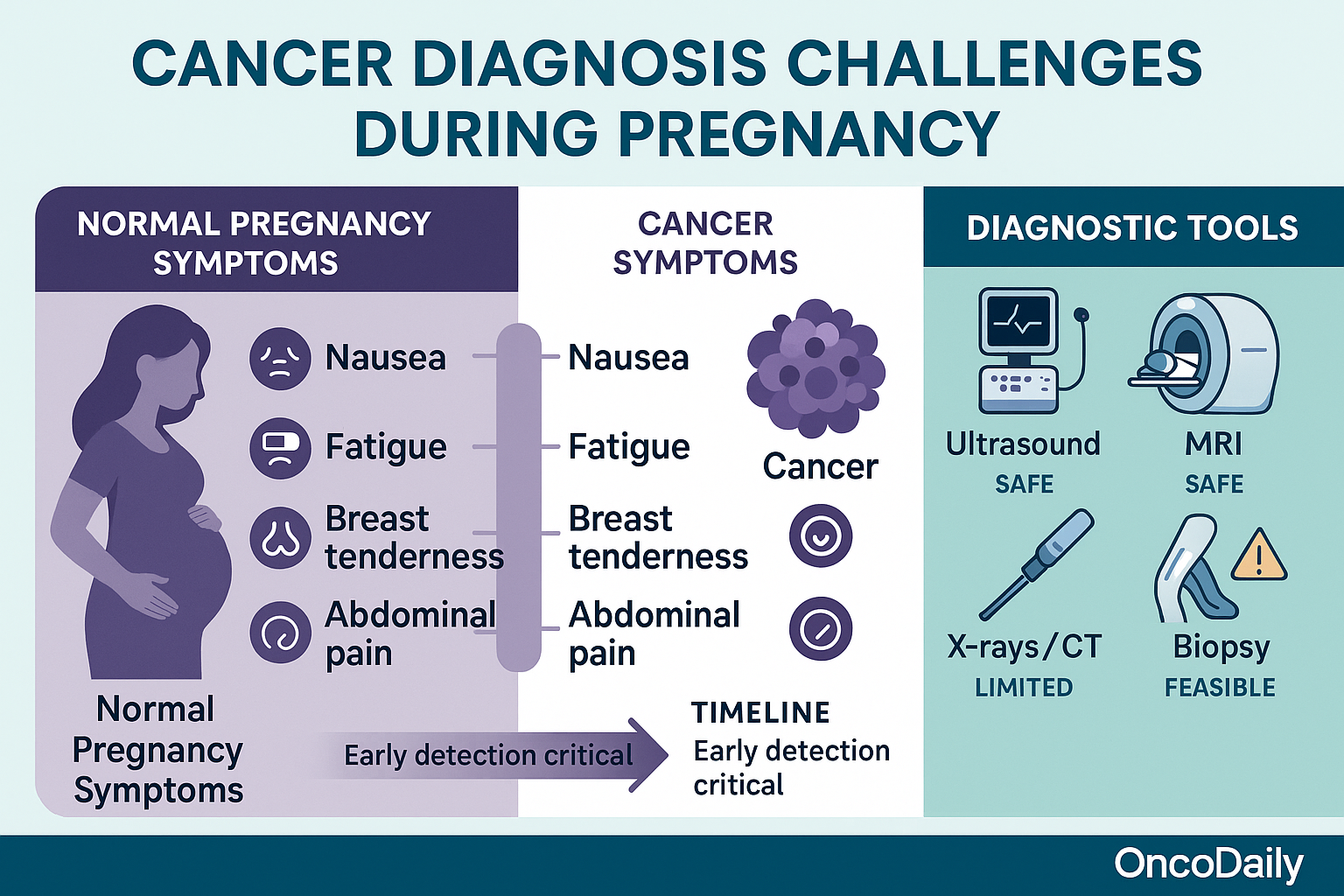
Regarding diagnostic tools, ultrasound is the safest and most commonly used imaging modality during pregnancy, effectively aiding in detecting cancers such as breast and thyroid tumors without exposing the fetus to radiation. Magnetic resonance imaging (MRI) is also considered safe, particularly after the first trimester, since it does not involve ionizing radiation; however, it is generally avoided during early pregnancy unless absolutely necessary.
