Glioblastoma Cure Rate: What Patients Should Know
Glioblastoma (GBM) is one of the most aggressive forms of brain cancer, often diagnosed in individuals over 50, although it can occur at any age. The tumor is notorious for its rapid growth, resistance to treatment, and high recurrence rate, leading to poor long-term survival outcomes. This article explores what the glioblastoma cure rate is, how it varies by stage, and the treatment options that can improve outcomes.
How Common Is Glioblastoma?
Glioblastoma is the most common and deadly type of malignant primary brain tumor in adults. According to the American Brain Tumor Association, there are approximately 12,000 new cases of glioblastoma diagnosed annually in the United States alone. The disease is more prevalent in older adults, and males are generally at higher risk than females.
Despite its frequency, the survival rate remains low due to its invasive nature, where tumor cells infiltrate surrounding healthy brain tissue, making surgical removal difficult.
Read About Glioblastoma on Oncodaily
What Does “Cure” Mean in Glioblastoma?
Glioblastoma is typically considered incurable due to its aggressive growth and resistance to most treatments. However, treatment can sometimes extend survival, improve quality of life, and reduce tumor burden. The goal of therapy is maximal tumor reduction through surgery, followed by radiotherapy and chemotherapy to delay recurrence.
The glioblastoma cure rate is low, with most patients experiencing a recurrence within 6-12 months of treatment. Nonetheless, with advances in targeted therapies and immunotherapies, survival rates are improving, especially for younger, healthier patients who are diagnosed at an earlier stage.
What Is the Glioblastoma Cure Rate by Stage?
Early-Stage Glioblastoma (Before Spread)
In the early stages of glioblastoma, surgery is often the first line of treatment. The goal is to remove as much of the tumor as possible. Although complete removal is challenging due to the tumor’s tendency to infiltrate surrounding brain tissue, maximal safe resection can lead to better outcomes.
The 5-year survival rate for patients with newly diagnosed glioblastoma is around 15-20%. This is a significant improvement over previous decades, thanks to the use of adjuvant radiotherapy and temozolomide chemotherapy, which help to control the tumor.
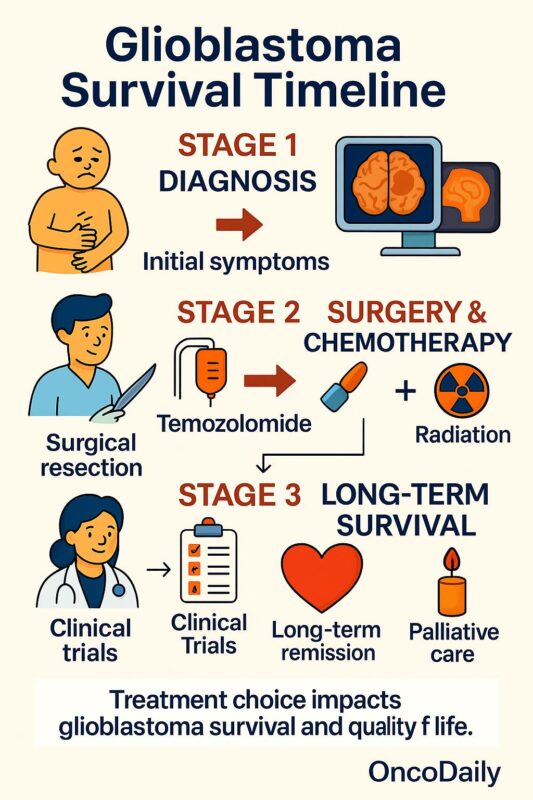
Advanced Glioblastoma (After Spread or Recurrence)
Once glioblastoma has recurred or metastasized, the prognosis worsens. The 5-year survival rate drops significantly, with some studies reporting survival as low as 5% for patients with recurrent glioblastoma. At this stage, treatment options are more limited, and outcomes are generally poorer, as the tumor becomes increasingly resistant to therapies.
Treatment for advanced glioblastoma typically includes chemotherapy (e.g., temozolomide) along with targeted therapies and immunotherapies aimed at shrinking or controlling tumor growth, but these are less likely to achieve a cure.
