Childhood Cancer in Pakistan: Factors Driving Treatment Abandonment at a Tertiary Center
Childhood cancer survival exceeds 80% in high-income countries but is often below 30% in low- and middle-income countries, around 20% in Pakistan, mainly due to treatment abandonment. Barriers include financial hardship, long travel, limited caregiver education, and fear of side effects. Addressing abandonment is key to the WHO goal of 60% global survival by 2030. A 2024 cohort study at PIMS Islamabad identifies social, clinical, and system-level factors, offering insights to improve adherence and narrow the survival gap.
Title: Identifying the Factors Contributing to Treatment Abandonment in Childhood Cancers at a Tertiary Care Hospital in Pakistan
Authors: Muhammad Wasim Khan, Ruqayya Manzoor, Nuzhat Yasmeen, Hijab Shaheen, Junaid Jamshed, Nazia Rafique
Background
Treatment abandonment is one of the main reasons for poor pediatric cancer outcomes in Pakistan, where survival rates remain as low as 20%. In this context, abandonment refers to failure to start or continue therapy for four or more consecutive weeks without valid medical justification. Previous reports from Karachi showed abandonment rates above 22%, with factors such as long travel distances, low maternal education, and financial difficulties playing central roles. The current study builds on this evidence by prospectively examining socioeconomic, geographic, and treatment-related contributors to abandonment at a tertiary care hospital in Islamabad.
Methods
This prospective cohort study was conducted at the Pediatric Oncology Department of PIMS Children’s Hospital in Islamabad over a one-year period in 2024. A total of 104 children younger than 14 years with newly diagnosed cancers were included, while cases of relapse, palliative-only referrals, or incomplete records were excluded. Caregivers were interviewed at diagnosis, and each child was followed for six months to assess whether treatment was continued or abandoned.
- Baseline interviews: collected information on demographics, socioeconomic status, maternal education, cancer type, and caregiver perceptions of treatment.
- Follow-up process: children were monitored during routine clinic visits and through telephone calls. Families missing visits were contacted up to three times at weekly intervals.
- Definition of abandonment: failure to start or continue curative treatment for four or more consecutive weeks, following SIOP guidelines.
- Abandonment interviews: families of children who discontinued therapy were asked about the reasons, which were grouped into financial strain, travel barriers, treatment side effects, use of alternative care, disease progression, or cultural factors.
This approach allowed the researchers to capture both quantitative data on the frequency of abandonment and qualitative insights into the challenges faced by families during treatment.
Results
Out of 104 children enrolled, 18 (17.3%) abandoned therapy, and 86 (82.7%) completed treatment. The mean age was 6.2 years; 60.6% were male, and two-thirds lived in rural areas. Most mothers (66.3%) had no formal education, and 73.1% of families earned less than 30,000 PKR per month. Treatment expenses were self-funded in nearly half of the cases, with the rest partially or fully subsidized.
Leukemia was the most common diagnosis (42.3%), followed by lymphoma (23.1%) and solid tumors (20.2%). Treatment-related side effects were reported in 31.7% of patients. Lower maternal education and the presence of toxicities were significantly associated with abandonment (p<0.05). Other variables, including age, sex, income, and residence, showed no statistical significance, though a trend toward higher compliance in males and higher abandonment in poorer households was noted.
Caregiver perceptions were generally positive: 63.4% found treatment well tolerated, 66.3% believed it was highly effective, and 93.3% rated provider communication as clear. Still, logistical burdens were heavy; 60.6% traveled more than 50 km, 82.7% required weekly visits, 91.3% relied on public transport, and nearly half spent 1,000–2,500 PKR weekly on travel.
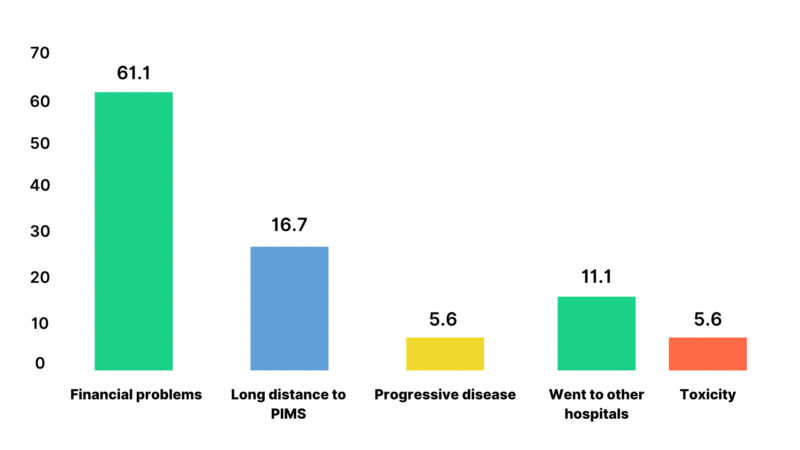
Reported Reasons for Treatment Abandonment
Khan MW, Manzoor R, Yasmeen N, Shaheen H, Jamshed J, Rafique N. Identifying the factors contributing to treatment abandonment in childhood cancers at a tertiary care hospital in Pakistan. Original Research: Pediatric Oncology. 2025 Aug 31. doi:10.69690/ODMJ-001-0829-4568.
Key Findings
- Abandonment rate of 17.3% highlights ongoing challenges despite some improvements compared with earlier Pakistani studies reporting >20%.
- Financial strain is the most consistent driver, encompassing both medical and indirect costs like travel and lodging.
- Distance and frequent hospital visits amplify burden, especially for rural families without private transport
- Low maternal education is an independent predictor, underscoring the need for caregiver literacy programs.
- Toxicities double the risk of abandonment, reflecting gaps in anticipatory counseling and supportive care.
- Positive caregiver perceptions of communication and treatment effectiveness suggest that system-level, not provider-level, barriers drive dropout.
Conclusion
This study shows that treatment abandonment affects nearly one in six children with cancer in Pakistan, driven mainly by financial hardship, long travel, low maternal education, and treatment toxicities. Most caregivers trusted the care provided, pointing to structural barriers rather than dissatisfaction as the cause of dropout. Solutions must include stronger financial support covering indirect costs, decentralization of services, early caregiver education on side effects, and close follow-up in the first months of therapy. Narrowing the survival gap in LMICs will require addressing these barriers alongside medical progress.
Read the full article here.

Note: The Second Global OncoThon: A Movement of Unity and Action for Pediatric Cancer, organized by OncoDaily and SIOP, is raising funds for pediatric cancer research. The charity is still open, and donations can be made through the official link.
-
Challenging the Status Quo in Colorectal Cancer 2024
December 6-8, 2024
-
ESMO 2024 Congress
September 13-17, 2024
-
ASCO Annual Meeting
May 30 - June 4, 2024
-
Yvonne Award 2024
May 31, 2024
-
OncoThon 2024, Online
Feb. 15, 2024
-
Global Summit on War & Cancer 2023, Online
Dec. 14-16, 2023