Use of ionizing radiation, such as X-rays or CT scans, is limited and approached with caution. Low-dose exposure (below 50 mGy) from a single diagnostic procedure is unlikely to harm the fetus, but high-dose imaging, especially abdominal or pelvic CT scans, is avoided during early pregnancy due to potential risks. Nuclear medicine scans (bone scans, PET) have limited safety data and are reserved for critical indications only. Invasive diagnostic procedures like fine needle aspiration or biopsy are feasible and safe during pregnancy when cancer confirmation is needed.
Cancer Surgery During Pregnancy
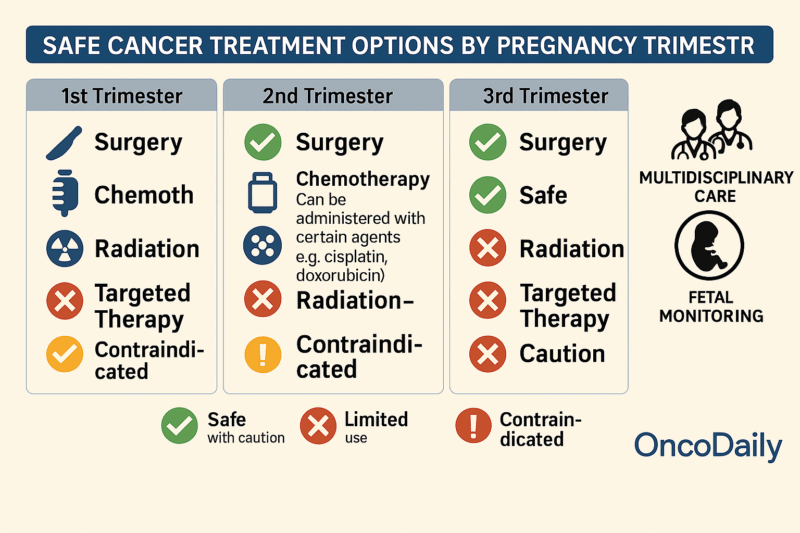
Surgery can be safely performed during all trimesters of pregnancy. Common cancer surgeries, including breast surgery (mastectomy, lumpectomy), biopsies, and intra-abdominal procedures, are feasible during pregnancy with multidisciplinary team involvement.
Timing Considerations by Trimester
The early second trimester is generally considered the optimal time for surgery, especially for intra-abdominal procedures. This timing balances the technical challenge of operating around the enlarging uterus and lowers miscarriage risks associated with first-trimester surgery. Surgery during the first trimester carries a slightly increased risk of miscarriage, while surgeries late in the third trimester may increase risks of preterm labor.
Postoperative Monitoring with Fetal Heart Rate Tracking and Obstetric Support
Postoperative monitoring with fetal heart rate tracking and obstetric support is recommended after viability; tocolytics may be considered if uterine manipulation occurred. Surgery during pregnancy is associated with a higher risk of preterm delivery, so risks must be discussed thoroughly with the patient. Locoregional anesthesia is preferred when feasible to minimize fetal exposure to anesthesia. Venous thromboembolism prophylaxis with low molecular weight heparin is critical due to the prothrombotic state of pregnancy, immobility, and cancer. Surgical treatment can control maternal cancer effectively while minimizing fetal risk if timed and managed properly.
Chemotherapy During Pregnancy
Chemotherapy is contraindicated during the first trimester due to high teratogenic risk when organogenesis occurs. It can be safely administered during the second and third trimesters (after 12-14 weeks gestation), continuing until about 1-3 weeks before expected delivery. Timing is crucial to avoid fetal myelosuppression close to birth and to reduce neonatal complications.
Agents Considered Safe
Several agents such as cisplatin and doxorubicin have been used without significant adverse fetal outcomes when administered in the second and third trimesters. Regimens are often adapted to exclude drugs with known strong teratogenicity or lacking safety data. Hormone therapies and most targeted agents are generally avoided during pregnancy due to insufficient safety data.