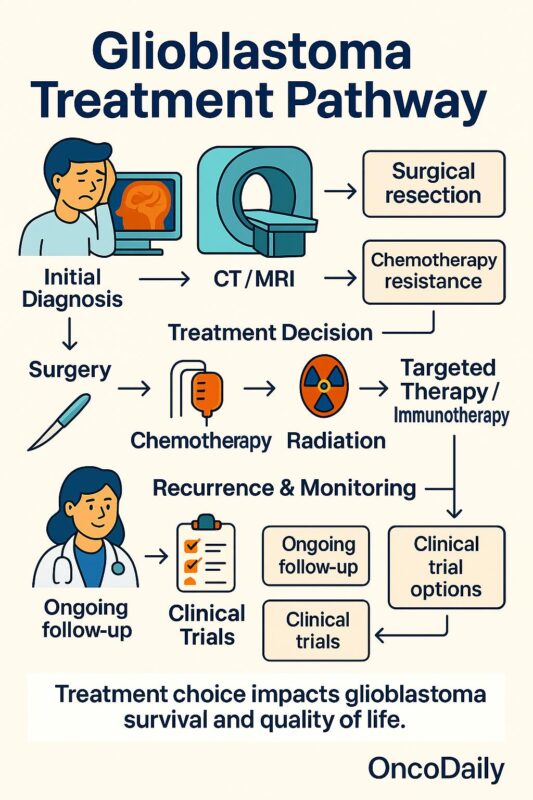
Which Treatments Offer the Best Chance of Survival?
Surgical Resection
Surgery remains the first-line treatment for glioblastoma, aiming to remove as much of the tumor as safely possible. While complete resection is often not achievable, a partial resection that reduces tumor mass can provide significant relief and improve survival outcomes.
Radiotherapy
After surgery, radiotherapy is used to target residual tumor cells that may not be visible or accessible for surgical removal. Standard treatment typically involves fractionated external beam radiation therapy (EBRT), delivered over a period of several weeks.
Chemotherapy
Temozolomide, an oral chemotherapy drug, is commonly used after surgery and radiotherapy to kill remaining cancer cells. Temozolomide works by interfering with the tumor cells’ DNA repair mechanisms. Though it can extend survival, it does not provide a cure.
Targeted Therapy and Immunotherapy
Despite standard treatments like surgery, radiation, and temozolomide chemotherapy, glioblastoma remains difficult to cure. This has led to growing interest in targeted therapies and immunotherapy, which aim to treat the disease more precisely.
Targeted therapy focuses on blocking specific molecular pathways that fuel tumor growth. One of the best-known examples is bevacizumab, which targets VEGF to reduce blood vessel formation in tumors. While it may ease symptoms and slow progression, it hasn’t significantly extended survival in newly diagnosed patients. Efforts to target EGFR mutations—common in glioblastoma—have been less successful due to resistance and poor drug delivery across the blood-brain barrier.
A more promising area is IDH-mutant glioblastoma. Though rare, these tumors are biologically distinct and linked to slower progression and better prognosis. Patients with IDH1 or IDH2 mutations may benefit from targeted drugs like ivosidenib, which blocks the mutant enzyme’s activity. These treatments are still under investigation but represent an important step toward personalized care.
Meanwhile, immunotherapy—which has revolutionized treatment for other cancers—has faced more obstacles in glioblastoma. Immune checkpoint inhibitors such as nivolumab have not shown major benefits in large trials, partly due to the tumor’s immune-suppressive environment. Researchers are now exploring combinations of immunotherapy with radiation, vaccines, and even CAR T-cell therapies to improve results.
While these novel approaches are still evolving, they bring hope for more effective and personalized glioblastoma treatment strategies in the near future.
What Factors Influence the Glioblastoma Cure Rate?
Several key factors influence survival outcomes and the potential for cure in glioblastoma patients:
- Age and general health: Younger patients with fewer comorbidities generally have better outcomes and are more likely to tolerate aggressive treatments.
- Tumor location: Tumors located in areas that are surgically accessible tend to have better outcomes than those located in critical areas of the brain.
- Extent of resection: The more tumor that can be safely removed during surgery, the better the chances of survival and recurrence control.
- Molecular markers: Certain genetic and molecular markers, such as MGMT methylation status, can predict how well the tumor will respond to chemotherapy, influencing survival.
- Recurrence patterns: Glioblastoma is known for its high recurrence rate. Patients whose tumors respond well to initial treatment may achieve longer survival, but recurrence is common.
What’s the Outlook for Glioblastoma Patients?
The overall prognosis for glioblastoma remains challenging, with a median survival rate of 15 to 18 months following diagnosis. While the glioblastoma cure rate remains low, treatments are improving, and patients can often achieve long periods of disease control, especially with cutting-edge therapies and clinical trials.
Emerging treatments such as gene therapy, targeted therapies, and immunotherapies hold promise for the future, offering hope for patients who might otherwise have limited treatment options.
You Can Watch More on OncoDaily Youtube TV
Written by Armen Gevorgyan, MD
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