Impact on Fetal Development and Pregnancy Outcomes:
Exposure to chemotherapy in the 2nd/3rd trimester has been linked to some increased risks of low birth weight and prematurity but generally not to congenital malformations. Long-term developmental outcomes in exposed children appear reassuring in limited studies but require further research.
Monitoring and Obstetric Follow-up:
Pregnant patients receiving chemotherapy require close prenatal monitoring for fetal growth, cardiac function, and hematologic status. Multidisciplinary teams, including oncologists and maternal-fetal medicine specialists, coordinate ongoing care.
Radiation Therapy During Pregnancy
Pelvic or abdominal radiation is absolutely contraindicated during pregnancy due to high fetal radiation exposure and risk of severe fetal harm or death. Radiation to areas remote from the fetus (e.g., head, neck, extremities) might be considered in exceptional cases with rigorous fetal shielding and dose limitation.
Potential Fetal Harm vs. Maternal Benefit
The cumulative fetal radiation dose should ideally not exceed 100 mGy to minimize the risk of fetal malformations and neurodevelopmental harm. Early pregnancy radiation carries higher fetal risk; later pregnancy exposure risks include growth restriction and cognitive deficits. Decisions must weigh urgent maternal indications against accurate assessment and minimization of fetal risks in a multidisciplinary setting.
Alternative Management Strategies
Surgery and chemotherapy are preferred over radiation when possible during pregnancy. Postponing radiation therapy until after delivery is common when clinically feasible. The use of advanced radiation techniques and shielding can reduce fetal dose if radiation is unavoidable.
Targeted Therapies and Immunotherapies During Pregnancy
Data on the safety of targeted therapies (e.g., tyrosine kinase inhibitors) and immunotherapies (e.g., checkpoint inhibitors) during pregnancy is very limited. Most targeted agents are contraindicated due to their mechanism and lack of well-established fetal safety data. Immunotherapies pose unclear risks as they modulate immune response, potentially affecting fetal-maternal tolerance.
Recommendations from Recent Guidelines
Current clinical guidelines generally recommend against the use of targeted and immunotherapies during pregnancy outside of life-threatening situations with no alternatives. When urgent treatment with these agents is needed, it should be managed in specialized centers with multidisciplinary consultation, ideally in clinical trials or registries to accrue data. Counseling patients about risks and potential unknowns is essential.
Summary of Cancer Management During Pregnancy
Surgery can be safely performed at any trimester with a preference for the early second trimester for intra-abdominal cases. Chemotherapy is contraindicated in the first trimester but relatively safe after organogenesis is complete; agents like cisplatin and doxorubicin have the most evidence. Radiation in the pelvis/abdomen is contraindicated, but limited upper-body radiation may be possible with precautions. Targeted therapies and immunotherapies lack sufficient safety data and are usually avoided during pregnancy. Multidisciplinary management with oncology, obstetric, neonatal, radiology, and anesthesia teams is critical to balancing maternal cancer control and fetal safety.
How Should Cancer Be Managed During Pregnancy to Protect Both Mother and Baby?
Management of cancer during pregnancy demands an individualized approach that carefully integrates obstetric and oncologic care. A multidisciplinary team is essential, bringing together experts in medical oncology, maternal-fetal medicine, neonatology, anesthesia, and surgery, all working collaboratively to optimize outcomes for both mother and fetus . Treatment plans are personalized according to the cancer’s type and stage, the gestational age, the patient’s overall health, and her preferences. Throughout pregnancy, continuous reassessment is crucial to adapt the treatment schedule as necessary, balancing the urgency of controlling maternal cancer with minimizing risks to fetal development .
Fertility preservation must be addressed proactively before initiating any gonadotoxic therapies. While procedures such as ovarian tissue cryopreservation or oocyte/embryo freezing are more challenging during pregnancy, they may be feasible in select cases. Use of gonadotropin-releasing hormone (GnRH) analogs to reduce ovarian toxicity during chemotherapy is supported by emerging evidence but requires careful consideration and further study . Counseling should include clear discussions about long-term reproductive health and family planning after treatment to aid informed patient decisions .
Psychological support plays a vital role given the dual stress of pregnancy and cancer diagnosis. Prompt access to psycho-oncology services, counseling, and social supports can alleviate anxiety, depression, and uncertainty. Involving family members in the support process helps improve coping and shared decision-making . Multidisciplinary psychosocial care should be integrated into routine management.
Timing and mode of delivery are carefully planned, aiming to prolong pregnancy until at least 37 weeks to reduce prematurity-associated complications . Delivery timing may sometimes be advanced to allow initiation or completion of therapies that are contraindicated in pregnancy. Vaginal delivery remains the preferred mode for most cancer types, unless obstetric indications or specific tumor locations (e.g., invasive cervical cancer) dictate cesarean section, which is reserved for maternal or fetal safety considerations . Helen Bolton, Obstetrics, Gynaecology & Reproductive Medicine 2025
Regarding breastfeeding, chemotherapy generally contraindicates lactation because cytotoxic agents pass into breastmilk and risk infant toxicity; breastfeeding is typically resumed after an appropriate drug-specific washout period post-therapy . The safety profile for many targeted therapies and immunotherapies during lactation remains insufficiently understood, necessitating cautious avoidance until further data emerge . Patients undergoing surgery without ongoing contraindicated treatments may breastfeed once adequately recovered. Lactation support and counseling are vital to ensure safe breastfeeding practices and infant health monitoring . Cynthia Maxwell Gynecology and Obscetrics 2025
These evidence-based management principles are reflected in international consensus guidelines and best practice recommendations from FIGO, ASCO, ESMO, and other expert bodies, emphasizing multidisciplinary, patient-centered care to safeguard both maternal prognosis and fetal well-being .
Multidisciplinary Care and Monitoring
The management of cancer during pregnancy necessitates close collaboration among a multidisciplinary team composed of oncology specialists, maternal-fetal medicine experts, obstetricians, pediatricians, and other healthcare professionals to optimize outcomes for both mother and fetus. This team approach is essential due to the complex interplay between cancer diagnosis and treatment and the unique physiologic and developmental stages of pregnancy. The multidisciplinary team coordinates to harmonize diagnostic methods, assess the tumor characteristics, and formulate individualized treatment plans that balance maternal therapeutic needs with fetal safety. This collaboration includes ongoing communication with the patient and her family to inform decision-making that respects medical, ethical, and personal considerations.
Specialized obstetricians within this team play a critical role in monitoring the fetus throughout the pregnancy, ensuring close prenatal surveillance to detect and manage any treatment-related maternal or fetal toxicities. This prenatal monitoring might include frequent ultrasounds, fetal growth assessments, and other specialized tests to evaluate the impact of anticancer therapies on fetal development. The involvement of pediatricians and neonatologists from early on prepares the clinical team for immediate and long-term care of the newborn, should any complications arise due to in utero exposure to cancer treatments.
Furthermore, the team carefully plans the timing and method of delivery to maximize the health outcomes for both mother and child. Delivery is preferably scheduled after 37 weeks of gestation to reduce risks associated with preterm birth unless obstetric or oncologic indications necessitate earlier intervention. Vaginal delivery is generally preferred unless specific clinical scenarios or complications warrant cesarean section. The comprehensive planning also includes postpartum considerations, such as breastfeeding guidance and neonatal monitoring for potential toxicities from in utero exposure to chemotherapy or other treatments. A Cubillo Clin Transl Oncol. 2020, Lone Storgaard Review Acta Obstet Gynecol Scand . 2024, A Cubillo, Clin Transl Oncol . 2021

Jan Van Eyck, The Arnolfini Portrait, 1434, National Gallery, London, UK.
What Are the Maternal and Fetal Outcomes of Cancer Treatment During Pregnancy?
Evidence shows that many cancers can be treated safely during pregnancy, especially when treatments such as chemotherapy are administered after the first trimester. Studies indicate that chemotherapy during the second and third trimesters is generally feasible and does not significantly affect fetal mortality or early childhood cognitive or physical development. For instance, a multi-center prospective study found that chemotherapy reduced maternal mortality without impairing children’s mortality rates or developmental outcomes measured by standardized assessments. Long-term studies also show no substantial increase in central nervous system, cardiac, auditory, or general health impairments in children exposed to chemotherapy in utero beyond the early first trimester. Zhang YP, J Cancer. 2019
However, cancer during pregnancy is associated with increased risks such as preterm birth and low birth weight. These adverse outcomes are mainly due to the illness itself or timing and intensity of treatment. Preterm labor and premature delivery are common complications managed by high-risk obstetric care, which focuses on close fetal monitoring and carefully planning the timing of delivery to balance fetal maturity with the need for maternal cancer treatment. Cesarean section rates tend to be higher among pregnant women with cancer. Despite these risks, neonatal outcomes are generally favorable when treatment is planned and timed properly. Intrauterine growth restriction and stillbirth risk are also elevated particularly with first-trimester chemotherapy exposure and thus intensified prenatal surveillance is required.
Regarding postpartum care, breastfeeding considerations depend largely on the cancer treatment received. Chemotherapy and other systemic treatments often contraindicate breastfeeding due to drug excretion in breast milk, but this varies by agent and timing. Pediatric and maternal oncology teams guide individualized recommendations balancing treatment continuation and benefits of breastfeeding.
What Support and Resources Are Available for Patients Diagnosed With Cancer During Pregnancy?
Support and resources are vital for women diagnosed with cancer during pregnancy, as they face unique psychological, social, and medical challenges. Psychological and social support options often include specialized charities and patient networks such as Hope for Two and Mummy’s Star, which connect pregnant cancer patients with others who have experienced similar situations. This peer-to-peer support can provide emotional reassurance and reduce feelings of isolation by sharing survivor stories and practical advice. Additionally, many cancer centers provide access to counselors, psychologists, and chaplaincy services to address the emotional burdens that arise from coping with both pregnancy and cancer simultaneously.
Access to specialized care centers with multidisciplinary teams experienced in managing cancer during pregnancy is also essential. These teams typically include oncologists, maternal-fetal medicine specialists, obstetricians, and pediatricians working collaboratively to devise individualized treatment and monitoring plans. Such centers offer comprehensive care that integrates both maternal cancer treatment and fetal well-being, ensuring safe and effective management throughout pregnancy. Patients are often referred promptly to these centers where educators and nurse liaisons help guide treatment decisions and support needs, emphasizing clear communication and shared decision-making.
Legal and ethical considerations also play a crucial role, especially when treatment decisions may impact pregnancy continuation. Patients may face difficult choices regarding therapy timing and whether to carry the pregnancy to term. Multidisciplinary teams provide counseling to help women understand their options, respecting patient autonomy while considering medical advice. Some organizations assist with navigating these decisions by offering clear information about risks, treatment safety, and rights relating to pregnancy and cancer care.
Overall, a comprehensive network of psychological support, expert multidisciplinary care, and informed counseling forms the backbone of resources available for pregnant women facing cancer, helping them navigate complex medical and emotional challenges while striving for the best possible outcomes for themselves and their babies.
Have Any Celebrities Been Diagnosed with Cancer During Pregnancy or Around Childbirth?
Several celebrities have faced cancer diagnoses during pregnancy or very close to childbirth, highlighting the challenges of managing cancer while expecting a baby. Maria Menounos was diagnosed with stage 2 pancreatic neuroendocrine tumor shortly before the birth of her child and has since become an advocate for early cancer detection. Stephanie Schmidt, a neonatal nurse, discovered she had breast cancer at eight weeks pregnant during a routine prenatal visit, confronting difficult treatment decisions while managing pregnancy. Laura Hudson learned she had stage 2 breast cancer at 36 weeks pregnant and delivered her daughter via emergency cesarean section before starting chemotherapy.
Lydia Dutcher was diagnosed with a rare type of cancer called choriocarcinoma shortly after giving birth, receiving chemotherapy while her newborn remained healthy. Michelle Hughes experienced pregnancy-related pain late in gestation, initially attributed to common pregnancy symptoms, but was later found to have terminal cancer years afterward. These stories reflect the complexity and emotional impact of cancer during pregnancy, as well as the importance of multidisciplinary care and support systems for affected women.
Written by Aharon Tsaturyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
